Because of a particular pharmaceutical solution's use, it may be
advertisement

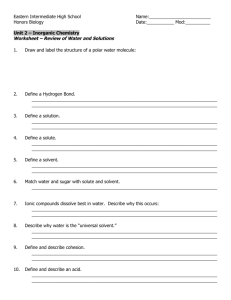
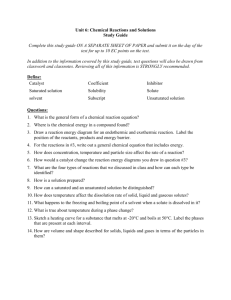
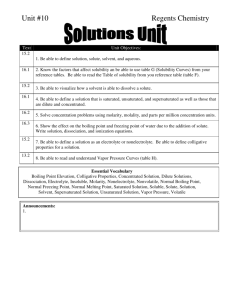
12. Solutions Contents 1. Solubility 2. Some Solvents for Liquid Preparations 3. Preparation of Solutions 4. Oral Solutions and Preparations for Oral Solution 5. Syrups 6. Elixirs 7. Tinctures 8. Proper Administration and Use of Liquid Peroral Dosage Forms 9. Topical Solutions and Tinctures 10. Vaginal and Rectal Solutions 11. Topical Tinctures 12. Topical Oral (Dental) Solutions 13. Miscellaneous Solutions 14. Nonaqueous Solutions 15. Extraction Methods for Preparing Solutions - - In pharmaceutical terms, solutions are “liquid preparations that contain one or more chemical substances dissolved in a suitable solvent or mixture of mutually miscible solvents”. Because of a particular pharmaceutical solution’s use, it may be classified as oral solution, otic solution, ophthalmic solution, topical solution. Solutions, because of their composition or use, may be classified as other pharmaceutical dosage forms. Syrups Elixirs Spirits Tinctures Certain solutions prepared to be sterile and pyrogen-free and intended for parenteral administration are classified as injections. Oral solutions, syrups, elixirs, spirits, and tinctures are prepared and used for the specific effects of the medicinal agents they carry. In these preparations, the medicinal agents are intended to provide systemic effects. 1. Solubility When molecules interact, attractive and repulsive forces are in effect. When the attractive and repulsive forces are equal, the potential energy between two molecules is minimum and the system is most stable. When a solute dissolves, the substance’s intermolecular forces of attraction must be overcome by forces of attraction between the solute and solvent molecules. This entails breaking the solute-solute forces and the solvent-solvent forces to achieve the solute-solvent attraction. The solubility of an agent in a particular solvent indicates the maximum concentration to which a solution may be prepared with that agent and that solvent. When a solvent at a given temperature has dissolved all of the solute it can, it is said to be saturated. Through selection of a different solubilizing agent or a different chemical salt form of the medicinal agent, alteration of the pH of a solution, or substitution in part or in whole of the solvent, a pharmacist can in certain instances dissolve greater quantities of a solute than would otherwise be possible. Temperature is an important factor in determining the solubility of a drug and in preparing its solution. Most chemicals absorb heat when they are dissolved and are said to have a positive heat of solution, resulting in increased solubility with a rise in temperature. A few chemicals have a negative heat of solution and exhibit a decrease in solubility with a rise in temperature. Other factors including the various chemical and other physical properties of both the solute and the solvent, pressure, the pH of the solution, the state of subdivision of the solute, and the physical agitation applied to the solution as it dissolves affect solubility. The solubility of a substance in a given solvent may be determined by preparing a saturated solution of it at a specific temperature, and determining by chemical analysis the amount of chemical dissolved in a given weight of solution. The solubility may be expressed as grams of solute dissolving in milliliters of solvent. When the exact solubility has not been determined, general expressions of relative solubility may be used. These terms are defined in the USP and presented in Table 12.1 A great many of the important organic medicinal agents are either weak acids or weak bases, and their solubility depends to a large measure on the pH of the solvent. These drugs react either with strong acids or strong bases to form water-soluble salts. Table 12.2 presents the comparative solubilities of some typical examples of weak acids and weak bases and their salts. Commonly, salts of organic compounds are more soluble in water than are the corresponding organic bases. Conversely, the organic bases are more soluble in organic solvents than the corresponding salt forms. In most instances, especially for solutions to be taken orally, used ophthalmically, or injected, water is the preferred solvent. When water is used as the primary solvent, commonly an auxiliary solvent is also employed to augment the solvent action of water or to contribute to a product’s chemical or physical stability. Alcohol, glycerin, and propylene glycol, have been quite effective in contributing to the desired characteristics of pharmaceutical solutions and in maintaining their stability. A number of fixed oils, such as corn oil, cottonseed oil, peanut oil, and sesame oil, are useful solvents, particularly in the preparation of oleaginous injections, and are recognized in the official compendia for this purpose. 