Glycogen synthase
advertisement

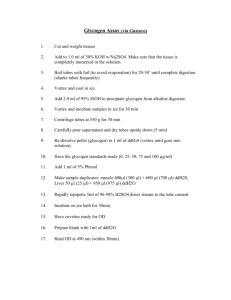
Dr. S.Chakravarty MD Points to be covered- Introduction Biomedical importance Glycogen Synthesis- Glycogenesis Regulation of glycogenesis Glycogen Breakdown- Glycogenolysis Regulation of glycogenolysis Reciprocal regulation of Glycogen Metabolism Glycogen Storage Diseases INTRODUCTION Glycogen - storage form of glucose - stored in the liver and the skeletal muscles - energy reserve. A homopolysaccharide - linear chain of (1→4) linked glucosyl residues with branches joined by (1→6) linkages. Glycogen in liver (6-8%) is higher than that in the muscles (1-2%). Liver glycogen - first line of defense against declining blood glucose levels especially between meals. Tissue Weight 1.8 kg Body Content Liver glycogen Percentage of Tissue Weight 5.0 Muscle glycogen Extracellular glucose 0.7 0.1 35 kg 10 L 245 g 10 g 90 g USMLE Biomedical Importance: 1. In health, liver glycogen maintain blood glucose level particularly between meals whereas muscle glycogen is a readily available source of glucose in the exercising muscles. 2. Deficient mobilization and abnormal accumulation of glycogen leads to certain disorders called as GLYCOGEN STORAGE diseases which can lead to muscular weakness and even death in the affected individual. REM-Glucose 6-phosphatase is absent in muscle-so NO contribution to plasma glucose level by muscle glycogen-only locally available glucose 6-P for glycolysis and HMP shunt GLYCOGEN SYNTHESIS(GLYCOGENESIS): Glycogen - synthesized from glucose. Site : Liver, Skeletal Muscles Subcellular site: cytosol Steps: 1.Synthesis of UDP-Glucose 2.Synthesis of Primer to initiate Glycogen synthesis 3.Elongation of chain 4.Formation of branches in Glycogen 1. Synthesis of UDP-Glucose Glucose ATP Glucokinase Hexokinase ADP Glucose-6-phosphate Phosphoglucomutase Glucose-1-phosphate UTP UDP-Glucose pyrophosphorylase PPi UDP- Glucose Pyrophosphate - is hydrolyzed to inorganic phosphate by Pyrophosphatase and thus ensures the IRREVERSIBILITY of this reaction. 2.Synthesis of PRIMER to initiate Glycogen synthesis: Primer is a preexisting (1→4) glucosyl chain with Glycogenin which will accept the glucosyl residues donated by UDPG. Normally a fragment of glycogen serves as a primer. When glycogen stores are depleted, a specific protein known as GLYCOGENIN provides the site at which the primer is built. Tyrosyl-OH + UDPG UDPG + glycogen primer (n residue) Tyrosyl-o-glucose + UDP UDP + Glycogen (n+1residues) 3. Elongation of the chain: UDP Glucose Glycogen synthase + UDP 4. Formation of Branches in Glycogen: The branch points - created by the action of BRANCHING enzyme. Also called as glucosyl 4:6 transferase OR amylo [14] [1-6]transglucosidase When the the chain is minimum 11 glucose residues long , branching enzyme removes a block of 6-8 glucosyl units from the non reducing end of the chain and attaches it via an (1→6) linkage to a glucose residue of the same or other chain. Branching enzyme New branch point created ( (1→6) linkage ) Regulation of glycogenesis: Rate limiting enzyme - GLYCOGEN SYNTHASE Regulated by- 1. Allosteric regulation: +ve modifiers- Glucose-6-phosphate in the liver and muscles. 