Lynn Gettrust BSN, RN
Alverno College-MSN student
Tutorial Project
Spiritlynnrn@netscape.net
Use the navigation arrows at the bottom of a page to
move between pages of the tutorial:
Clicking on
sends you to the home page
Clicking on
sends you to the next page
Clicking on
sends you to the previous page
Click on the Emesis Basin to learn about a specific objective
At the end of the tutorial you will know the:
Incidence of postoperative nausea and vomiting (PONV)
Pathophysiologic process involved in the development of PONV
Inflammation, stress response, and genetics in the development
of PONV
Risk factors associated with the development of PONV
Potential complications of PONV
Medical, nursing and complimentary treatments currently
available to manage PONV
Case Study
References
PONV occurs in 30% of patients overall, 70% of high
risk patients
Patients prioritize vomiting as the top adverse reaction
in anesthesia to avoid
PONV is unpleasant and associated with patient
discomfort /dissatisfaction with their perioperative
care
30% of ambulatory patients experience post discharge
nausea and vomiting (PDNV)
All clipart from
Wender, 2009
microsoft.com
unless otherwise
noted
Financial Impact
Average of $618 per patient is incurred today from a
single episode of PONV, even without unplanned
admission
Consequences of unplanned admissions
Detract from goal-same day discharge
Inconvenience to patients/families
Results in lost wages/missed work time
Increases cost to hospital-additional drug treatment/nursing
care
Kloth, 2009
Answer True or False to the following questions
Click on the correct answer
1.
True or False-Patients prioritize vomiting as the top
adverse reaction in anesthesia to avoid
2.
True or False-PONV may result in unplanned
hospital admission resulting in lost wages and
missed work for patients
Definitions
Nausea is a:
Sensation associated with awareness/urge to vomit
Subjective, unpleasant feeling in upper stomach and/or back
of throat
Patient descriptors-feel sick to my stomach, feel queasy, feel
squeamish
Autonomic symptoms-pallor, diaphoresis, tachycardia,
salivation
ASPAN’S Evidence-Based
Clinical Practice
Guideline-PONV/PDNV2006
Definition
Retching
Attempt to vomit without expelling any material
Involves labored spastic respiratory movements against a
closed glottis with rhythmic contractions of the abdominal
muscles, chest wall and diaphragm
Retching can occur without vomiting but normally generates
enough pressure to produce vomiting
Patients describe this as dry heaves
ASPAN’S Evidence –Based
Clinical Practice GuidelinePONV/PDNV-2006
Definition
Vomiting
Forceful expulsion GI contents
Caused by powerful, sustained contractions abdominal/
chest wall musculature, accompanied by descent of
diaphragm and opening of gastric cardia
Reflux activity not under voluntary control
Autonomic symptoms-pallor, tachycardia, diaphoresis
Patient descriptors-puking, throwing up, tossing my cookies,
barfing
ASPAN’S Evidence-Based Clinical
Practice GuidelinePONV/PDNV-2006
Muscular Contractions Associated with
Nausea and Vomiting
Copyright 2004,
Amdipharm plc, All rights
reserved
PONV is nausea or vomiting that occurs within the
first 24 hour period after surgery
3 phases
Early PONV-Occurs within first 2-6 hours after surgery, often
in PACU
Late PONV-Occurs in 6-24 hour period after surgery, often
after transfer to floor or unit
Delayed PONV-Occurs beyond 24 hours postoperatively in
the inpatient setting
ASPAN’S Evidence-Based Clinical
Practice Guideline-PONV/PDNV-2006
Nausea and vomiting are protective reflexes
Physiologic protective mechanism, limits possibility of
damage from ingested noxious agents by emptying
contents of stomach and portions of small intestine
May represent a total body response to a multiplicity of
causes including pregnancy, motion, drugs and
surgery.
www.nausea and vomiting co.uk
2004
Answer True or False to the Following Questions
Click on the Correct Answer
1.
