Triage competency - Lori Van Zoeren MSN, RN
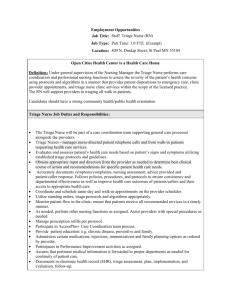
advertisement

L&D Triage Orientation Triage derived from French verb trier: To separate, sort, select Lori Van Zoeren BS, RN Ferris State University Objectives Identify skills and qualifications necessary for LD Triage Success Describe EMTALA and how it applies to the LD triage role Practice scoring patients for Medical Exam Screen and identify patients who require immediate provider evaluation Discuss supplies needed to assist providers in triage evaluation Assess and accurately interpret real life scenarios through case studies Evaluate the effectiveness of the orientation program ED triage skills for success Diverse knowledge base Multi-tasker under stress Strong interpersonal skills Ability to provide on-going Independent Effectively communicate Strong critical thinking Ability to perform a brief, focused interview and physical assessment Ability to make quick accurate decisions ENA, 2009 education Ability to work collaboratively Delegation ability Adaptability to fluctuations in workflow Understanding of the cultural diversity of not just patient but family L&D Triage Nurse Qualifications Successful L&D unit orientation At least two years of labor and delivery experience At least one year of labor and delivery experience at Bronson Emergency Triage VS OB Triage Prioritizing Case Study Patient presents with complaint of passing a plum sized clot at 37 weeks. Baby is active and there are no other risk factors communicated initially. Patient presents with complaint of a MVA two days ago and just wanted to make sure baby was alright. She is 28 weeks gestation and no other risk factors noted initially. Patient presents to triage at 18 weeks with complaint of lower back pain and cramping for 4 hours which has gotten progressively worse over the last hour. Patient states she is scared as she has lost a baby at 20 weeks due to incompetent cervix. What is EMTALA ? Emergency Medical Treatment and Active Labor Act Medical Exam Screen 250 foot rule Capability & Capacity Austin, 2011 EMTALA Violation Example Patient was evaluated and deemed in active labor at a hospital that did not deliver babies. Patient was allowed to be transported in friend’s car to the delivering hospital. The patient was delivered a few minutes after arrival and both mom and baby were fine. The hospital paid $40,000 dollars in civil monetary penalties for allegations that they failed to provide appropriate medical exam screening and stabilizing treatment as well as not providing appropriate transfer vehicle. Austin, 2011 Initial Documentation EMR requirements include the triage portion of the triage/admission tab in the EPIC chart Medical exam screen within 20 minutes Complex physical assessment PTA medications (prior to admission) Labor flow sheet with fetal monitor tracing interpretation and any interventions if indicated Consent for treatment signed upon arrival Allergies documented Medical Exam Screen Policy Screening within 20 minutes of arrival and again prior to discharge Patients scoring 10 or greater must be seen by a provider in a timely fashion Emergency Medical Condition Acute pain vs. regular contractions 10 minute fetal heart rate monitor Medical Exam Screen Scoring Patient presents to LD triage. SVE reveals: 2cm, 70% effaced, and -2 station. Membranes intact. Contractions are every 4 min, lasting 30-40 seconds, palpate mild, regular, no urge to push. Vital signs are: Temp 98.8, BP is 138/88, Resp 20. There is no edema of extremities but facial edema is present. Is having normal bloody show and FHT stable and reactive. Baby is vertex. Medical Exam Screen Scoring Patient presents to triage who is 38 weeks gestation with bright red bleeding like her normal periods. SVE deferred due to bleeding initially. She is having an occasional contraction, no urge to push, VS are stable, no edema. FHR is normal and reactive. Baby was vertex by Leopold's. Medical Exam