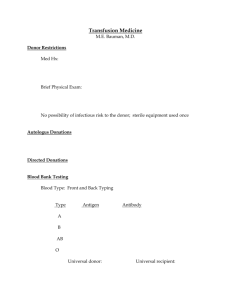
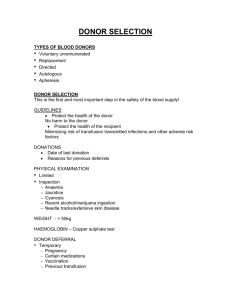
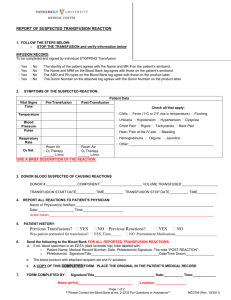
Delivering maternal health interventions among internally displaced
advertisement

The MOM Project: “Mobile Obstetric Medic” Maternal health interventions among IDPs in eastern Burma: Blood Transfusion Thomas Lee, MD MHS Director, Global Health Access Program (GHAP) Adj. Associate Professor of Medicine, UCLA School of Medicine Luke Mullany, PhD Director, GHAP Monitoring and Evaluation Assistant Professor, International Health / Center for Public Health and Human Rights Kate Teela, MHS MOM Project Coordinator Funding: Bill and Melinda Gates Institute for Pop and RH Eastern Burma Context Minimal access— CBOs only HRVs and conflict: 600k1,000k IDPs Limited mobility, long transit times IMR 91, U5MR 221, MMR 10001200 * *Lee T, Mullany L, et.al. TMIH 2006 MOM Project Rationale Ethnic minority CBOs – No bricks and mortar – Mobile clinics and “backpack” teams – Health workers Adapt RH interventions to existing service delivery models – Emphasis on mobility of providers to bring services to communities – Community-based providers with variable skill sets—training based on intervention MOM Selected Interventions BEOC – Kiwi, MVA, Magnesium, Misoprostol, Antibiotics, Manual removal placenta Focused ANC – Deworm, ITN, Malaria Screening, Fe/FA Clean Deliveries, PNC, Family Planning Transfusion 3-tiered provider network Maternal health workers (MHW) – 8 months training in RH department – Complex services (such as transfusion) Health workers (HW) – Some BEOC, ANC/PNC Traditional Birth Attendants (TBA) – Link between community and MHWs/HWs – Some basic services Transfusion Needs High Trauma: landmine-specific mortality rate = 1/1000 persons/yr Falciparum malaria prevalence >10% Malaria cause of death >40% Maternal anemia >60% (Hg<11) PPH leading cause of maternal death Transfusion Program Key Components Rapid diagnostic tests for low resource settings “Walking Blood Bank” concept – Blood taken from donors at time of need Community Education – Program acceptance, Donor Recruitment Transfusion Technical Issues Rapid Diagnostic Tests – Heat stability – Capillary blood vs plasma (centrifuge) – Adequate sensitivity No cross-matching (Type-specific) Blood typing “Walking Blood Bank” Donor list and map with blood types Donor recruitment during ANC: standby during time of delivery Not anonymous Counseling/treatment for screened diseases Donor screening Sequential testing – avoid testing for less treatable or more stigmatizing diseases – resource conservation Simultaneous testing for emergencies Goal of screening is blood safety, not necessarily diagnosis Conclusions Rethink appropriateness of limiting transfusion to referral centers (“Basic” vs. “Comprehensive” dichotomy) Transfusion may be easier than some elements of “Basic” EmOC Mobility of service provision to the population rather than centralized services accessed by the population Flexibility in “toolkit” for different types of providers Kiwi problems Technically challenging for health workers Inadequate training time Kiwi mechanical problems – Connection between pump and cup breaks too easily – Suction decreases with reuse – Belt loses consistency (too elastic) after decontamination – Too many pieces (multi-use model) Future Avenues One-sample donor screening test “Black-box” donor screening test – safe or unsafe Heat stability studies Thank you Partners Burma Medical Association Karen Department of Health and Welfare Shan Health Committee Karenni National Health Organization Mon Health Department Mae Tao Clinic Colleagues Palae Paw Lin Yone Eh Poh Eh Kalu Shwe Oo Cynthia Maung MOM Administrative staff Technical Advice/Oversight Luke Mullany Catherine Lee Kate Teela Nicole Franck-Masenior Chris Beyrer Funders Bill and Melinda Gates Institute for Population and Reproductive Health Hussman Foundation Foundation for the People of Burma Global Health Access Program Burma Border Projects