Approach To Patient With Iron Deficiency Anaemia
advertisement

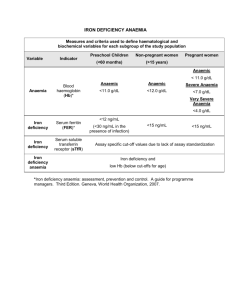
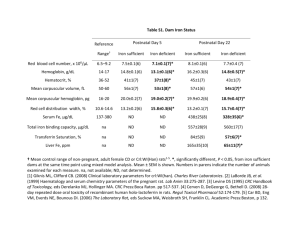
Approach To Patient With Iron Deficiency Anaemia By Sin Kaan Chan 11/7/02 Scenario A 40 years old lady, presented with pallor, lethargy, palpitations and SOB on exertion. FBC: Hb 7.5g/dl MCV 64fl MCH 18.5pg WBC and differential normal Platelet normal range What is next? Differential Diagnosis of Hypochromic Microcytic Anaemia Fe deficiency Anaemia of chronic disease Thalassaemia Sideroblastic anaemia (rare) Causes of Iron Deficiency Bleeding: Menorrhagia GI bleed Peptic ulcer Oesophageal varices Aspirin ingestion Hookworm Neoplasm IBD Haemorrhoids Factors contributing to Iron Deficiency Increased demands: Pregnancy (commonest factor and increases with parity) Growth (infancy and adolescent) Erythropoietin therapy Causes of Iron Deficiency Malabsorption: Gluten-induced enteropathy Gastrectomy Poor diet History Any ongoing bleeding? Menstrual history Passing bloody stool / black stool Any abdominal symptoms? Easy bruising or bleed? (clotting or platelet abN) Medications Diet How long has the patient been anaemic? History Past medical history: Any chronic diseases? (renal, liver, connective tissue…etc) Family history: Thalassaemia, cancer, other illness Social History: Racial origin (thalassaemia more common in Mediterranean/Southern Asian) Smoking, alcohol Vegetarian Haematological Examination Basically a thorough examination from head to toe. In Fe deficiency: General: pallor Hands: Pale ridged or spoon-shaped nails (koilonychia) Pulse rate increase Pale conjunctiva Painless glossitis/angular stomatitis Investigations Repeat FBC including ESR (to better evaluate ferritin result) FE study Fe deficiency Serum Decrease Fe Chronic Thalassae diseases mia Decrease Normal TIBC Decrease Normal Increase Serum Decrease Ferritin Normal/ increase Normal Investigations The above studies will sort out single-cause cases. Where multiple causes confuse the picture enough to prevent diagnosis, may rarely have to undertake: Bone marrow iron Sensitive and reliable test for Fe deficiency Prussian blue stain for stored iron in macrophages and erythroblasts In iron deficiency, decrease or absence Investigation For Cause of Iron Deficiency GI bleed History, physical and rectal examination Occult blood tests Upper GI endoscopy, sigmoidoscopy, or colonoscopy. Abdominal X-ray, Barium study Microscope stool for hookworm ova Investigation For Cause of Iron Deficiency Malabsorption If history highly suspected, - Test for endomysial and gluten antibodies. - Duodenal biopsy Management Principle: Determine and treat underlying cause. Correct anemia and replenish iron stores by oral iron. Oral Iron Ferrous sulphate Ferrous gluconate Should be given long enough to correct anaemia and replenish iron stores. Therefore given for at least 6 months. Failure to Response to Oral Iron Possible cause considered b4 parenteral iron used. Possible causes: Continuing bleeding Failure to take tablets Wrong dx – thalassaemia trait / sideroblastic anaemia Other causes – malignancy, inflammation Malabsorption Parenteral Iron Iron-sorbitol-citrate Repeated deep IM injections Ferric hydroxide-sucrose Slow IV injection or infusion May have hypersensitivity or anaphylactic reaction Summary…… Approach to iron deficiency: Determine and treat the underlying cause!