Update on Treatment of Type 1 Diabetes in Children
advertisement

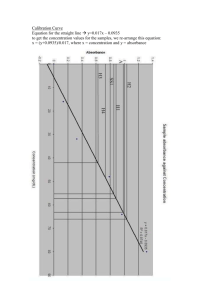
Diabetes in Young Children The Lollipop Brigade Francine R. Kaufman, M.D. Professor of Pediatrics The Keck School of Medicine of USC Head, Center for Diabetes and Endocrinology Childrens Hospital Los Angeles What Will Be Discussed What are the Targets for Young Children? What are the Diabetes Regimens? Is There a Greater Risk of Hypoglycemia? What are the Developmental Issues ? Question What are the glycemic targets for young children? Glycemic Targets Glucose values are plasma (mg/mL) Age Pre-Meal BG HS/Night BG HbA1c Toddler (0-5 yrs) 100-180 110-200 ≥7.5 & ≤8.5% School-age (6-11 yrs) 90-180 100-180 <8% Adolescent (12-19 yrs) 90-130 90-150 <7.5% Diabetes Care 28:186-212, 2005 But What are the Goals? To give your child a loving, supportive environment where each day is taken at a time (not each blood sugar) Where your child can grow and thrive, learn and explore Where blood sugars are corrected, not interrogated Where the family is in balance – like a mobile And where the long haul is what is important Question Can Intensive Management Be Done Safely in Young Children? CHLA Type 1 DM Year 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 N 357 414 468 747 887 991 1072 1285 1375 1664 1635 Mean 8.4 8.6 8.5 8.2 8.3 8.5 8.5 8.2 8.3 8.2 8.07 A1c % <7 18 20 % 7- 46 7.99 % 37 8-10 % 17 >10 37 44 51 47 42 42 50 48 29 34 45 42 38 40 44 44 39 40 42 35 18 14 11 13 14 14 11 12 11 11 HbA1c Statistics for CHLA 2003 Type 1: Diabetes > 1 year, followed > 1 year Enrolled in Long-term study – total n 1375 n Average ± SD All patients 1375 8.2 ± 1.6 Males 673 8.2 ± 1.6 Females 702 8.2 ± 1.6 <5 61 7.8 ± 1.3 5-10 450 7.9 ± 1.3 11-16 579 8.4 ± 1.8 17-19 >20 157 127 8.3 ± 1.5 7.4 + 1.3 Evaluation of Young Children at CHLA Kaufman, et al, Pediatr Diabetes, 3:179-183, 2002. Retrospective analysis of data 147 children < 8 years of age 2 year data from July 99 – July 2001 Study Question : Is HbA1c < 8.0 associated with more severe or assymptomatic hypoglycemia? <8.0 >8.0 P Age 5.77 5.67 0.7 Duration 2.56 2.88 0.2 HbA1c 7.0+.76 8.7+.74 <0.001 Regimen 2.9 3.0 0.29 U/kg 0.57 0.62 0.15 n 89 58 Hypoglycemia 5.6 3.4 NS DKA 1.1 3.4 NS Competency 4.0 3.6 0.019 % within 40.3 29.2 <0.0001 % above 37.1 51.7 <0.0001 % below 22.7 19.1 0.23 Question What are the principles of management? Diabetes Management Principles An effective insulin regimen Monitoring of glucose As flexible with food and activity as possible Must remember Young children need routine and rules Young children need to develop autonomy Young children need to explore and experience Young children need to begin to make decisions Insulin management Fixed dose regimens: requires scheduled meals and snacks and is not flexible enough for most young children Basal: bolus regimens: MDI useful only if child is willing to take frequent injections Insulin pumps child must be willing to wear the pump Basal/Bolus Treatment Program with Rapid-acting and Long-acting Analogs Plasma insulin Breakfast Lunch Dinner Aspart Aspart Lispro Lispro Glulysene Glulysine Aspart Lispro Glulysine Glargine or Detemir 4:00 8:00 12:00 16:00 Time 20:00 24:00 4:00 8:00 Type 1 Diabetes: Serum Insulin Concentrations Following Subcutaneous Injection of Insulin Lispro or Human Regular 3.0 2.5 Injection Insulin Lispro (n=10) Human Regular (n=10) Serum 2.0 Insulin Conc. 1.5 (ng/mL) 1.0 Mean + SE 0.5 0.2 mU/min/kg insulin infusion 0.0 -60 0 60 Meal 120 180 240 300 360 420 480 Heinemann et al. Diabetic Medicine,13:625-629, 1996 Time (minutes) Effectiveness of Postprandial Humalog in Toddlers Rutledge, Chase, Klingensmith et al Pediatrics 100:968,97 Determine if postprandial rapid-acting insulin effective Subjects < 5 years old Results: 2-hour glucose excursions lower with postprandial Humalog compared to preprandial regular Similar to preprandial Humalog Glucose Infusion Rates (mg/kg/min) Insulin Glargine - Pharmacokinetics by Glucose Clamp 6 NPH 5 4 Glargine 0.4 U/kg 3 2 Placebo 1 0 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 Hours Linkeschowa R, et al. Diabetes.1999;48(Suppl 1):A97. Insulin Detemir – Pharmacokinetics by Glucose Clamp Glucose Infusion Rate (mg/kg/min) 2.0 1.5 1.0 DetemirHigh DetemirLow 0.5 Placebo 0.0 100 100 300 500 700 900 1100 1300 1500 Elapsed Time (min) Brunner et al. Exp Clin Endocrinol Diabetes. 