2. Some Solvents for Liquid Preparations (1) Alcohol, USP: Ethyl Alcohol, Ethanol (2) Diluted Alcohol, NF (3) Alcohol, Rubbing (4) Glycerin, USP (Glycerol) (5) Isopropyl Rubbing Alcohol (6) Propylene Glycol, USP (7) Purified Water, USP (1) Alcohol, USP: Ethyl Alcohol, Ethanol Alcohol is the most useful solvent in pharmacy next to water. USP, is 94.9 to 96% C2H5OH by volume (i.e., v/v) Together with water it forms a hydroalcoholic mixture that dissolves both alcohol-soluble and water-soluble substances, a feature especially useful in the extraction of active constituents from crude drugs. Alcohol has been well recognized as a solvent and excipient in the formulation of oral pharmaceutical products. Certain drugs are insoluble in water and must be dissolved in an alternative vehicle. Alcohol is frequently used with other solvents, such as glycols and glycerin, to reduce the amount of alcohol required. It also is used in liquid products as an antimicrobial preservative alone or with parabens, benzoates, sorbates, and other agents. However, concern has been expressed over the undesired pharmacologic and potential toxic effects of alcohol. OTC Children under 6 years of age 6-12 years of age Over 12 years of age and adults alcohol limit 0.5% 5% 10% (2) Diluted Alcohol, NF Diluted Alcohol, NF, is prepared by mixing equal volumes of Alcohol, USP, and Purified Water, USP. The strength of Diluted Alcohol, NF, is not exactly half that of the more concentrated alcohol but slightly greater, approximately 49%. Diluted alcohol is a useful hydroalcoholic solvent in various pharmaceutical processes and preparations. (3) Alcohol, Rubbing Rubbing alcohol contains about 70% ethyl alcohol by volume, the remainder consisting of water, denaturants with or without color additives and perfume oils, and stabilizers. 100 ml Sucrose octaacetate (蔗糖八乙酸酯) 355 mg or (denatonium benzoate 地那铵苯甲酸盐 1.4 mg) denaturants 8 parts acetone 1.5 parts methyl isobutyl ketone 100 parts ethyl alcohol It is employed as a rubefacient externally and as a soothing rub for bedridden patients, a germicide for instruments, and a skin cleanser prior to injection. It also used as a vehicle for topical preparations. The product is volatile and flammable and should be stored in tight containers remote from fire. (4) Glycerin, USP (Glycerol) Glycerin is a clear syrupy liquid with a sweet taste. It is miscible with both water and alcohol. Glycerin has preservative qualities and is often used as a stabilizer and as an auxiliary solvent in conjunction with water or alcohol. It is used in many internal preparations. (5) Isopropyl Rubbing Alcohol Isopropyl rubbing alcohol is about 70% by volume isopropyl alcohol, the remainder consisting of water Commercially with or without color additives, 91% isopropyl alcohol solution stabilizers, and perfume oils. for diabetic patients It is used externally as a disinfecting needles, rubefacient and soothing rub syringes and skin and as a vehicle for topical products. (6) Propylene Glycol, USP Propylene glycol, a viscous liquid, is miscible with water and alcohol. It is a useful solvent with a wide range of applications and is frequently substituted for glycerin in modern pharmaceutical formulations. (7) Purified Water, USP Purified Water, USP, is obtained by distillation, ion exchange treatment, reverse osmosis, or other suitable process. It is prepared from water complying with the federal Environmental Protection Agency with respect to drinking water. Compared with ordinary drinking water, Purified Water, USP is more free of solid impurities. When evaporated to dryness, it must not yield greater than 0.001% of residue (1 mg of total solids per 100 mL of sample evaporated). Purified Water, USP is intended for use in the preparation of aqueous dosage forms, except those intended for parenteral administration (injetions). Distillation Method The first portion of aqueous distillate (about the first 10 to 20%) must be discarded. The last portion of water (about 10% of the original volume of water ) remaining in the distillation apparatus must be discarded and not subjected to further distillation. Ion-exchange method On a large or small scale, the ion-exchange method for the preparation of purified water offers a number of advantages over the distillation method. The ion-exchange process permits ease of operation, minimal maintenance, and a more mobile facility. - - There are mainly two types of resins in column ion-exchange the cation, or acid exchangers, which permit the exchange of the cations in solution with hydrogen ion from the resin the anion, or base exchange resins, which permit the removal of anions. These two processes are successively or simultaneously employed to remove both cations and anions from water. Cation exchange H-Resin + M+ + X- + H2O M-Resin + H+ + X- + H2O (pure) Anion exchange Resin-NH2 + H+ + X- + H2O Resin-NH2HX + H2O (pure) Water purified in this manner is referred to as demineralized or de-ionized water. Reverse osmosis In this process, a pressurized stream of water is passed parallel to the inner side of a filter membrane core. A portion of the feed water permeates the membrane as filtrate. The water that has passed through the system is referred to as the concentrate. The flow in this crossflow system is from a more concentrated to a less concentrated solution-thus the term reverse osmosis. Cross-flow filter membranes can remove particles defined in the range of microfiltration (0.1 to 2 microns, e.g., bacteria) ultrafiltration (0.01 to 0.1 microns, e.g., virus) nanofiltration (0.001 to 0.01 microns, e.g., organic compounds in the molecular weight range of 300 to 1000) reverse osmosis (particles smaller than 0.001 microns) Reverse osmosis removes virtually all virus bacteria pyrogens organic molecules and 9099% of all ions. 3. Preparation of Solutions Most pharmaceutical solutions are unsaturated with solute. Thus the amounts of solute to be dissolved are usually well below the capacity of the volume of solvent employed. The strengths of pharmaceutical preparations are usually expressed in terms of percent strength, expressions of ratio strength may be used. These expressions and examples are shown in Table 12.4. The symbol % used without qualification (as with w/v, v/v, or w/w) means percent weight in volume for solutions or suspensions of solids in liquids; percent weight in volume for solutions of gases in liquids; percent volume in volume for solutions of liquids in liquids; and weight in weight for mixtures of solids and semisolids. To hasten dissolution, a pharmacist may employ one of several techniques, such as applying heat, reducing the particle size of the solute, using a solubilizing agent, or subjecting the ingredients to vigorous agitation. Most chemical agents are more soluble at elevated temperatures than at room temperature or below because an endothermic reaction between the heat to enhance dissolution. In addition to or instead of raising the temperature of the solvent to increase the rate of solution, a pharmacist may choose to decrease the particle size of the solute. Most solutions are prepared by simple mixing of the solutes with the solvent. On an industrial scale, solutions are prepared in large mixing vessels with ports for mechanical stirrers. 