True or False-Vomiting is a reflex activity under
voluntary control
2.
True or False-PONV is divided into three phases,
early, late and delayed
3.
True or False-Nausea and vomiting are physiologic
protective mechanisms to limit damage from toxins
Schematic representation of factors and body systems
involved in nausea and vomiting process
© Copyright 2004,
Amdipharm plc. All
rights reserved
Pathophysiology
Vomiting Center
controls act of
vomiting-located in
medulla oblongata of
the brain
Medulla is at base of
brain, formed by
enlarged top spinal
cord
Medulla contains
cardiac, vasomotor
and respiratory
MEDULLA
www.anomalocaris.net
centers of brain
Mattson-Porth,
2005
Vomiting center- not a discrete
anatomical site-represents nerve
network that receives input from
different areas in body
Controls vomiting, when activated,
sends signals to salivary,
respiratory centers, pharynx,
stomach/intestinal muscles
Signals result in vomiting
Wilhelm et al, 2007
Copyright 2004,
Amdipharm plc. All
rights reserved
Nerve pathways:
Input to vomiting center
from body carried on
afferent nerve pathways.
Input from vomiting
center to areas that
initiate actual vomiting
reflex carried on efferent
nerve pathways.
www.nlm.nih.gov
www.nauseaandvomiting.co.uk
2004
Chemoreceptor Trigger
Zone located in fourth
ventricle brain
Chemoreceptorsensory nerve activated
by chemical stimuli
www.nauseaandvomiting.co.uk
2004
Copyright 2004, Amdipharm plc. All
rights reserved
Chemoreceptor Trigger Zone (CTZ)
Located outside blood brain barrier
Major chemosensory organ for emesis-usually associated with
chemically induced vomiting.
Blood-borne/cerebrospinal fluid toxins have easy access to
CTZ.
CTZ can be affected by anesthetic agents/opioids
Provides input to vomiting center
DiPiro , 2005
Answer True or False to the following questions
Click on the correct answer
True or False-The vomiting center in the medulla
controls the act of vomiting
2. True or False-A chemoreceptor is a sensory nerve
activated by movement
3. True or False-The CTZ is outside the blood-brain
barrier and is usually associated with chemically
induced vomiting
1.
Input to vomiting
center:
GI Tract
Input comes from
stomach, jejunum,
ileum
Input travels on
visceral afferent
vagus nerve
www.nauseaandvomiting.co.uk 2004
Two types of receptors in the GI organs are involved in
detecting vomiting producing stimuli
Mechanoreceptor
Sensory nerve in muscular wall gut-responds to mechanical
stimulation
Examples-touch, pressure, muscular contractions
Tension receptors-send input to vomiting center in response
to distention or contraction
www.nauseaandvomiting.co.uk 2004
www.illustrationsof.com
Chemoreceptor
Sensory nerve cell activated by chemical stimuli
Located in mucosal layer of GI tract
Triggered by noxious substances in luminal
environment
Respond to a variety of toxins
When toxins cause irritation to GI tract, information
travels to CTZ and vomiting center which may initiate
vomiting reflex.
www.nauseaandvomiting.co.uk
2004
Input to vomiting center:
Cerebral cortex
Layer of neurons and
synapses (gray matter) on
surface of cerebral
hemispheres.
Mattson-Porth, 2005
Cerebral Cortex
Function-to integrate higher mental functions, general
movements, visceral functions, perception, speech and
memory patterns.
Higher cortical effects can stimulate or suppress nausea
and vomiting
Prefrontal cortex-responsible for planning, problem solving,
intellectual insight, judgment, expression of emotion. May
send input to vomiting center regarding past memories,
fears, anticipation associated with vomiting.
Example-Patient arrives anxious and fearful , states “I always
vomit after surgery.”