2000;108. 21 GHb, FBG, and Nocturnal Hypoglycemia in Children With T1DM (Plus Regular Insulin) (N=349) NPH 8 6 18 4 2 p<0.05 6 % of Patients Change in GHB (%) and FBG (mmol/L) Glargine 0 -2 -6 Nocturnal Hypoglycemia* *Nocturnal hypoglycemia with FBG <36 mg/dL, month 2 to study end GHb FBG Schoenle et al. EASD 1999; Abst 883. Study 3003 Variable Basal Rate: CSII Program Plasma insulin Breakfast Lunch Dinner Bolus Bolus Bolus Basal infusion 4:00 8:00 12:00 16:00 Time 20:00 24:00 4:00 8:00 Year A1c by Treatment type at CHLA: 2000 2001 2002 2003 3 Injections BasalBolus CSII 8.1 ± 1.2 2004 2005 8.5 ± 1.5 8.4 ± 1.5 9.2 ± 1.7 8.8 ± 1.5 8.4 ± 1.5 8.4 ± 1.4 8.2 ± 1.4 8.1 ± 1.2 7.9 ± 1.2 7.9 ± 1.1 7.8 ± 1.0 7.6 ± 1.2 Outcomes of Pump Therapy Kaufman, et al, Diabetes Metabolism and Reviews,2000 6 month data 130 subjects PRE POST P value HbA1c % 8.4 + 1.8 7.8 + 1.2 0.01 BMI 22.8 + 4 23.2 + 5 NS Hypoglycemia 0.06 0.03 0.05 0.15 0.09 0.05 events/pt/y DKA events/pt/y Results of Insulin Pump Therapy In Young Children Kaufman, et al, Diabetes Spectrum, 2001 Pre Post P Value HbA1c 8.5+1.8 7.4+1.1 0.01 Mean BG 157+ 64 92 + 31 0.03 Hypoglycemia 0.18 0.09 ND Quality of Life Family Cohesion 82 + 6 90 + 5 0.009 A Randomized Controlled Trial of Insulin Pump Therapy in Young Children With Type 1 Diabetes Larry A. Fox, et al Diabetes Care 28:1277-1281, 2005 26 children randomly assigned to current therapy or CSII for 6 months, age 46.3 ± 3.2 months RESULTS— Mean HbA1c and BG did not change Frequency of severe hypoglycemia, ketoacidosis, or hospitalization was similar between groups Subjects on CSII had more fasting and predinner mild/moderate hypoglycemia All subjects continued CSII after study completion CSII in Young Children CONCLUSIONS CSII is safe and well tolerated in young children with diabetes and may have positive effects on QOL CSII did not improve diabetes control when compared with injections The benefits and realistic expectations of CSII should be thoroughly examined before starting this therapy in very young children CGMS Tracing Use of CGMS to Improve Clinical Care 13 47 Patients 29 girls Age years 11.8 ± 4.6 Duration years 5.5 ± 3.5 A1c start 8.61 + 1.51 A1c end 8.36 + 1.28 HbA1C (%) 18 boys, 12 11 10 9 8 7 6 Baseline 3 months post Sensor p=0.01 Kaufman, et al: Diabetes Care 24:2030, 2001. Mean Data for All Pts by Sensor 350 # of readings mean glucose level SD mean glucose 300 250 200 150 100 50 0 Ist Sensor 3rd Sensor 5th Sensor 7th Sensor Result Summary: Treatment Changes Basal (57%) Bolus (43%) 50% 45% 40% 42% 35% 30% 30% 25% 20% 15% 15% 10% 9% 5% 4% 0% Increase Basal Rate Decrease Basal Rate Increase in CHO Dose Increase in Correction Dose Percent of Total Changes Other Result Summary: Glucose Changes Subject #1 #2 #3 #4 #5 #6 #7 #8 #9 #10 A1c Start 7 6.9 9.4 7.5 7 8.3 9.3 8.8 8.2 8.3 A1c End 7.3 6.7 8.7 7.3 6.7 7.7 9.4 7.7 8.2 8.2 Daily Glucose Sensor 1-2 (First Week) 194 143 187 154 153 175 183 138 171 174 ± 55 ± 34 ± 23 ± 14 ± 23 ± 24 ± 21 ± 21 ± 31 ± 46 Daily Glucose Sensor 6-7 (Last Week) 182 120 172 163 145 138 167 123 177 169 ± 26 ± 21 ± 22 ± 38 ± 38 ± 28 ± 24 ± 25 ± 20 ± 31 HbA1c reduced from 8.1 to 7.8% after only 30 days Average glucose decreased from 167 to 156 mg/dl Question Why About the Risk of Hypoglycemia From Intensive Regimens? Intensive