4. Oral Solutions and Preparations for Oral Solution Most solutions intended for oral administration contain flavorants and colorants to make the medication more attractive and palatable. When needed, they may also contain stabilizers to maintain the chemical and physical stability of the medicinal agents and preservatives to prevent the growth of microorganisms in the solution. The formulation pharmacist must be wary of chemical interactions between the various components of a solution that may alter the preparation’s stability and/or potency. Liquid pharmaceuticals for oral administration are usually formulated such that the patient receives the usual dose of the medication in a conveniently administered volume, as 5mL, 10mL, or 15mL. (1) Dry Mixtures for Solution A number of medicinal agents, particularly certain antibiotics, have insufficient stability in aqueous solution to meet extended shelf life periods. Commercial manufacturers of these products provide them to the pharmacist in dry powder or granule form for reconstitution with a prescribed amount of purified water immediately before dispensing to the patient. The dry powder mixture contains all of the formulative components, including drug, flavorant, colorant, buffers, and others, except for the solvent. Once reconstituted by the pharmacist, the solution remains stable when stored in the refrigerator for the labeled period, usually 7 to 14 days, depending on the preparation. (2) Oral Solutions The pharmacist shoule be sufficiently knowledgeable about the dispensed product to expertly advise the patient of the proper use, dosage, method of administration and storage of the product. Table 12.5 presents examples of some oral solutions. Knowledge of the solubility and stability characteristics of the medicinal agents and the solvents employed in the commercial products is useful to the pharmacist for informing the patient of the advisability of mixing the solution with juice, milk, or other beverage upon administration. (3) Oral Rehydration Solutions Rapid fluid loss associated with diarrhea can lead to dehydration and ultimately death in some patients, particularly infants. Diarrhea is characterized by an increased frequency of loose, watery stools, and because of the rapid fluid loss, dehydration can be an outcome. During diarrhea, the small intestine secretes far more than the normal amount of fluid and electrolytes, and this simply exceeds the ability of the large intestine to reabsorb it. This fluid loss, which occurs mostly from the body’s extracellular fluid compartment, can lead to a progressive loss of blood volume culminating in hypovolemic shock. Oral rehydration solutions are usually effective in treatment of patients with mild volume depletion, 5 to 10% of body weight. A liter or typical oral rehydration solution contains 45 mEq Na+, 20 mEq K+, 35 mEq Cl-, 30 mEq citrate, and 25 g dextrose. It is important that the user add the specific amount of water needed to prepare the powder forms. (4) Magnesium Citrate Oral Solution Magnesium citrate oral solution is a colorless to slightly yellow, clear, effervescent liquid having a sweet, acidulous taste and a lemon flavor. The solution is employed as a saline cathartic with the citric acid, lemon oil, syrup, carbonation. The solution is prepared by reacting official magnesium carbonate with an excess of citric acid, flavoring and sweetening the solution with lemon oil and syrup, filtering with talc, and then carbonating it by the addition of either potassium or sodium bicarbonate. (5) Oral Colonic Lavage Solution Polyethylene glycol 3350 Sodium sulfate Sodium bicarbonate Sodium chloride Potassium chloride 236.00 g 22.74 g 6.74 g 5.86 g 2.97 g In 4800 ml disposable container The PEG acts as an osmotic agent within the gastrointestinal tract and the balanced electrolyte concentration results in virtually no net absorption or secretion of ions. (6) Sodium Citrate and Citric Acid Oral Solution The solution is administered orally in doses of 10 to 30 ml/4 times. Systemic alkalinization 1 ml aqueous solution 100 mg sodium citrate 67 mg citric acid Uric acid Cystine calculi 5. Syrups Syrups are concentrated aqueous preparations of a sugar or sugar substitute with or without flavoring agents and medicinal substances. Syrups containing flavoring agents but not medicinal substances are called nonmedicated or flavored vehicles (syrups). Medicated syrups sucrose purified water flavoring agents coloring agents therapeutic agent Syrups provided a pleasant means of administering a liquid form of a disagreeable-tasting drug. They are particularly effective in the administration of drugs to youngsters, since their pleasant taste usually dissipates any reluctance on the part of the child to take the medicine. Any water-soluble drug that is stable in aqueous solution may be added to a flavored syrup. However, care must be exercised to ensure