Mattson-Porth, 2005
Parietal lobe
Integrates/processes sensory
information from various parts
body
In parietal lobe sensory
experiences begin to form into
cognitions experienced as
thinking in frontal lobes
Sensory input from nausea and
vomiting integrated here.
www.howstuffworks.com
Mattson-Porth, 2005
Answer True or False to the following questions
Click on the correct answer
1.
True or False-A mechanoreceptor is a sensory nerve
ending that responds to distention
2.
True or False-Input to the CTZ and vomiting center is
carried on visceral efferent nerve pathways
3.
True or False-The parietal lobe integrates and
processes sensory input
Input to vomiting center:
Vestibular apparatus
Consists of peripheral
apparatus and CNS
connections
Peripheral apparatus- 5 parts:
three semicircular canals, a
utricle and saccule
Copyright © 1996-2005, WebMD,
Inc. All rights reserved
Mattson-Porth, 2005
Vestibular apparatus
Inner ear structures associated with balance/position
sense-maintains head/body position through reflex
control and stable visual field despite head
movements
Vestibular nerve fibers carry information from inner
ear to vestibular nuclei.
Vestibular nuclei has neurons that project to thalamus
and temporal and sensory areas of parietal cortex.
Mattson-Porth, 2005
Thalamic and cortical projections of vestibular apparatus
provide basis for subjective experience of
position/rotation/dizziness.
Vestibular system can stimulate PONV as a result of
surgery involving middle ear or postoperative movement.
Sudden head movement after surgery, leads to vestibular
disturbance, and increased incidence of PONV
Mattson-Porth, 2005
Neuromediators
Neurotransmitters are chemical
messenger molecules of
nervous system.
Neurotransmission involves
development, storage, and
release of a neurotransmitter;
reaction of neurotransmitter
with its receptor site, and
termination of receptor action
DiPiro , 2005
Numerous neurotransmitters are located in vomiting
center, CTZ, GI tract
Examples-cholinergic, histaminic, dopaminergic,
opiate, serotonergic, neurokinin, benzodiazepine
receptors
Emetic compounds (chemotherapy drugs, narcotics),
theoretically trigger vomiting process through reaction
of emetic compound with its receptor site
Effective antiemetics are able to block or antagonize
emetogenic receptors
DiPiro , 2005
Chemoreceptor
trigger zone and
cerebral cortex
Vestibular
apparatus
Visceral
afferent nervesGI tract
Central
vomiting center
Salivary
center
Respiratory
center
VOMITING
Pharyngeal/GI/
abdominal
muscles
Diagram representing
nausea and vomiting
pathways
Answer True or False to the following questions
Click on the correct answer
1.
True or False-The vestibular apparatus is the inner
ear structures associated with balance/position sense
2.
True or False-Neurotransmitters are the chemical
messenger molecules of the nervous system
3.
True or False-Neurotransmitters bind to receptor
sites to trigger the vomiting process
Inflammation as a cause of
PONV
Causes of intraabdominal
organ inflammation are
multifactoral and may
include irritation, infection,
toxin exposures, and surgical
procedures and anesthesia
Mattson-Porth, 2005
http://digestive.niddk.nih.gov
Anesthesia, surgery and PONV
Gastric inflation during mask ventilation may cause
PONV by producing gaseous distention of stomach/
upper small intestine
Nitrous oxide gas diffusion into spaces of intestinal wall
worsens distention
Surgical procedures may produce gastric inflammationi.e. gastric resection.
Inflammation activates mechanoreceptors which send
afferent signals to vomiting center via vagus nerve
Rahman et al, 2004
The corticotropin-releasing
factor system
Integrator of CNS response to
stress/negative emotion
Hypothalamus controls release
of CRH
When released during stress,
increases transit through large
bowel/delays gastric emptying
which may produce PONV
Larzelere, 2008
Activities of brain and gut are highly interrelated,
which accounts for high prevalence of GI symptoms
reported by patients in response to stress
Stress may be psychological
Psychological stress may be manifested prior to surgery
in nervous patient who is already experiencing a queasy
stomach
GI difficulty can impact mood, behavior, and pain
responsiveness
Larzelere, 2008
Stress may be physical
Surgical trauma stimulates the release of CRH
Increased cytokine production, as a result of stress, can
produce similar physiologic effects (delayed gastric
emptying/increased colonic motility)
Minimally invasive surgery reduces wound size and
thereby decreases the undesirable inflammatory
response, pain and catabolism
Larzelere, 2008
Answer True or False to the following questions
Click on the correct answer
1.
