INTEGUMENTARY SYSTEM
advertisement

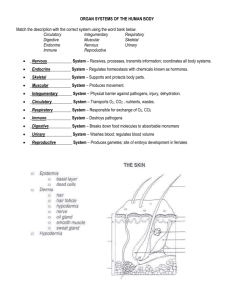
INTEGUMENTARY SYSTEM HONORS ANATOMY & PHYSIOLOGY CHAPTER 5 HUMAN ANATOMY & PHYSIOLOGY Integumentary System Includes: Skin Nails Hair Sweat & Oil Glands FUNCTIONS 1. Protection: chemical barriers: skin secretions: acidic: hostile to most bacteria some bactericidal melanin: chemical pigment shield protects DNA from damage by UV rays physical barrier: continuity of skin & hardness of keratinized cells stratum corneum: multiple layers of dead cells (brick) and water-resistantglycolipids (mortar) Substances that Penetrate Skin 1. 2. 3. 4. 5. 6. lipid-soluble substances: )2, CO2, Vit A,D,E,K oleoresins: poison ivy, poison oak organic solvents: acetone, dry-cleaning fluid, paint thinner all dissolve cell lipids heavy metal salts: Pb, Hg selected drugs: nitroglycerine, nicotine, fentanyl, seasickness meds, estrogen penetration enhancers: help carry other drugs into body thru skin Functions – Protection cont’d 3. Biological Barriers: dendritic cells of epidermis active elements of immune system agn presenting cells dermal macrophages phagocytes viruses or bacteria agn presenting cells DNA e- can absorb some UV rays heat Functions of Skin -2 body temperature homeostasis when body overheated blood flow to skin increases & some heat radiates off body, sweating (sensible losses) when body cold less blood flows to skin, more to trunk, goose bumps @normal temps sweat glands lose ~500 mL/dthru insensible losses Functions of Skin - 3 Cutaneous Sensation (sensory receptors): exteroceptors: sense stimuli from outside body Meissner’s corpuscles: in dermal papilla, feel light touch Pacinian corpuscles: deep dermis or hypodermis, feel deep touch hair follicle receptors: feel breezes, insect free nerve endings: pain from irritants or extreme cold or heat Functions of Skin - 4 Metabolic Functions: 1. 2. 3. Sun light nrg powers some chemical reactions: modified cholesterol Vit D precursor keratinocyte enzymes “disarm” cancer-causing chemicals activate some steroid hormones (cortisone cream cortisol a more potent anti-inflammatory) synthesize important proteins collagenase Functions of Skin - 5 Blood Reservoir dermal vessels can hold up to 5%of blood vol. vessels constricted when other organs need extra blood constriction shunts blood to areas in need Functions of Skin- 6 excretory function: sweat contains urea, uric acid (breakdown products of proteins) NaCl + water lost with profuse sweating Structure of the Skin made of 2 kinds of tissues 1. Epidermis 2. Dermis Epidermis made of stratified squamous epithelium some keratinized, some not avascular Cells: Keratinocytes majority of cells make keratin Melanocytes Langerhans Cells Immune System aka dendritic cells Cells of the Epidermis Epidermal Layers 1. stratum basale deepest layer constantly undergoing cell division/ cells pushed upward 2. stratum spinosum 3. stratum granulosum 4. stratum lucidum (only in thick skin) clear, flatter, more keratin 5. stratum corneum (cornified = keratinized) outermost layer/ 20-30 dead cells thick Layers of Epidermis Thick Skin areas subject to abrasion palms soles finger tips Thin Skin covers rest of body thinnest skin (thinner subcutaneous layer) eyelid: 0.02mm bridge of nose ankles knuckles Melanin pigment (yellow to brown to black) produced by melanocytes most are in stratum basale cells stimulated to make more melanin when skin exposed to sunlight shields DNA from damaging effects of UV radiation freckles & moles: seen where melanin concentrated in 1 spot Freckle Dermis a strong, stretchy envelope that helps to hold the body together leather is the dermis of whatever animal it was made from made of dense CT: strong& flexible rich blood supply 2 regions: 1. Papillary 2. Reticular Papillary Layer upper dermis dermal papillae: uneven projections into lower epidermis that contain: 1. capillaries 2. pain receptors 3. touch receptors: Meissner’sCorpuscles 4. in thick skin: form ridges (fingerprints) that improve gripping ability genetically determined Dermal Papillae Dermis: Reticular Layer deepest skin layer Contains: 1. sweat & oil glands, hair follicles, blood vessels 2. Pacinian corpuscles (deep touch receptors) 