Screen Scoring Patient presents to triage with complaint of abdominal pain that rates a 10 on the pain scale. She is writhing around in the bed to the point it is difficult to palpate for contractions. SVE reveals cervix that is 0 cm, 40% effaced, and 0 station. She states no leaking of fluid or bleeding, she is holding her breath like she is bearing down. BP stable, pulse is 110, Temp 100. No edema. FHR 110 with moderate variability and accelerations. Baby is vertex. Re-evaluation guidelines Pre-eclampsia-B/P every 15 if elevated, FHR every hour Labor evaluation- FHR every hour, VS every 4 hours Preterm labor- FHR every hour, VS every 4 hours Any abnormalities would indicate increased surveillance Med exam screen: Not always Non-emergency situations such as: Patients admitted directly into the hospital, bypassing triage. Betamethasone Injections or NSTs Austin, 2011 Success in L & D Triage Resources readily available Know your parameters Do you always have the backing to place orders? OB section/More to follow Order to do an SVE Do not be fooled Communication & Situation Background Assessment Recommendation (SBAR) Chain of Command Charge Nurse Unit Coordinator Manager Director CNO PAUL BERKOWITZ, MD (OB/GYN) CAMELIA MERATI, MD (Hospitalist) STEVEN POLLENS, MD (Family Practice) JOHN SIKORA, DO (Anesthesia) Stryker Gynnie Carts Know the supplies needed to assist providers in specimen collection Amnisure Review policy if not familiar Explain procedure (insert 2-3 inches into vagina and leave for 60 seconds) Insert swab into solvent and rotate swab for 60 seconds Properly label specimen and collect in Epic for the lab requisition Tube to lab as a stat and call 6440 to notify an Amnisure is coming for evaluation Amnisure Collection Inaccurate results can occur in the presence of: Meconium, antifungal creams, lubricating jelly, baby oil, Replens, expired solution, gross presence of blood, digital exams prior to swabbing, sample is collected greater than 12 hours after ruptured membranes Fetal Fibronectin No Prenatal Care “Abdominal” Pain Preterm Labor Term labor Epigastric Round ligament Kidney Ovarian Torsion Appendix Abruption Devarajan & Chandraharan, 2011 Underlying Pathology Area of Pain Organs to consider Possible causes Left Hypochondrial Spleen, pancreas, colon Splenic infarc, colitis Epigastric Stomach, pancreas, aorta, heart Gastritis, pancr, aortic dissection/mayocarditis/MI Right Hypochondrial Liver, Kidney, hepatic flex colon, gall bladder Liver issues, Fatty Liver of preg, HELLP, Pre-eclamp Right Lumbar Kidney, ascending colon Pyleo, renal calc, IBS Umbilical Trans colon, appendix, uterus Appy, gastro, pancreatitis, abruption, uterine rupture Left Lumbar Kidney, descending colon Pyelo, renal calc, IBS Left Iliac Sigmoid, Lt tube/ovary IBS, Ectopic, tube abscess or rupture, ovarian torsion Right Iliac Appendix, rt tube/ovary Appy, diverticulistis, above Supra-pubic Bladder, Uterus Cystitis,abrup, Scar rupt Devarajan & Chandraharan, 2011 Which of the following is not associated with abruptio placenta? Cocaine Heroin HTN Smoking Advanced Maternal Age Women under 20 years of age Abdominal trauma Alcohol Use Male fetus Chorioamnionitis Triage Imminent Delivery The infant warmer is in triage in the corner by the blanket warmer. Supplies are covered but is stocked with needed emergency supplies to deliver a baby in the triage area. Discharge Process Social Work Resources Coverage Cab passes Phone cards Child Life Domestic violence Drug Seeking Behavior Never chart that a patient is drug seeking Describe patient’s perception of her pain Document assessment of patient’s observable symptoms BE OBJECTIVE! MAPS report Case Study 1 41 year old G2 P1 30 week pregnant patient presents via ambulance to L&D triage. She was shopping and collapsed. She has no known medical conditions. She had an oral airway but spit out in route to hospital. Her VS are HR of 130, BP 190/110, Temp 97.3, Oxygen sat 93%, Glascow Coma scale 