compatibility between the drug substance and the other formulative components of the syrup. (1) Components of Syrups Most syrups contain the following components in addition to the purified water and any medicinal agents present: Sugar Antimicrobial Preservatives Flavorant Colorants Sucrose and non-sucrose based syrup Sucrose Dextrose Non-sugars Sorbitol Glycerin Propylene glycol Methylcellulose Hydroxyethylcellulose Most syrups contain a high proportion of sucrose, usually 60-80%. Concentrated sugar solutions are quite resistant to microbial growth. Simple syrup 85 g sucrose +purified water =100 ml syrup Antimicrobial preservative Benzoic acid (0.1 to 0.2%) Sodium benzoate (0.1 to 0.2%) Methyl-, propyl-, and butylparabens (0.1%) Alcohol (15 to 20%) Syrups can be preserved by 1) storage at low temperature 2) adding preservatives in the formulation 3) by the maintenance of a high concentration of sucrose as a part of the formulation Example Rx Active drug 5ml volume occupied Other drug solids 3 ml volume occupied Glycerin 15 ml Sucrose 25 g Ethanol 95% q.s. Purified water q.s. 100 ml How much alcohol would be required to preserve this prescription? Flavorant Synthetic flavorants Naturally occurring materials Volatile oils Vanillin Because syrups are aqueous preparations, these flavorants must be water soluble. Colorant The colorant is generally water soluble, nonreactive with the other syrup components, color stable at the pH range and under the intensity of light that the syrup is likely to encounter during its shelf life. green with mint brown with chocolate (2) Preparation of Syrups Syrups are frequently prepared by one of four general methods. 1) 2) 3) 4) solution of the ingredients with the aid of heat, solution of the ingredients by agitation without the use of heat, or the simple admixture of liquid components, addition of sucrose to a prepared medicated liquid or to a flavored liquid, percolation of either the source of the medicating substance or of the sucrose. Ⅰ. Solution With the Aid of Heat Syrups are prepared by this method when it is desired to prepare the syrup as quickly as possible, when the syrup’s components are not damaged or volatilized by heat. In this method the sugar is generally added to the purified water, and heat is applied until the sugar is dissolved. then other heat-stable components are added to the hot syrup, the mixture is allowed to cool, its volume is adjusted to the proper level by addition of purified water. If heatlabile agents or volatile substances, such as volatile flavoring oils and alcohol, are to be added, they are generally added to the syrup after the sugar is dissolved by heat, and the solution is rapidly cooled to room temperature. Because of the prospect of decomposition by heat, syrups cannot be sterilized by autoclaving. The use of boiled purified water in the preparation of a syrup can enhance its permanency, and the addition of preservative agents, when permitted, can protect it during its shelf life. Storage in a tight container is a requirement for all syrups. Ⅱ. Solution by Agitation Without the Aid of Heat To avoid heat-induced inversion of sucrose, a syrup may be prepared without heat by agitation. On a small scale, sucrose and other formulative agents may be dissolved in purified water and thorough agitated of the mixture. This process is more time consuming than use of heat, but the product has maximum stability. Huge glass-lined or stainless steel tanks with mechanical stirrers or agitators are employed in large-scale preparation of syrups. When solid agents are to be added to a syrup, it is best to dissolve them in a minimal amount of purified water and incorporate the resulting solution into the syrup. Ⅲ. Addition of Sucrose to a Medicated Liquid or to a Flavored Liquid Occasionally a medicated liquid, such as a tincture or fluidextract, is employed as the source of medication in the preparation of a syrup. Many such tinctures and fluidextracts contain alcohol-soluble constituents and are prepared with alcoholic or hydroalcoholic vehicles. If the alcohol-soluble components are desired medicinal agents, some means of rendering them water soluble is employed. If the tincture or fluidextract is miscible with aqueous preparations, it may be added derectly to simple syrup or to a flavored syrup. Ⅳ. Percolation (渗漉) In the percolation method, either sucrose may be percolated to prepare the syrup, or the source of the medicinal component may be percolated to form an extractive to which sucrose or syrup may be added. This latter method really is two separate procedures: first the preparation of the extractive of the drug and then the preparation of the syrup. Ipecac syrup Percolation Glycerin Syrup Ipecac dried rhizome roots of cephaelis ipecacuanha Extractive of powdered ipecac alkaloids emetine cephaeline psychotrine The usual dose of ipecac syrup is 15 ml. This amount of syrup is commonly used in the management of poisoning in children when the evacuation of the stomach contents is desirable. Ipecac syrup also has some application as a nauseant expectorant, in doses smaller than the emetic dose. 6. Elixirs Elixirs are clear, sweetened hydroalcoholic solutions intended for oral use and are uaually flavored to enhance their palatability. Nonmedicated elixirs are employed as vehicles; Medicated elixirs are used for the therapeutic effect of the medicinal substances they contain. Compared with syrups, elixirs are usually less sweet and less viscous. Elixirs are better able than aqueous syrups to maintain both water-soluble and alcoholsoluble components in solution. Each elixir requires a specific blend of alcohol and water to maintain all of the components in solution. In addition to alcohol and