2. Covalent modification: By phosphorylation & dephosphorylation Protein Kinase Glycogen synthase Glycogen synthase (Dephosphorylated) (active) Protein phosphatase (Phosphorylated) (Inactive) Hormonal regulation Glucagon/Epinephrine Insulin + Adenylate cyclase Phosphodiesterase ATP cAMP Inactive protein kinase 5’AMP Active protein kinase Protein Kinase Glycogen synthase Glycogen synthase (Dephosphorylated) (active) (Phosphorylated) Protein phosphatase (Inactive) + Glycogenesis stimulated Glycogenesis inhibited GLYCOGEN BREAKDOWN (GLYCOGENOLYSIS) The principal enzyme of glycogenolysis - GLYCOGEN PHOSPHORYLASE. Glycogen + Pi Glycogen + Glucose – 1-P ( n residues) Phosphorylase (n-1 residues) glucosyl 4:4 transferase activity transfers the 3 of the 4 glucosyl units and involves cleaving of an (1→4)linkage at one site and formation of new (1→4)bond elsewhere. The key enzyme for removing branch points is the debranching enzyme - (1→6) glucosidase activity – free glucose released. Glycogenolysis: + Phosphorylase Glucan Transferase Debranching enzyme (Glucosidase or 1,6 glycosidase) Glucose molecules are removed sequentially by PHOSPHORYLASE until approximately 4 glucose remain on either side of a 16branch point Glucan transferase removes a trisaccharide from one branch to the other. Glucosidase removes the remaining glucose Regulation of Glycogenolysis: The rate limiting enzyme of glycogenolysis is glycogen phosphorylase which is regulated by1. Allosteric regulation - +ve modifiers- AMP -ve modifiers- ATP in liver and muscles Glucose in liver Glucose-6-phosphate in muscles 2.Covalent modification-Phosphorylated form is active. Phosphorylase kinase Glycogen phosphorylase Glycogen phosphorylase (dephosphorylated) (phosphorylated) (inactive) Protein phosphatase (active) 3.Ca ions- activates phosphorylase kinase Hormonal regulation Glucagon/Epinephrine Insulin + Adenylate cyclase Phosphodiesterase ATP cAMP Inactive protein kinase 5’AMP Active protein kinase Phosphorylase Kinase Glycogen phosphorylase Glycogen phosphorylase (Dephosphorylated) (Inactive) (Phosphorylated) Protein phosphatase (active) + Glycogenolysis stimulated Reciprocal regulation Regulation of Glycogenolysis in muscle: Glucose loading in Sports!! • i.v glucose loading( CARBO-LOADING ) for 1-2 days prior to sports event has been extensively used by athletes to build up stores of glycogen to enhance performance later on during the contest. Glycogen storage diseases Abnormalities in metabolism of glycogen leads to a group of disorders called Glycogen storage diseases. Types- Hepatic (I III,IV,VI,and VIII) Myopathic(V and VII) General features – Hypoglycemia , poor exercise tolerance , lactic acidosis Muscle weakness in myopathic forms Hepatic fibrosis and hepatomegaly(due to accumulation of glycogen in liver) Glycogen Storage Diseases USMLE Type Name Enzyme Deficiency Clinical Features 0 — Glycogen synthase Hypoglycemia; hyperketonemia; early death Ia Von Gierke's disease Glucose 6phosphatase Ib — II Pompe's disease IIIa Limit dextrinosis, Forbe's or Cori's disease Liver and muscle Fasting hypoglycemia; hepatomegaly in infancy; debranching enzyme accumulation of characteristic branched polysaccharide (limit dextrin); muscle weakness IIIb Limit dextrinosis Liver debranching enzyme Glycogen accumulation in liver and renal tubule cells; hypoglycemia; lactic acidemia; ketosis; hyperlipemia, hyperuricemia Endoplasmic As type Ia; neutropenia and impaired reticulum glucose 6- neutrophil function leading to recurrent phosphate infections transporter Accumulation of glycogen in lysosomes: Lysosomal α 14 juvenile onset variant, muscle hypotonia, death and α16 glucosidase (acid from heart failure by age 2; adult onset variant, maltase) muscle dystrophy As type IIIa, but no muscle weakness harper USMLE IV Amylopectinosis, Branching enzyme Hepatosplenomegaly; accumulation of Andersen's