Management and Hypoglycemia HbA1c Association Is There Greater Risk of Hypoglycemia at Lower HbA1c Levels? Or with Intensive Regimens? Lack of Association Between HbA1c and Hypoglycemia Cox – no association in 78 pts with mean level of 10.25% Bhatia, Wolfsdorf – incidence of 0.12/pt/yr in 196 pts with HbA1 11.4% (nl 5.4-7.4) Daneman 16% of 311 pts with HbA1 of 8.7% Nordfelt, Ludvigsson – 146 pts intensive therapy, no increase in severe hypoglycemia Levinehighest HbA1c tertile, 36/pt/yr Kaufman et al Endocrinologist 9:342,99 Analysis of data to determine bedtime BG level 167 nights Analyze the number of glucose values <40 and < 50 mg/dl through the night Kaufman FR, et al, J Pediatr. 141:625-630, 2002. Results 45 nights (27%) – at least one reading < 40 mg/dl 59 nights (35%) – at least one reading < 50 mg/dl For nights < 100 at HS – 86.4 minutes No relation to A1c or regimen Kaufman FR, et al, J Pediatr. 141:625-630, 2002. Adverse Events in Intensively Treated Children and Adolescents with Type 1 Nordfeldt, Ludvigsson Acta Pediatr 88:1184,99 139 Subjects, ages 1-18 yrs on MDI Mean HbA1c 6.9% Severe Hypoglycemia - 0.17 events/pt/yr Decreased from 1-2 injections Correlated with previous severe hypoglycemia r=.38,p<0.0001 DKA rate 0.015 events/pt/yr MDI effective and safe How Well Are We Doing? Metabolic Control in Patients with Diabetes Thomsett, Shield, Batch, Cotterill J Pediatr & Child Health 35:479,99 Brisbane 268 < 19 yrs mean 11.2 yrs Duration 4.4 0-16 yrs Mean HbA1c 8.6+1.4%, range 5.2-14% Puberty 8.7+1.5%, Prepubertal 8.5+1.2% 33% < 8.0% HbA1c correlated insulin dose, duration Not correlated severe hypoglycemia, DKA, age, # of injections, # clinic visits Prediction of Hypoglycemia Good Predictors Weighted assessment of low BG for 2-3 wks Nighttime BG < 100-108 mg/dl Age < 5-7 yrs > 2 previous episodes Daily dose > 0.85 U/kg Duration > 2 yrs > 2 consecutive low BG in 2 wks > 4 BG < 50 mg/dl in 2 wks Poor Predictors Glycated hemoglobin level Number of insulin injections Intensive vs conventional treatment Kaufman et al Endocrinologist 9:342,99 Question What are the Developmental Issues of Young Children? Babies and Toddlers 0-3 Physical Rapid growth Erratic eating and sleeping Cognitive Differentiates self Learns language to represent objects/people Moral Development Judgments based on personal preference Preschool 4-6 Physical Greater mastery of gross and fine motor skills Cognitive Egocentric/Classifies objects by a single feature Magical thinking/Simple Moral Development Judgment of good/bad based on punishment/ reward Babies and Toddlers 0-3 Emotional and Sense of Self Begins to recognize that others' feelings are different from own Begins to have sense of self Social Parallel play Responsibility Total care by parents/ caretakers Preschool 4-6 Emotional and Sense of Self Sex role differentiation Likes to help Wants to do things by self Deference to authority Social Cooperative play Responsibility Child begins to have some responsibility with adult assistance Babies and Toddlers 0-3 Preschool 4-6 School At home/daycare Beginning to learn routines Adjusting to different caretakers School Entering school /Separation from parents Learning routines, rules outside of home School readiness skills Extra-Curricular Activities Babysitters Extra-Curricular Activities School aftercare Playdates Incentives Immediate and can be symbolic (stickers, stars, etc) Incentives Immediate and concrete Management Issues Babies and Toddlers 0-3 Preschool 4-6 Medication Regimen Choosing a regime to fit eating patterns and lifestyle Getting child to accept injections Requiring supervision in all settings Needing insulin coverage at preschool Pumps Picking the right catheter Finding the right catheter placement based on fat Using very small basal Choosing a person to be responsible for pump Child wanting to