water, other solvents, such as glycerin and propylene glycol, are frequently employed in elixirs as adjunctive solvents. Although many elixirs are sweetened with sucrose or with a sucrose syrup, some use sorbitol, glycerin, and/or artificial sweeteners. All elixirs contain flavorings to increase their palatability, and most elixirs have coloring agents to enhance their appearance. Elixirs containing more than 10 to 12% of alcohol are usually self-preserving and do not require the addition of an antimicrobial agent. One advantage of elixirs over their counterpart drugs in solid dosage forms is the flexibility and ease of dosage administration to patients who have difficulty swallowing solid forms. A disadvantage of elixirs for children and for adults who choose to avoid alcohol is their alcoholic content. Elixirs should be stored in tight, lightresistant containers and protected from excessive heat. (1) Preparation of Elixirs Elixirs are usually prepared by simple solution with agitation and/or by admixture of two or more liquid ingredients. Alcohol-soluble and water-soluble components are generally dissolved separately in alcohol and in purified water, respectively. Then the aqueous solution is added to the alcoholic solution to maintain the highest possible alcoholic strength at all times so that minimal separation of the alcoholsoluble components occurs. When the two solutions are completely mixed, the mixture is made to volume with the specified solvent or vehicle. Frequently the final mixture will be cloudy because of separation of some of the flavoring oils by the reduced alcoholic concentration. Talc Filter (2) Nonmedicated Elixirs (a) (b) Nonmedicated elixirs may be useful to the pharmacist in the extemporaneous filling of prescriptions involving the addition of a therapeutic agent to a pleasant-tasting vehicle, dilution of an existing medicated elixir. In selecting a liquid vehicle for a drug substance, the pharmacist should be concerned with the solubility and stability of the drug substance in water and alcohol. All components should be chemically and physically compatible. The three most commonly used nonmedicated elixirs were aromatic elixir, compound benzaldehyde elixir (复方安息 香醛酏剂), isoalcoholic elixir. (3) Medicated Elixirs Antihistamines elixirs are useful primarily in the symptomatic relief of certain allergic disorders. The most common untoward effect is sedation. Other common adverse effects include dryness of the nose, throat, and mouth; dizziness; and disturbed concentration. Barbiturate sedative/hypnotic elixirs Barbiturates are administered in small doses in the daytime hours as sedatives to reduce restlessness and emotional tension. Greater doses may be given before bedtime as hypnotics to release insomnia. long-acting intermediate-acting short-acting ultrashort-acting phenobarbital amobarbital pentobarbitol secobarbitol thiopental Phenobarbital Elixir Phenobarbital elixir is formulated to contain phenobarbital 0.4%,which provides about 20 mg of drug per teaspoonful (5mL)of elixir. Orange oil Colored red Syrup Glycerin Digoxin Elixir Digoxin is poisonous, and its dose must be carefully determined and administered to each individual patient. The official elixir contains about 10% of alcohol. Dropper 100 ml elixir 4.5 mg to 5.25 mg 0.25 mg/5mL teaspoonful Cardiotonic agent 1.5 mg initial therapy 0.5 mg maintenance therapy 7. Tinctures Tinctures are alcoholic or hydroalcoholic solutions prepared from vegetable materials or from chemical substances. They vary in method of preparation, strength of the active ingredient, alcoholic content, and intended use in medicine or pharmacy. Depending on the praparation, tinctures contain alcohol in amounts ranging from approximately 15 to 80%. The alcohol content protects against microbial growth and keeps the alcoholsoluble extractives in solution. In addition to alcohol, other solvents, such as glycerin, may be employed. Tinctures must be tightly stoppered and not exposed to excessive temperatures. Many tinctures must be stored in lightresistant containers and protected from sunlight. paregoric camphorated tincture of opium 8. Proper Administration and Use of Liquid Peroral Dosage Forms The liquid dosage forms should be measured out in calibrated devices for administration. Even though these are liquids, it is recommended that the patient follow the administration of the liquid dosage form with a glassful of water. The pharmacist must be careful in the selection of liquid products given the patient’s history and other concurrent medicines. Diabetic patient Antabuse-like activity Another drug-drowsiness 9. Topical Solutions and Tinctures Generally, the topical solutions employ an aqueous vehicle, whereas the topical tinctures characteristically employ an alcoholic vehicle. As required, cosolvents or adjuncts to enhance stabililty or the solubility of the solute are employed. Most topical solutions and tinctures are prepared by simple dissolving. However, certain solutions are prepared by chemical reaction. Because of the nature of the active constituents or the solvents, many topical solutions and tinctures are self-preserved. (1) Sprays Sprays may be defined as aqueous or oleaginous solutions in the form of coarse droplets or as finely divided solids to be applied topically, most usually to the nasopharyngeal tract or to the skin. Many commercial sprays are used intranasally to relieve nasal congestion and inflammation and to combat infection and contain antihistamines, sympathomimetic agents, and antibiotic substances. Other sprays that are employed against sunburn and heat burn contain local anesthetics, antiseptics, skin protectants, and antipruritics. Throat sprays containing antiseptics, deodorants, and