Factors involved in Normal Digestion and Absorption of Food
advertisement
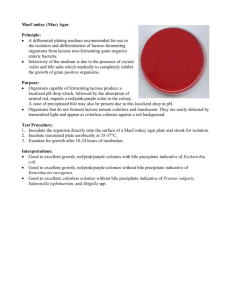
MALABSORPTION פרופ' יוסף צימרמן גסטרואנטרולוגיה המרכז הרפואי של הדסה והאוניברסיטה העברית ,עין כרם ,ירושלים MALABSORPTION • GENERALIZED: Non specific impairment in the absorption of multiple nutrients; Pancreatic insufficiency Short Bowel Syndrome • SPECIFIC: Impairment of digestion or absorption of a single nutrient; Lactase deficiency When Should We Suspect Malabsorption? • Nutritional deficiencies (anemia, osteoporosis), mainly if dietary intake appears appropriate; • Weight loss; • diarrhea; Malabsorption: Physical Signs • Non specific: wasting, bloated abdomen, edema and signs of specific nutrient deficiency (glossitis, angular cheilosis, petechiae, etc.) • May suggest a diagnosis (clubbing in small bowel disease etc.) Pathophysiology • LUMINAL FACTORS (MALDIGESTION) • MUCOSAL FACTORS Impaired hydrolysis (dissacharidases, peptidases) impaired transport; • POST MUCOSAL FACTORS Vascular Lymphatic Dietary Fat is Mostly Triglyceride (TG) TG DIGESTION: GASTRIC PHASE • Initial hydrolysis by the lingual and gastric lipases. • These lipases, unlike the pancreatic lipase, are active at an acid pH (4.5-5.4) and hydrolyze TG to diglyceride and free fatty acid (FFA). • While their contribution to overall fat digestion in the normal adult is small, they are important in neonates and in patients with cystic fibrosis. LIPID EMULSIFICATION IN THE STOMACH • Dietary fat, which is partly hydrolyzed by gastric and lingual lipases, is dispersed in the gastric contents in small droplets, creating a lipid emulsion. The motor activity of the antrum is essential in this process. • The emulsion is stabilized by FFA’s released from dietary TG through the action of the lingual and gastric lipases in the stomach . GASTRIC EMPYING • Delivery of chyme from the stomach is delicately adjusted so it enters the duodenum at a controlled rate, allowing mixing with pancreatic secretions and bile. • Control of gastric emptying is thus critical to ensure optimal digestion. Stages of Fat Digestion and Absorption: Intestinal Phase • Hydrolysis (pancreatic lipase); • Solubilization in bile salt micelles; • Transport across the luminal membrane of the enterocyte; • Resynthesis of TG in the enterocyte; • Incorporation of TG into chylomicrons; • Elimination of the chylomicrons by the lymphatic system Triglyceride Hydrolysis by Pancreatic Lipase + 2 FFA Properties of the Pancreatic Lipase • • • • • • Secreted in active form (not proenzyme); Interfacial enzyme, positional specificity; Secreted in great excess; Optimum activity at pH ~6; Destroyed by acid (pH<3); Requires co-lipase; Bile Salt Micelle formation • In order to solubilize fat, bile salts must form micelles; • The formation of micelles depends on the concentration of bile salts, and occurs when their concentration is > 1.5 mmol/L (CMC). • Normally, the bile salt concentration in the duodenum during meal is 5-10 mmol/L. FUNCTIONS OF INTRALUMINAL BILE SALTS • Micellar solubilization of fat-soluble vitamins (A,D,E,K)-essential for their absorption; • Micellar solubilization of fatty acids and monoglycerides; • Protection of pancreatic lipase against tryptic digestion. CHYLOMICRON CLEARANCE FROM THE INTESTINE • Normally, fat absorption is completed in the upper 2/3 of the jejunum. • Fat malabsorption may result from the following: Defective mixing; Reduced solubilization; Decreased lipolysis; Decreased mucosal absorption and chylomicron formation; Defective lymphatic transport of chylomicrons; CONSEQUENCES OF FAT MALABSORPTION • • • • Steatorrhea; Weight loss; Diarrhea; Deficiency in fat-soluble vitamins; STEATORRHEA Sudan Stain Test : A Qualitative Fecal Test for Steatorrhea FAT BALANCE: THE TEST FOR STEATORRHEA Chemical determination of fecal fat excretion on a defined fat intake (70-100g/day). Requires a complete collection of stools during the study period (24-72 hours). Normally, 95% of dietary fat is absorbed and fecal fat excretion is≤ 5 grams/day on a 100 gram-daily fat intake. The test is not specific as to etiology. Disturbances in the Enterohepatic Circulation of Bile Salts • Liver Disease; • Bile ducts; • Small bowel: Malabsorption Deconjugation Binding or