True or False-Mask ventilation may cause PONV by
creating gastric and upper intestinal inflammation
2.
True or False- The medulla controls the release of CRH,
which, when released during stress increases transit
through the bowel and delays gastric emptying.
3.
True or False-Minimally invasive surgery reduces wound
size and decreases the undesirable inflammatory
response
There are genetic differences in how drugs are metabolized
Genetic information is stored in the structure of DNA
Errors in duplication of DNA may occur producing a
mutation
Somatic mutation affects a group of cells that differentiate
into one or more of many tissues of body
Somatic mutations that do not have an impact on health
or functioning are called polymorphisms
Mattson-Porth, 2005
Majority of drugs are metabolized via microsomal enzymes
localized in liver, and to a lesser extent, small intestine
Activity of many drugs depends on their interaction with
enzymes of P450 (CYP) system
More than 5o human CYP isozymes have been identified,
CYP2D6 is best characterized isozyme
CYP2D6 metabolizes approximately 25% of all clinically used
medication, including antiemetics
Genetic polymorphisms in drug-metabolizing enzymes are a
major cause of variability in drug metabolism leading to adverse
effects or lack of therapeutic effect
Bernard, 2006
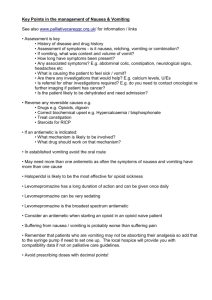
Primary purpose of risk factor identification in
preoperative period is to determine potential risk of a
patient developing PONV or PDNV
Risk factor tools have been developed to identify
patients at high risk for PONV
The simplified tools provide better discrimination and
calibration for prediction of PONV
ASPAN’S Evidence-Based Clinical
Practice Guideline-PONV/PDNV2006
1-2 risk factors=20-40% risk of developing PONV
3-4 risk factors increase number of patients with PONV to
60-80%
Patients with 20% or greater risk of developing PONV
should be considered high risk and treated prophylactically
Appropriate PONV prophylaxis should reduce need for
postoperative treatment and reduce length of stay in PACU
Kapoor, 2008
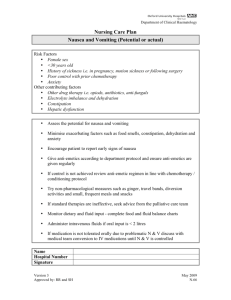
The following risk factors are supported by strong evidence
in literature
Female-two-four fold higher incidence of PONV compared to
males
History PONV and motion sickness-doubles risk
Nonsmoker-doubles risk
Postoperative opioids-doubles risk
Volatile Anesthetics
Nitrous Oxide
ASPAN’S Evidence-Based
Clinical Practice
Guideline-PONV/PDNV2006
A risk factor that is supported by conflicting evidence
in the literature is the type of surgery
Risk factors increase with abdominal, gynecologic,
orthopedic, ENT surgery
Laparoscopic surgery increases risk because of gas
insufflated into abdomen or pelvis
Intubation increases risk due to pharyngeal
mechanoreceptor afferent stimulation
Wender, 2009
PONV is a significant concern because
It exacerbates patient discomfort
Increases risk for suture dehiscence, esophageal rupture,
aspiration and subcutaneous emphysema
Prolonged postoperative hospital stays
Delayed return of patient functional ability
Need for additional drug treatment and nursing care
increases cost of care
Kapoor, 2008
Answer True or False to the following questions
Click on the correct answer
1.