3. many phagocytes 4. fibers: elastic: give young skin elasticity collagen: make dermis tough & keeps skin hydrated by binding to water Dermis Striae extreme stretching of skin white scars aka stretch marks Blisters fluid –filled pocket separating epidermis/dermis Skin Color 3 pigments contribute to skin color: 1. Melanin amount & kind (yellow black) 2. Carotene orange – yellow pigment stratum corneum & subcutaneous layers 3. Hemoglobin amount O2 bound to it in RBCs in dermal blood vessels has greater affect in light skinned people Skin Color in Sickness & in Health cyanosis: blue hue to skin; due to poorly oxygenated blood erythema: redness, due to increased blood flow (infection, inflammation); burn, HT, blushing pallor: paleness, due to emotions, anemia, low BP, decreased blood flow jaundice: yellow; usually from liver disease (not clearing bilirubin) hematomas: bruising (bleeding under skin) Appendages of the Skin derivatives of epidermis: hair& hair follicles nails sweat glands sebaceous glands Hair & Hair Follicles areas of skin with no hair: palms soles lips nipples parts of external genitalia Functions of Hair sense insects b/4 they bite protects against heat loss (scalp) protects against sun shield eyes filter air inhaled through nose Hair “pili” produced by hair follicles consist of dead keratinized cells keratin here compared to keratin in epidermis: tougher & more durable individual cells do not flake off Hair 3 concentric layers of keratinized cells 1. Medulla innermost large cells & air space absent in fine hair 2. Cortex surrounds medulla layers of flattened cells 3. Cuticle 1 layer overlapping cells provides strength Hair Pigment melanocytes @ base of follicle to cortical cells differing proportions of melanins of different colors give different hair colors melanin production decreases (delayed-action genes) replaced by air bubbles gray white Hair Follicle fold down from epidermis dermis forming hair bulb sensory nerve ending : root hair plexus surrounds hair bulb bending hair stimulates plexus sensitive touch receptors Hair Follicle dermal papilla: bit of dermal tissue protruding into base of follicle capillaries matrix: actively dividing cells produces hair arrector pili: smooth muscle from dermal part of follicle epidermis @ angle contraction goose bumps Types of Hair VELLUS TERMINAL pale, fine hair coarse long hairs children and females eyebrows, scalp @ puberty: Factors the Influence Hair Growth Nutrition poor nutrition poor growth 2. Hormones 3. local inflammation increased growth 1. normal growth~2.5 mm/wk fastest growth teens 40’s then slows each follicle goes thru cycle: 1. active growth phase wks yrs 2. regressive phase 3. matrix cells die resting phase 1 – 3 mos Hirsutism excessive hairiness could be from ovarian or adrenal gland tumor secreting high levels of androgens Alopecia hair thinning starts @ anterior hairline posteriorly males: by age 35: 40% by age 60: 85% Male Pattern Baldness most common type of baldness X-linked recessive inheritance: delayed-action gene switches on in adult & changes hair follicle response to testosterone follicles very short growth cycle may get vellus hair Alopecia Areata immune system attacks hair follicles hair falls out in patches Nails scalelike modification of epidermis forming clear protective covering on dorsal surface of distal digits hard keratin Functions: 1. pick up small objects 2. scratch 3. protect tips of digits Parts of a Nail 1. free edge 2. nail plate or body 3. nail bed proximal portion = matrix: nail growth 4. proximal root 5. nail folds: proximally :eponychium (cuticle) Nail Abnormalities yellow: thyroid or respiratory problem thickened yellow: fungus infection outward concavity: iron deficiency (spoon nail) horizontal lines: malnutrition Sweat Glands aka sudoriferous glands over entire skin surface except: nipples parts of external genitalia 2 types: 1. Eccrine Sweat Glands 2. Apocrine Sweat Glands secretory cells surrounded by myoepithelial cells: contract when stimulated by nervous system sweat goes thru duct to skin Eccrine Sweat Glands more numerous than apocrine abundant on palms & soles of feet secretory cells in dermis sweat released thru pore (not skin