precipitation BILE SALT MALABSORPTION: CAUSES • Ileitis (Crohn’s disease); • Surgical resection of ileum; • Idiopathic BILE SALT MALABSORPTION: CLINICAL FEATURES • Diarrhea; Bile salts; Hydroxy Fatty acids • Steatorrhea; • Cholesterol gallstones; • Enteric hyperoxaluria Oxalate nephrolithiasis Bile-Salt-Induced Diarrhea • Malabsorption of bile acids results in an increased concentration of bile salts in the colon. • At concentrations >1.5 mmol/L, DIHYDROXY bile salts inhibit electrolyte absorption and stimulate secretion by the colonic mucosa. FATTY ACID-INDUCED DIARRHEA IN BILE ACID MALABSORPTION In the absence of micelles, unabsorbed free fatty acids reach the colon. FORMATION OF HYDROXY FATTY ACIDS FROM UNSATURATED FATTY ACIDS + H 2O HYDROXY STEARIC ACID OLEIC ACID Ricinoleic acid Ricinoleic Acid, a laxative acting by increasing intestinal Secretion of water Treatment of Diarrhea Caused by Bile Acid Malabsorption • Bile salt binding agents- cholestyramine. Cholesterol Gallstone Formation in Bile Salt Malabsorption • Cholesterol solubility in bile (aqueous solution) depends on the concentration of bile salts. • Bile salt depletion reduces the solubility of cholesterol in bile, which precipitates out and forms gallstones in the gallbladder. Bile Salt Malabsorption and Nephrolithiasis Oxalate Mechanism of urinary oxalate stones formation in bile acid deficiency • Oxalate in food is usually precipitated out as Calcium oxalate in the lumen and is lost in the stool. • When lipolysis is normal and bile salts concentration is <critical micellar concentration, unabsorbed longchain fatty acid compete with oxalate for calcium; • Consequently, a large amount of oxalate is lost to the colon, where it is passively absorbed and ultimately excreted in the kidneys. Oxalate Crystals in the Urine Disturbances in the Enterohepatic Circulation of Bile Salts • Liver Disease; • Bile ducts; • Small bowel: Malabsorption Deconjugation Binding or precipitation Bile Salt Deconjugation • Bile salts are secreted from the liver as conjugates with either glycine or taurine. • The conjugation increases the acidity of the bile salt and makes it more hydrophilic1. • The conjugation decreases passive diffusion of the bile salts in the jejunum and maintains a high intraluminal concentration. 1. pKa of unconjugated bile acid≈5; of glycine conjugates ≈ 3.9; of taurine conjugates ≈2.0. • Deconjugation of bile salts may occur when bacteria colonize the proximal small bowel. • Normally, such colonization is prevented by 2 factors: GASTRIC ACID; MOTILITY OF THE SMALL BOWEL; Bacterial counts and Luminal pH in the Human Alimentary Tract •Duodenum : •Jejunum: •Ileum: •Cecum Count 102-1003/ml 102-1003/ml 108/ml 1010-1011/ml pH 5.5-6.0 6.0-6.5 6.5-7.0 Small Bowel Bacterial Overgrowth (SIBO) • Achlorhydria or hypochlorhydria: (PPI treatment; atrophic gastritis; postoperative stomach). • STASIS: Motility disorder: diabetic autonomic neuropathy, scleroderma, chronic intestinal pseudoobstruction). Anatomical changes: Strictures, small bowel diverticula, fistula, blind loop. CROHN’S DISEASE: ILEAL DISEASE AND FISTULAE Clinical Features of SIBO • Underlying disease; • Deconjugation of Bile salts: Steatorrhea (15-30 gram/day). Deficiency of fat-soluble vitamins; • Anemia, usually macrocytic Deficiency of vitamin B12; Normal or elevated serum folic acid levels; Occasional iron deficiency; • Hypoalbuminemia; SIBO-DIAGNOSIS • “Gold Standard”: Aspiration of duodenojejunal fluid with culture and bacterial counts. • Presence of >105 CFU/mL is diagnostic for SIBO. • This test is not routine performed because it is invasive and complicated. SIBO-DIAGNOSIS: Breath Tests • Principle: bacteria are able to produce H2 after metabolizing a sugar. • Bacterially-produced H2 is eliminated via the lungs and can be detected in the expiratory air. • An increase of 20 ppm over baseline after ingestion of glucose is considered diagnostic of SIBO. • The glucose breath test has a sensitivity of 62% and a specificity of 83% for SIBO. SIBO-TREATMENT • Antibiotics-broad spectrum; In blind loopmetronidazole; • Rifaximin- a non absorbable antibiotic is effective at a dose of 400 mgx3/daily for 14 days; • Recurrences are common and repeated courses of treatment may be necessary.