True or False-Genetic polymorphisms may exist in the
enzymes that metabolize medications leading to adverse
effects (such as PONV) or lack of drug effectiveness
2.
True or False-The primary purpose of risk factor
identification preop is to determine the risk for PONV
3.
True or False-PONV increases patient discomfort,
prolongs stay and delays return to patient functional
ability
You are correct,
polymorphisms are
interesting, don’t you
agree?
Click to go back
8 classifications of medication to treat PONV
Classification
Generic
Brand
Phenothiazine
Procholoroperazine
Compazine
Anticholinergic
Scopolamine
Isopto Hyoscine
Antihistamine
Promethazine
Phenergan
Butyrophenones
Droperidol
Inapsine
Benzamides
Metoclopromide
Reglan
Corticosteroids
Dexamethasone
Decadron
5-HT3 receptor
antagonists
Ondansetron
Zofran
NK1 receptor
antagonists
Aprepitant
Rahman, 2004
Emend
Target neurotransmitter-receptor sites in brain and
peripherally
Anti-emetic may target single or multiple receptors
Each pathway functions independently providing an
opportunity to treat PONV
When therapies from multiple drug classes are
combined, targeting multiple receptor systems,
increase in antiemetic efficacy is generally observed.
Ignoffo, 2009
Phenothiazines
Mainly block
dopamine/5HT3 receptors
in CTZ
Act against agents that
directly stimulate CTZ
(opioids/general
anesthesia)
Active against emetic
stimuli from GI tract
Copyright 2004, Amdipharm plc. All rights
reserved
Rahman, 2004
Anticholinergics
Block action of
acetylcholine at
muscarinic receptors in
vestibular system
Reduces gastric
motility/afferent
stimulation of vomiting
center
Copyright 2004, Amdipharm plc. All rights
reserved
Antihistamines
Block acetylcholine
action in vestibular
apparatus
Less effect on vomiting
induced by direct
stimulation CTZ
Rahman, 2004
Copyright 2004, Amdipharm plc. All
rights reserved
Butyrophenones
Block dopamine
receptors in CTZ
Similar properties to
phenothiazines
*Droperidol-monitored
patients only(potential
prolong cardiac QT
interval)
Rahman, 2004
Copyright 2004, Amdipharm plc. All
rights reserved
Benzamides
Block dopamine
receptors in CTZ
Block peripheral
dopamine receptorsenhanced
gastric/upper intestinal
motility
Rahman, 2004
Copyright 2004, Amdipharm plc. All rights
reserved
Corticosteroids
Precise mechanism of
action unknown
Effects thought to be
mediated by
antiinflammatory/
membrane stabilizing
activities peripherally and
centrally
Kloth, 2009
Copyright 2004, Amdipharm plc. All rights
reserved
5HT3 receptor
antagonists
Block 5HT3 receptors
Peripherally in gut
(vagal afferent nerves)
Centrally in CTZ
Rahman, 2004
Copyright 2004, Amdipharm plc. All
rights reserved
Neurokinin-1 receptor
antagonists
Block substance P
(neurotransmitter)
at neurokinin-1
receptors
Vomiting center and
CTZ
Rahman, 2004
Copyright 2004, Amdipharm plc. All rights reserved
Answer True or False to the following questions
Click on the correct answer
1.
True or False-There are four classifications of medication
to treat PONV
2.
True or False-Medications target receptors peripherally
and centrally and some target more than one site
3.
True or False-PONV is decreased by combining
medications that target multiple receptors
Fluid abnormalities may be multifactoral
Preoperative fasting
Surgical preps (bowel preps)
Administration/management anesthesia
Surgical procedure/associated fluid losses
Noble, 2008
IV fluid therapy
Perioperative fluid administration of greater than 1L
improves recovery after minor to moderate operations
Data does not support choice of one fluid over another
IV fluid generally reduced postoperative
drowsiness/dizziness
Be cautious-vulnerable patients-fluid volume overload!