10/15. Case Study 2 25 y/o G2 P1 presents to triage with painless vaginal bleeding at 24 weeks. She had a previous cesarean section delivery. VS BP 130/78, Pulse 92, Resp 20, Temp 98.4. Case Study 3 Patient is 40 weeks gestation and presents to L&D triage in active labor. Fetal heart tones are 145. After asking if any bleeding or leakage of fluid you perform a SVE. Cervix is dilated 5 cm, 100% effaced, and -3 station. Patient rolled to left side and spontaneous ruptured membranes occurred. Fetal heart tones were then noted and verified at 70 bpm as patient’s pulse is 96. Case Study 4 Pt is a 20 year-old G3-P1 pregnant patient who complains of vaginal discharge which is especially prominent after intercourse. She states that it has a fishy odor. There is no bleeding and no regular contractions. VS are stable. She does complain of left lower quadrant pain that is constant. Case Study 5 Call from the ER received with report to expect an ambulance bringing in a G3, P2 patient who is 32 weeks pregnant involved in a multivehicle pile up. Patient is alert and oriented, her VS are stable, fetal heart tones are 150 with positive fetal movement. Case Study 6 A 31 year-old G4 P3 patient with twin gestation at 36 weeks presents to triage. When placed on cart she spontaneously ruptures membranes and there is a moderate amount of bleeding noted. Twin A now has fetal tachycardia and a sinusoidal heart rate pattern. Vasa Previa Case Study 7 Patient presents to L&D Triage with complaints of dizziness, headache, difficulty concentrating, pounding heart, tingling of the mouth, and feeling irritable. She is sweaty and pale. In Summary References Austin, S. (2011, June). What does EMTALA mean for you? Nursing, 41(6), 55-59. http://dx.doi.org/10.1097/01.NURSE.0000398175.36147.bc Bronson Methodist Hospital website .(2014). https://inside.bronsonhg.org/ Devarajan, S., & Chandraharan, E. (2011). Abdominal pain in pregnancy: A rational approach to management. Obstetrics, Gynaecology, and Reproductive Medicine, 21(7), 198-206. http://dx.doi.org/10.1016/j.ogrm.2011.04.001 Emergency Nurses Association. (2011). Triage qualifications. Retrieved from http://www.ena.org/SiteCollectionDocuments/Position%20Stat ements/TriageQualifications.pdf Project Goals and Objectives Goal: To develop an orientation program for labor and delivery triage nurses at Bronson Methodist Hospital in Kalamazoo, MI Objectives: 1.1 Identify recommended LD triage nurse competencies required to care for the obstetrical patient population. 1.2 Provide an educational program for nurses who work in LD triage on skills needed for competency that are unique to triaging obstetrical patients. 1.3 Evaluate the effectiveness of the orientation program for staff. 1.4 Preceptor evaluation of the attainment of the proposed goals of the scholarly project. 1.4 Selfevaluation of the attainment of the proposed goals of the scholarly project. 1.5 Revise orientation program based on evaluation results. Personal & Professional Accountability Adherence to NLN Nurse Educator Competencies Performed a comprehensive literature search Assimilated knowledge from lit review Applied new knowledge to the triage orientation program Followed project plan utilizing time management skills Project Outcomes Increased knowledge of EMTALA and the legal ramifications Increased knowledge of the differences between ER triage and LD triage BMH standards discussions for triage competency Collaboration discussions with area hospitals Hands on activities provided new knowledge of assisting providers with obtaining cultures Project Evaluation Do you have a better understanding of EMTALA? Was the PPT beneficial to learning about LD triage role? Did the PPT provide new knowledge? Do you feel the importance of the Medical Exam Screen was thoroughly explained? Do you believe you can correctly prioritize patients listed in case studies? Do you believe the objectives of the LD orientation and competency validation program were met?