amylopectin like polysaccharide with few branch disease points; death from heart or liver failure before age 5 V Myophosphorlyl Muscle Poor exercise tolerance; muscle glycogen ase deficiency, phosphorylase abnormally high (2.5–4%); blood lactate very low McArdle's after exercise syndrome VI Hers' disease Liver Hepatomegaly; accumulation of glycogen in liver; phosphorylase mild hypoglycemia; generally good prognosis VII Tarui's disease Muscle and Poor exercise tolerance; muscle glycogen erythrocyte abnormally high (2.5–4%); blood lactate very low phosphofructokin after exercise; also hemolytic anemia ase 1 VIII Liver Hepatomegaly; accumulation of glycogen in liver; phosphorylase mild hypoglycemia; generally good prognosis kinase IX Liver and muscle Hepatomegaly; accumulation of glycogen in liver phosphorylase and muscle; mild hypoglycemia; generally good kinase prognosis X cAMP-dependent Hepatomegaly; accumulation of glycogen in liver protein kinase A harper • Glucose 6 phosphatase deficiency • Hypoglycemia not responding even to i.v glucagon/epinephrine . • Lactic acidosis – Impairment of gluconeogenesis. • Accumulation of G6P inhibits conversion of lactate to pyruvate. The lactic acid level rises during fasting as glucose falls. In people with GSD I, it may not fall entirely to normal even when normal glucose levels are restored. • Hepatomegaly – progressing to cirrhosis • Hyperuricemia ?? ---- increased glucose 6 P increased influx into HMP shunt increased Ribose 5P INCREASED DENOVO BIOSYNTHESIS OF Nucleic acids. Pompe’s disease: • Type II – Glycogen storage disease: • Lysosomal α 14 and α16 glucosidase (acid maltase) deficiency. • Affects - liver , muscle and heart. • Accumulation of glycogen in vacuoles • Death due to cardiac failure • Massive cardiomegaly. • Normal blood glucose levels. Anderson Disease: • Def of Branching enzyme – • Accumulation of poorly branched polysaccharide – with minimal branching • Amylopectin like appearance of glycogen molecules • Normal blood glucose levels • Death in first year of life Cori disease/Forbes disease: • Def. of enzyme – Debranching enzyme • Accumulation of abnormal small dextrin like polysaccharides in liver. • Hypoglycemia seen. 6-month-old who is failing to thrive is brought to your clinic. Tests reveal hepatosplenomegaly, muscle weakness and atrophy, hypotonia, and decreased deep tendon reflexes. Blood tests reveal that the infant has normal glucose levels. Biopsy of the liver reveals initial stages of cirrhosis due to the accumulation of an abnormal glycogen with few branch points, whose structure resembles amylopectin. The clinical and laboratory results presented are indicative of which glycogen storage disease? •Von Gierke disease •Tarui disease •Andersen disease •Cori or Forbes disease •McArdle disease Branching enzyme An infant with growth retardation, hepatomegaly and hypoglycemia demonstrate hepatic fibrosis without fat accumulation on liver biopsy. There is also accumulation of small chain dextrin- like material within the cytosol of the hepatocytes. Which of the following enzymes is most likely deficient in this patient? •Glucose -6-phosphate •Glycogen phosphorylase •Debranching enzyme •Amylo-α (1,6) –glucosidase •Pyruvate kinase. Cori’s or Forbe’s or Limit Dextrinosis After a meal, blood glucose enters cells and is stored as glycogen, particularly in the liver. Which of the following is the donor of new glucose molecules in glycogen? • • • • • UDP-glucose-1-phosphate UDP-glucose UDP-glucose-6-phosphate Glucose-6-phosphate Glucose-1-phosphate