Holte, 2006
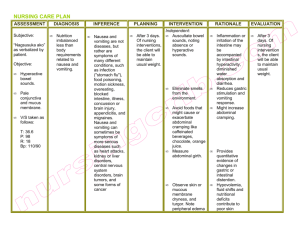
Nursing diagnosis-Nausea
Outcome- Improve or maintain hydration
Intervention-Manage fluid/electrolyte balance
Nursing activities
Promote oral intake in absence N/V
Set appropriate IV rate, (consider current IV fluid intake,
patient comorbidities)
Keep accurate record I/O
Monitor S/S fluid retention (monitor lab values)
Monitor vital signs
Assess buccal membranes, sclera, skin indications altered
fluid/electrolyte balance
Bulechek, 2008
Moorhead, 2008
Nursing diagnosis-Nausea
Outcome-control of nausea and vomiting
Intervention-nausea and vomiting management
Nursing activities
Identify risk factors N/V pre and postoperatively
Evaluate past experiences with nausea
Complete assessment N/V –frequency, duration, severity,
precipitating factors (use tool, i.e. Rhodes Index of N/V)
Bulechek, 2008
Moorhead, 2008
Nursing Activities (interrelate with pathophysiology)
Cerebral cortex
Control environmental factors –aversive smells, sounds,
unpleasant visual stimulation
Reduce/eliminate personal factors that precipitate or
increase nausea/vomiting (anxiety, fear, fatigue, lack of
knowledge)
Oral hygiene to promote comfort with nausea/following
emesis
Clean up after emesis with special attention to removing
odors
Teach use of nonpharmacologic techniques (guided imagery)
Bulechek, 2008
Nursing Activities
GI tract
Position to prevent aspiration/maintain airway
Provide physical support during vomiting (assist person to
bend over or support person’s head)
Wait at least 30 minutes after emesis, start with fluids that
are clear/free of carbonation-gradually increase fluids if no
vomiting in 30 minute period
Monitor for damage esophagus/posterior pharynx from
prolonged retching/vomiting
Ensure effective antiemetics given to prevent N/V- monitor
effects vomiting management throughout
Bulechek, 2008
Nursing Diagnosis-Surgery recovery delayed
Outcome-decreasing the severity of nausea and
vomiting
Interventions-managing nausea and vomiting
Nursing activities
All activities as listed for nausea and vomiting
management (please review content as needed)
Bulechek, 2008
Moorhead, 2008
American Society of Perianesthesia Nurses developed
clinical practice guidelines in 2006
16 multispecialty, multidisciplinary experts
reviewed/analyzed published data and developed a
consensus for clinical practice recommendations
Algorithms developed for prevention and/or
management of PONV/PDNV
ASPAN’S Evidence-Based
Clinical Practice
Guideline-PONV/PDNV2006
ASPAN’s Evidence-based Clinical Practice Guideline for the
Prevention and/or Management of PONV/PDNVr((2006)
Journal of PeriAnesthesia Nursing, 21(4), pp 230-250
*ASPAN=American Society of Perianesthesia Nurses
Answer True or False to the following questions
Click on the correct answer
1.
True or False-Perioperative fluid administration of
greater than 1 L improves recovery after minor to
moderate operations
2.
True or False-Reducing or eliminating personal factors
(fear/anxiety) that may increase N/V targets the cerebral
cortex
3.
True or False-After an emesis it is important to wait 30
minutes before offering liquids that are clear and free of
carbonation
Music therapy-Application of music to influence
physical, mental, emotional functioning. Often used
with behavioral techniques
Relaxation-Progressive muscle relaxation to establish a
deep state of relaxation. Focused breathing often used
with this technique
Guided imagery-Form a relaxing and pleasing mental
image, often proceeded by relaxation, used with music
Quinn, 2004
Distraction-Focus attention on activity unrelated to N/V
Aromatherapy-Use of essential oils combined in a carrier
cream. Used with massage
Acupressure-Application of digital pressure or
acustimulation bands in a specific way on designated
points on body.
