DIAGNOSTIC ACCURACY OF 11C
advertisement

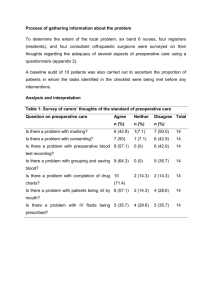
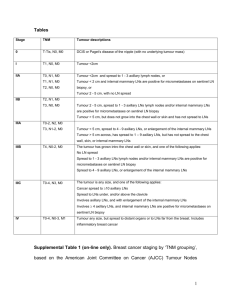
DIAGNOSTIC ACCURACY OF 11C-CHOLINE PET/CT IN COMPARISON WITH CONTRAST-ENHANCED CT IN THE PREOPERATIVE LYMPH-NODE STAGING OF BLADDER CANCER USING THE PATHOLOGICAL SPECIMENS AS REFERENCE STANDARD. Bianchi L1, Borghesi M1, Vagnoni V1, Pultrone C1, Gentile G1, Cevenini M1, Ceci F2, Giampaoli M1, Chessa F1, Passaretti G1, Brunocilla E1, Fanti S2, Martorana G1, R. Schiavina1 1 Department of Urology, Alma Mater Studiorum University of Bologna, Bologna, Italy 2 Department of Nuclear Medicine, Alma Mater Studiorum University of Bologna, Bologna, Italy Aim: Current imaging techniques, such as contrast enhanced computed tomography (CE-CT) and magnetic resonance imaging (MRI), which provide only morphologic information, demonstrated to be not adequately accurate in the preoperative nodal staging of bladder cancer (BC). 11 C-Choline has been proposed as a potential tracer for visualization of BC. First clinical trials showed controversial results, even if the series available in literature are still limited. The aim of this study was to evaluate the role of 11C-Choline-PET/CT in preoperative evaluation of nodal involvement of BC patients suitable for radical cystectomy and ePLND in comparison with CE-CT using the pathological specimen as reference standard. Methods and materials: 78 consecutive patients with histologically proven BC, suitable for radical cystectomy and extended pelvic lymph node dissection (ePLND), were enrolled from April 2011 to January 2014. In all patients pelvic lymph nodes were dissected up to the origin of the inferior mesentery artery. The areas of the LN dissection were grouped as follow: region A included preaaortic and precaval LNs; region B included paravescical, common, internal and external iliac, obturatory, presacral LNs in the right pelvis; region C included paravescical, common, internal and external iliac, obturatory, presacral LNs in the left pelvis. 11 C-Choline-PET/CT and abdominal CE-CT were used to assess the presence of lymph node metastases on a patient-, region- and LN-based analysis, using results of surgical specimens as diagnostic gold standard. Results: The mean age was 68.9±9.2 years. 24 of 78 (30%) patients showed nodal metastases at pathological analysis. Overall, 2350 LNs were evaluated and 154 LNs (6.5%) showed metastatic involvement. Detection rates and comparisons of 11C-Choline-PET/CT and CE-CT according to the patient-, region- and LN-based analysis are showed in Table 1. Finally, the detection rate (DR) of 11C-Choline-PET/CT and abdominal CE-CT were calculated for three different ranges of diameter of the metastatic deposit (<5 mm, 5-10 mm and >10 mm): 11C-Choline-PET/CT was superior than CE-CT in all the ranges evaluated and was able to detect nodal metastasis even with small (<10mm). Discussion: In BC, lymph node involvement is critical for prognostic and therapeutic reasons. In literature few data are available about the accuracy of 11C-Choline-PET/CT in BC. In our study, 11C-Choline-PET/CT was more accurate than CE-CT in the LN evaluation of BC: on patient based analysis and on lymph node analysis 11 C-Choline-PET/CT showed a better sensitivity, PPV, NPV than CE-CT. Conclusion: 11 C-Choline-PET/CT could provide additional diagnostic information in preoperative nodal staging of patients with BC in comparison with CE-CT. A study with a larger population should determine if 11 C-Choline-PET/CT could be recommended as routine technique in high risk patient with BC.