push buttons Testing Choosing sites for testing Checking overnight Selecting the right meter Having a small sample size Needing to include child in care Progressing to do own checks Avoiding labeling blood glucose "good" or "bad” CGMS Reducing anxiety about overnight hypoglycemia Evaluating basal bolus balance Checking overnight basal rates or long-acting insulin Hypo/Hyperglycemia Unable to tell caregiver when high or low May not cooperate with treatment Learning meaning of high/low BG Needing help in identifying symptoms Fearing hypoglycemia Insulin Administration and Adjustment Using very small doses Needing quarter units Requiring diluted insulin Minimizing pain and fear Having needle phobia Health & Sick Day Having more frequent vomiting and diarrhea Becoming dehydrated rapidly Needing immunizations Having more outside exposures Increasing number of sick days Contracting childhood illnesses Nutrition Breastfeeding makes measuring intake difficult Introducing solid foods Eating habits often erratic Using food as power struggle Grazing eating patterns Using artificial sweeteners may be controversial Needing to involve child in meal plan Exercise/Activity Growing very rapidly Becoming mobile Continuously in motion Energy level is high Case Study 1 Ana is a two-year old recently diagnosed Very spirited toddler Fights blood glucose testing by screaming, hiding and clenching her fists. What should this family do with this challenge? Issues by Developmental Status Challenges of Diabetes Management: Testing Factors Contributing to the Challenge: Normal Growth and Development Family Dynamics Developmental Tasks: Moral Development Emotional Development Incentives Solution Ana’s judgment about glucose testing based on personal preference – she did NOT like fingersticks Not possible to “convince” Ana she needs to test her blood Parents worked together and developed matter-of-fact attitude Committed to routine, no bargaining, stalling, chasing Parents provided immediate and concrete incentives - a hug, a “good job”, let her pick finger, read book as reward Picked meter capable of alternate site testing, very small sample and results in five seconds Within a very short time, Ana willingly participated Case 2 Terrel, 4-year old, type 1 for ten months and celiac disease BG testing 8-10 times per day, MDI, on gluten-free diet with few management problems at home Problems occurred in pre-school In school, regular episodes of hypoglycemia Continuous activity Not as much blood testing Skipped snacks related to less supervision What does family do? DEVELOPMENTAL ISSUES Challenges of Diabetes Management: Testing, Hypoglycemia, Nutrition Factors Contributing to the Challenge: Normal Growth and Development, School Developmental Tasks: Physical; Moral Development; Emotional Development; Responsibility; Incentives Solution At age four, Terrel likes to help, wants to do things by himself and adapts well to routines He is able to understand the meaning of low blood glucose and the importance of eating his carbohydrates In the school setting, he needs supervision while at the same time he needs to learn to take some responsibility for participating in testing and eating Incentives he likes - praise, stickers and providing choices Solution Every day before snack and recess After the snack Pick a small prize from a treasure chest Terrel liked being involved He was more inclined to eat and check BG test Choose a gluten-free snack provided by mother Getting a prize an extra incentive In a short time, this routine became the norm and hypoglycemia resolved Conclusion Ultimate Goals Of Diabetes Treatment Sustained Normal Blood Glucose Control Lowest Possible Incidence of Hypoglycemia = No Long-Term Diabetes Complications = No Acute Diabetes Complications Best Quality of Life with Diabetes For the child and your family