Used to correct imbalances by stimulating/easing energy flow
P6-most common/easily accessible-three finger-widths from
wrist crease
ASPAN’S Evidence-Based Clinical Practice
Guideline-PONV/PDNV-2006
Nunley, 2008
Novel drugs created which target existing receptors,
but have sufficiently different pharmacological
properties and different clinical behaviors
Standardization of care for managing PONV/PDNV
More research related to PDNV-Introduction of new
prophylactic modalities that outlast range of
traditional antiemetics
Wender, 2009
Melissa is a 34 year old female that came to the ER with abdominal
pain/fever/N/V
CT scan-indicated acute appendicitis
Transferred to day surgery-prepped for laparoscopic appendectomy.
To be seen by anesthesiologist prior to surgery
Pt dataSurgery in past without N/V
History of motion sickness
Denies history of heart disease, kidney disease, diabetes or lung
disease
Click on arrow below question when you are ready
for answer
1. What are Melissa’s identified risk factors for PONV?
Female and positive history motion sickness
2. Is it appropriate to premedicate Melissa to prevent
PONV?
Yes. Dr Green gives the nurse an order to
apply a scopalamine patch and give Pepcid 20mg IVP
Melissa arrives in PACU following surgery.
It was discovered that her appendix was ruptured, will need to be
admitted for IV antibiotics.
In surgery, received IV propofol for anesthesia, fentanyl for pain and
zofran. EBL minimal, IV intake 500cc
Awakens complaining of pain in her abdomen level 8/10(0 being no
pain, 10 worst pain imaginable)
PACU nurse gives her 10mg morphine-pain to level 4/10
and infuses additional 200cc IV fluid
PACU nurse calls report to floor-vital signs stable, dressings intact,
patient is sleepy, awakens easy, denies nausea
Click on arrow below question when you are ready for
answer
1. Would it be appropriate in PACU to provide an
additional antiemetic?
Yes, opioids are a risk for PONV,
patient received 10 mg morphine in PACU
2.
Could Melissa have received more IV fluids?
Yes, she could have received 1 L of
fluid perioperatively for a moderate
operation in a healthy person
Melissa is transported to her
fourth floor room
Upon arrival, she is asked to
slide from the cart onto the
bed
Once in bed, she complains
of nausea and states “I’m
going to throw –up” She is
handed a basin and has a
100cc emesis
Click on arrow below question when you are ready for
answer
1. What would be your first steps in treating Melissa’s
PONV?
Determine what antiemetics she has already
received (scopalamine and pepcid preop, zofran in OR)
Based on physiology/pharmacology choose a
medication that acts at a different receptor site from
those already given
Infuse IV fluids, and hang second bag
Click on arrow below question when you are ready for
answer
1. Melissa is feeling better now, her nausea and vomiting
have not recurred. How are fluids started and can
additional antiemetics be given if needed?
Wait 30 minutes after last emesis and then
begin with sips of clear liquids that are free of
carbonation
If nausea and vomiting recur, additional
antiemetics may be given targeting a different
receptor site
Congratulations, you have
completed the tutorial, give
yourself a round of applause!!
ASPAN. (2006). Evidence-Based Clinical Practice Guideline for the Prevention and/or
Management of PONV/PDNV. Journal of PeriAnethesia Nurses , 21 (4), pgs 230250.
Bernard, S. N. (2006). Interethnic Differences in Genetic Polymorphism of CYP2D6 in
the US Population: Clinical Implications. The Oncologist , 11: pgs 126-135.
Bulechek, G. B. (2008). Nursing Interventions Classification (NIC). St Louis: Mosby
Elsevier.