flavorants may be effectively employed to relieve conditions such as halitosis, sore throat, and laryngitis. Other sprays treat athlete’s foot and other fungal infections. Recently, one-way pump sprays have been developed to deliver medication into the nose. (2) Aluminum Acetate Topical Solution Aluminum acetate is colorless and has a faint acetous odor and a sweetish, astringent taste. It is widely applied topically as an astringent wash or wet dressing after dilution with 10 to 40 parts of water. It is frequently used in various types of dermatologic lotions, creams, and pastes. (3) Aluminum Subacetate Topical Solution Aluminum subacetate (碱式醋酸铝) topical solution, is used in prepatation of aluminum acetate topical solution. Aluminum acetate topical solution, diluted first with 20 to 40 parts of water, is used externally as an astringent wash and wet dressing. (4) Calcium Hydroxide Topical Solution Calcium hydroxide topical solution, commonly called limewater, must contain not less than 140 mg of Ca(OH)2 in each 100 mL of solution. Calcium hydroxide is less soluble in hot than in cold water, and cool purified water is the solvent. The solution should be stored in well-filled, tightly stoppered containers to deter the absorption of carbon dioxide and should be kept in a cool place to maintain an adequate concentration of dissolved solute. The solution is categorized as an astringent. For this purpose it is generally employed in combination with other ingredients in dermatologic solutions and lotions to be applied topically. (5) Coal Tar Topical Solution Coal tar topical solution is an alcoholic solution containing 20% coal tar and 5% polysorbate 80. The final content is 81 to 86% ethyl alcohol. Coal tar is a nearly black viscous liquid having a characteristic naphthalene-like odor and a sharp, burning taste. It is slightly soluble in water and partially soluble in most organic solvents, including alcohol. Coal tar is a local antieczematic. The solution is used in external treatment of a wide variety of chronic skin conditions after dilution with about 9 volumes of water, or in combination with other agents in various lotions, ointments or solutions. (6) Hydrogen Peroxide Topical Solution Hydrogen peroxide topical solution contains 2.5 to 3.5%(w/v) hydrogen peroxide, or H2O2 . The solution is a clear, colorless liquid that may be odorless or have the odor of ozone. It usually deteriorates upon long standing , forming oxygen and water. Preservative agents, such as acetanilide, have been found to retard decomposition. Decomposition is enhanced by light and by heat, and for this reason the solution should be preserved in tight, light-resistant containers, preferably at a temperature not exceeding 35℃. The solution is also decomposed by practically all organic matter and other reducing agents and reacts with oxidizing agents to liberate oxygen and water; metals, alkalies, and other agents can catalyze its decomposition. Hydrogen peroxide solution is categorized as a local anti-infective for use topically on the skin and mucous membranes. (7) Chlorhexidine Gluconate Solution Chlorhexidine gluconate has been employed extensively as a broad-spectrum antiseptic in clinical and veterinarian medicine. Its spectrum encompasses gram-positive and gram-negative bacteria, including Pseudomonas aeruginosa. In a concentration of 4% (Hibiclins, Stuart) it is used as a surgical scrub, hand wash, and skin wound and general skin cleanser. The most common side effect of chlorhexidine is the formation of an extrinsic yellow-brown stain on the teeth and tongue after only a few days of use. The developed stain can be periodically removed with dental prophylaxis. (8) Povidone Iodine Topical Solution The agent povidone iodine is a chemical complex of iodine with polyvinylpyrrolidone. The povidone iodine complex contains approximately 10% available iodine and slowly releases it when applied to the skin. The preparation is employed topically as a surgical scrub and nonirritating antiseptic solution, with its effectiveness directly attributable to the presence and release of iodine from the complex. (9) Thimerosal(硫柳汞) Topical Solution Thimerosal is a water-soluble organic mercurial antibacterial agent used topically for its bacteriostatic and mild fungistatic properties. It is used mainly to disinfect skin and as an application to wounds and abrasions. It has been applied to the eye, nose, throat, and urethra in dilutions of 1:5000. It is also used as a preservative for various pharmaceutical preparations. The solution must be maintained in lightresistant containers 0.1% Thimerosal Ethylene diamine solution Sodium borate Monoethanolamine Thimerosal topical solution contains 0.1% thimcrosal. The solution is affected by light and must be maintained in light-resistant containers. 10. Vaginal and Rectal Solutions (1) Vaginal Douches Solutions may be prepared from powders as indicated earlier or from liquid solutions or liquid concentrates. In using liquid concentrates , the patient is instructed to add the prescribed amount of concentrate to a certain amount of warm water. The user simply adds the prescribed amount of powder to the appropriate volume of warm water and stirs until dissolved. Among the components of douche powders are the following: 1. Boric acid or sodium borate 2. Astringents 3. Antimicrobials 4. Quaternary ammonium compounds 5. Detergents 6. Oxidizing agents 7. Salts, e.g. ,sodium citrate, sodium chloride 8. Aromatics, e.g. , menthol, thymol. (2) Retention Enemas hydrocortisone A number of solutions are administered aminophylline rectally for the local effects of the medication or for systemic absorption. Clinically effective blood levels of the agents are usually obtained within 30 minutes following rectal instillation. (3) Evacuation Enemas - - Rectal enemas are used to cleanse the bowel. The agents present are solutions of sodium phosphate and sodium biphosphate glycerin and docusate potassium light mineral oil The patient should be advised to gently insert the tip of the product with steady pressure and be told that it is not absolutely necessary to squeeze all of the contents out of the disposable plastic bottle. The patient should be told that the product will most probably work within 5 to 10 minutes. 