pore) Eccrine Sweat Gland secretion: hypotonic (99% water) filtrate of blood also has: salts vitamin C abys wastes: urea, uric acid, NH3 Eccrine Sweat Gland regulated by sympathetic division of ANS Functions: 1. prevent overheating forehead spreads inferiorly 2. “emotional” sweating fright or extreme nervousness palms, soles, or axilla over body Apocrine SweatGlands axillary & anogenital areas only larger than eccrine glands found deeper in dermis/hypoderrmis empty onto hair follicle odorless until released onto skinwhere bacteria decompose molecules musky, unpleasant odor in addition to what is found in eccrine sweat: fatty acids proteins Apocrine Sweat Glands begin functioning @ puberty activated by sympathetic division of ANS during: pain stress exact function uncertain but likely analogous to animals glands that secrete pheromones Ceruminous Glands modified apocrine glands secretion mixes with sebum (made by sebaceous gland) cerumen (ear wax) Function: deters insects blocks entry of foreign objects Mammary Glands specialized sweat glands that secrete milk Sebaceous Glands oil glands found with hair follicles smaller on trunk & limbs large on face, neck, upper chest secrete sebum: oily substance develop as outgrowths of hair follicle arrector pili contractions force sebum to skin surface androgens stimulate secretion (activity starts in puberty) Sebum Functions: 1. softens & lubricates skin & hair 2. bactericidal action Whitehead created by: sebum blocks sebaceous gland duct Blackhead sebum in whitehead oxidizes Acne active inflammation of sebaceous glands see: pustules or cysts on skin surface associated with bacterial infection (staph) Skin Cancer Benign tumors such as warts and moles are not serious. Malignant tumors can start on the skin and invade other body areas. Crucial risk factor- overexposure to UV radiation Skin Cancer 20% in USA will develop skin cancer (↑ing #s) #1 risk factor: Sun UV radiation DNA damaged suppresses tumor suppressor gene new skin lotions contain liposomes initiate repairof damaged DNA Types of Skin Cancer Basal cell carcinoma- most common, 30% of all white skin people get it. Arises from the stratum basale layer of the skin 99% curable if caught early Dome shaped nodules that form an ulcer in the center. Squamous Cell carcinoma Arise from stratum spinosum Grows rapidly and metastasizes if not removed Small red rounded elevation on the skin Basal Cell Carcinoma Lesion removed from patient Basal Cell Carcinoma Squamous cell carcinoma Skin Cancer Types cont. Melanoma Cancer of melanocytes (very dangerous) 5% of skin cancers but rising fast Can arise from preexisting moles Appears as a spreading brown or black patch Chance of survival is poor if the lesion is greater than 4 mm thick Melanoma What is the ABCD rule? Used for recognizing melanoma A-Asymmetry: two sides of the pigmented mole do not match B-Border irregularity: borders are not smooth C- Color: lesion has a multiple of colors D- Diameter the spot is larger than 6 mm in diameter (size of a pencil eraser) What are the 3 types of burns? First-degree burns: only the epidermis is damaged. Redness, swelling and pain are common. (sunburn) 2-3 days to heal Second-degree burns: epidermis and upper layers of dermis. Blistering can occur. 3-4 weeks to heal. Third-degree burns: involves the entire thickness of the skin. (pg. 164-165) Second-degree burns Third-degree burn Burn Evaluation Rule of 9’s: divides body into11areas each 9% of body surface area + 1% for genitalia Burn Treatment patients require extra calories to replace lost proteins & allow tissue repair must add parenteral nutrition (IV) 2◦ infections main threat 24 hrs after burn wound is sterile fungi, bacteria,& other pathogens multiply rapidly Immune system deficient infection leading cause of death in burn victims Burn Treatment: Skin Grafts 1st debride burned tissue wash area with antibiotic in solution apply synthetic membrane temporarily skin graft: healthy skin applied to area autograft: taken from the patient synthetic skin: silicone “epidermis” bound to spongy “dermis” made of collagen fibers & ground cartilage patients own cells absorb &replace synthetic * no rejection from immune system Think About It