Candiotti, K. B. (2005). The Impact of Pharmacogenics on Postoperative Nausea and
Vomiting. Anesthesiology , 102 (3), pgs 543-549.
DiPiro, J. T. (2005). Pharmacotherapy: A Pathophysiologic Approach. New York:
McGraw-Hill.
Holte, K. (2006). Fluid Therapy and Surgical Outcomes in Elective Surgery: A Need for
Reassessment in Fast-Track Surgery. Journal American College of Surgeons ,
202 (6), pgs 971-989.
Ide, P. F. (2008). Perioperative Nursing Care of the Bariatric Surgical Patient. American
Operating Room Nurse , 88 (1) pgs 30-58.
Ignoffo, R. (2008). Current research on PONV/PDNV: Practical implications for today's
pharmacist. American Journal Health-System Pharmacy , 66(1) S19-24.
Johnson, M. B.-D. (2006). NANDA, NOC, and NIC Linkages. St Louis: Mosby Elsevier
Kapoor, R. H. (2008). Comparison of two instruments for assessing risk of postoperative
nausea and vomiting. American Journal Health-System Pharmacy , 65: 448-453.
Kloth, D. (2009). New pharmacologic findings in the treatment of PONV and PDNV.
American Journal Health-System Pharmacy , 65 (1) S11-18.
Larzelere, M. J. (2008, july 11). Stress and Health. Retrieved February 23, 2009, from The
Clinics: Primary Care: http://primarycare.the clinics.com
Mattson-Porth, C. (2005). Pathophysiology: Concepts of Altered Health States.
Philadelphia: Lippincott Williams & Wilkins.
Microsoft Clip Art Images. Retrieved March 15, 2009 from http://office.microsoft.com/
en-us/tou.aspx
Moorhead, S. J. (2008). Nursing Outcomes Classification (NOC). St Louis: Mosby
Elsevier.
Nausea and Vomiting-an introduction (2004). Retrieved March 15, 2009 from
http://www.nauseaandvomiting.co.uk
Noble, K. (2008). Fluid and Electrolyte Imbalance: A Bridge Over Troubled Water.
Journal of PeriAnesthesia Nursing , 23 (4), pgs 267-272.
Noble, K. (2008). The Obesity Epidemic: The Impact of Obesity on the PeriAnesthesia
Patient. Journal of PeriAnesthesia Nursing , 23 (6), pgs 418-425.
Nunley, C. W. (2008). The Effects of Stimulation of Acupressure Point P6 on
Postoperative Nausea and Vomiting: A Review of Literature . Journal of
PeriAnesthesia Nursing , 23 (4), pgs 247-261.
.
Pavlin, J. (2008). Recovery after ambulatory anesthesia. Current opinion in
Anaesthesiology, 21(6), pgs 729-735.
Quinn, D. (2004). PeriAnesthesia Nursing Core Curriculum: Preoperative, Phase I
and Phase II PACU Nursing . St Louis: Elsevier.
Rahman, M. (2004). Post-operative nausea and vomiting. The pharmaceutical
Journal, 273, pgs 786-788.
Stevenson, C. (2006, July 19). Drugs for preventing postoperative nausea and vomiting
(Review). Retrieved February 23, 2009, from Cochrane Database of Systemic
Reviews: http://www.the cochranelibrary.com
Villars, P. V.-M. (2008). Adaptation of the OODA Loop to Reduce Postoperative
Nausea and Vomiting in a High-Risk Outpatient Oncology Population.
Journal of PeriAnesthesia Nursing , 23 (2) pgs 78-86.
Wender, R. (2009). Do current antiemetic practices result in positive patient
outcomes? Results of a new study. American Journal Health System
Pharmacy , 6 (1) S3-10.
Wilhelm, S. D.-S.-P. (2007, march 21). Prevention of Postoperative Nausea and
Vomiting. Retrieved march 4, 2009, from Medscape:
http://www.medscape.com


![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)