11. Topical Tinctures (1) Iodine Tincture 2% iodine crystals 2.4% sodium iodide Alcohol Purified water I2+NaINaI3 This reaction prevents the formation of ethyl iodide from the interaction between iodine and the alcohol, which would result in the loss of the antibacterial activity of The tincture. The tincture is a popular local anti-infective agent applied to the skin, is useful in delineating the application over the affected skin area. The tincture should be stored in a tight container to prevent loss of alcohol. (2) Compound Benzoin Tincture Maceration in alcohol of 10% benzoin 24% aloe, storax and tolu balsam The tincture is categorized as a protectant. It is used to protect and toughen skin in the treatment of bedsores, ulcers, cracked nipples, and fissures of the lips and anus. It is also commonly used as an inhalant in bronchitis and other respiratory conditions. Compound tincture of benzoin serves as a delivery vehicle of podophyllum in the treatment of venereal warts. (3) Thimerosal Tincture The commercial preparation is colored orange red and has greenish fluorescence. 0.1% Thimerosal The red stain it leaves on the Monoethanolamine skin defines the area of Distilled water application. Acetone It is a commonly used 50% alcohol household antiseptic for application to abrasions and cuts and also in preparation of patients for surgery. 12. Special application solutions (1) nasal preparations The vast majority of preparations intended for intranasal use contain adrenergic agents and are employed for their decongestant activity on the nasal mucosa. Nose drops Sprays Jellies Nasal decongestant solutions Most nasal decongestant solutions are aqueous preparations rendered isotonic to nasal fluids (approximately equivalent to 0.9% sodium chloride), buffered to maintain drug stability (pH5.56.5) stabilized and preserved as required. Most of the adrenergic drugs used in nasal decongestant solutions are synthetic compounds epinephrine. Most solutions for nasal use are packaged in dropper bottles or in plastic spray bottles, usually containing 15 to 30 ml of medication. The concentration of adrenergic agent is ranging from about 0.05 to 1.0%. Nasal decongestant solutions are employed in the treatment of rhinitis of the common cold and for vasomotor and allergic rhinitis including hay fever, and for sinusitis. The frequent use or their use for prolonged periods may lead to chronic edema of the nasal mucosa. Thus, they are best used for short periods (no longer than 3 to 5 days). (2)Otic Solution Ear preparations are usually placed in the ear canal by drops or in small amounts for the removal of excessive cerumen (ear wax) or for the treatment of ear infections, inflammation, or pain. Cerumen-removing solutions Light mineral oil Vegetable oils Hydrogen peroxide Solution of Synthetic surfactants Commercial products 1) Triethanolamine polypeptide oleate-condensate in propylene glycol 2) Carbamide peroxide in glycerin/ Propylene glycol Anti-infective, anti-inflammatory, and analgesic ear preparations Drugs used topically in the ear for their antiinfective activity include chloramphenicol colistin sulfate neomycin polymyxin B sulfate nystatin Anti-inflammatory agents -Hydrocortisone -Dexamethasone sodium phosphate -Acetic acid (2%) in aluminum acetate solution -Boric acid (2.75%) in isopropyl alcohol Topical analgesics antipyrine local anesthetic benzocaine in a vehicle of propylene glycol or anhydrous glycerin Preservation Chlorobutanol (0.5%) Thimerosal (0.01%) Combinations of the parabens Antioxidants Sodium bisulfite Stabilizers 13. Miscellaneous Solutions (1) Aromatic Waters Aromatic waters are clear, aqueous solutions saturated with volatile oils or other aromatic or volatile substances. Aromatic waters may be used for perfuming and/or flavoring. (2) Diluted Acids Diluted acids are aqueous solutions prepared by diluting the corresponding concentrated acids with purified water. The strength of a diluted acid is generally expressed on a percent weght-to-volume (% w/v) basis, that is, the weight in grams of solute per 100 mL of solution, whereas the strength of a concentrated acid is generally expressed in terms of percent weight to weight (% w/w), which indicates the number of grams of solute per 100 g of solution. To prepare a diluted acid from a concentrated one, it is necessary first to calculate the amount of solute required in the diluted product. Then the amount of concentrated acid required to supply the needed amount of solute can be determined. To illustrate, concentrated hydrochloric acid (HCl) contain not less than 35 g and not more than 38 g of solute per 100 g of acid and therefore is considered to be, on the average, 36.5% w/w in strength. Diluted HCl contains 9.5 to 10.5 g of solute per 100 mL of solution and is therefore considered to be approximately 10% w/v in strength. If one wished to prepare 100mL of the diluted acid from the concentrated acid, one would require 10 g of solute. The amount of concentrated HCl required to supply this amount of solute may be calculated by the following proportion: Thus, 27.39 g of concentrated acid is required to supply 10 g of solute needed for the preparation of 100 mL of the diluted acid. Concentrated sulfuric acid 95-98% (w/w) Concentrated nitric acid 69-71% (w/w) Concentrated phosphoric acid 85-88% (w/w) (3) Spirits Spirits are alcoholic or hydroalcoholic solutions of volatile substances. Generally, the alcoholic concentration of spirits is rather high, usually over 60%. Because of the greater solubility of aromatic or volatile substances in alcohol than in water, spirits can contain a greater concentration of these materials than the corresponding aromatic waters. Spirits may be used pharmaceutically as flavoring agents and medicinally for the therapeutic value of the aromatic solute. For medicinal purposes, spirits may be taken orally, applied externally, or used by inhalation, depending upon the particular preparation. When taken orally, they are generally mixed with a portion of water to reduce the pungency of the spirit. 14. Nonaqueous Solutions (1) Liniments (搽剂) Liniments are alcoholic or oleaginous solutions or emulsions of various medicinal substances intended to be rubbed on the skin. Liniments are useful when rubefacient, counterirritant, or penetrating action is desired; oleaginous liniments are employed primarily when massage is desired. All liniments should bear a label indicating that they are suitable only for external use and must never be taken internally. Oleaginous liniments The solvent may be fixed oil such as almond oil peanut oil sesame oil cottonseed oil volatile substance such as winter-green oil or turpentine (2) Collodions(火棉胶) Collodions are liquid preparations composed of pyroxylin (硝酸纤维素) dissolved in a solvent mixture usually composed of alcohol and ether with or without added medicinal substances. Pyroxylin, like collodions, is exceedingly flammable and must be stored away from flame in well-closed containers, protected from light. Collodions are intended for external use. Collodion Collodion is a clear or slightly opalescent viscous liquid . The product is capable of forming a protective film on application to the skin and the volatilization of the solvent. The flim is useful in holding the edges of an incised wound together. However, its presence on the skin is uncomfortable because of its inflexible nature. Flexible collodion (弹性火棉胶) Flexible collodion is prepared by adding 2% camphor and 3% castor oil to collodion. The castor oil renders the product flexible, permitting its comfortable use over skin areas that are normally moved, such as fingers and toes. The camphor makes the product waterproof. Salicylic acid coilodion It is used for its keratolytic effects, especially in the removal of corns from the toes. The product should be applied one drop at a time on the corn or wart, allowing time to dry before the next drop is added. Proper tightening and storage of the product after use are absolutely necessary because of the volatility of the vehicle. 15. Extraction Methods for Preparing Solutions Certain pharmaceutical preparations are prepared by extraction, that is, by withdrawal of desired constituents from crude drugs through the use of selected solvents in which the desired constituents are soluble. Water Hydroalcoholic mixtures Glycerin Methods of Extraction The principal methods of drug extraction are maceration and percolation. Generally, the method of extraction selected for a given drug depends on several factors, including the nature of the crude drug, its adaptability to each of the various extraction methods, and the interest in obtaining complete or nearly complete extraction of the drug. (1) Maceration (浸渍) It is a process in which the properly comminuted drug is permitted to soak in the menstruum until the cellular structure is softened and penetrated by the menstruum and the soluble constituents are dissolved. For drugs containing little or no cellular material, such as benzoin(安息香), aloe (芦荟), and tolu(妥鲁香 ), which dissolve almost completely in the menstruum, maceration is the most efficient method of extraction. Maceration is usually conducted at a temperature of 15℃ to 20 ℃ for 3 days or until the soluble matter is dissolved. (2) Percolation(渗漉) It may be described generally as a process in which a comminuted drug is extracted of its soluble constituents by the slow passage of a suitable solvent through a column of the drug. The drug is packed in a special extraction apparatus termed a percolator, with the collected extractive called the percolate. Most drug extractions are performed by percolation . In the process of percolation the flow of the menstruum over the drug column is generally downward to the exit orifice, drawn by the force of gravity as well as the weight of the column of liquid. In certain specialized and more sophisticated percolation apparatus, additional pressure on the column is exerted with positive air pressure at the inlet and suction at the outlet or exit. Percolators for drug extraction vary greatly as to their shape, capacities, composition, and, most important utility. Percolators employed in the large-scale industrial preparation of extractive are generally stainless steel or glasslined metal vessels that vary greatly in size and in operation. Percolation on a small scale generally involves the use of glass percolators of various shapes for extraction of small amounts (perhaps up to 1000 g) of crude drug. The cylindrical percolator is particularly suited to the complete extraction of drugs with a minimal expenditure of menstruum. Example preparations prepared by extraction processes Fluidextracts Extracts Questions 1. 2. 3. 4. How to prepare purified water? What solvents are commonly used for liquid preparations? What are elixirs and tinctures? Please give examples to explain how to prepare medicated elixirs and tinctures?