Imaging modalities
advertisement

Imaging modalities
History
Energy Source
The earliest medical images used light to create photographs,
either of gross anatomic structures, or if a microscope was used,
of histological specimens. Light is still an important source for
creation of images. However, visible light does not allow us to
see inside the body.
X-rays were first discovered in 1895 by Wilhelm Conrad
Roentgen, who was awarded the 1901 Nobel prize in physics for
this achievement. The discovery caused worldwide excitement,
especially in the field of medicine; by 1900, there already were
several medical radiological societies. Thus, the foundation was
laid for a new branch of medicine devoted to imaging the
structure and function of the body
X-Ray system
Principle of an X-ray system with image intensifier. X rays impinging on the
image intensifier are transformed into a distribution of electrons, which
produces an amplified light image on a smaller fluorescent screen after
acceleration. The image is observed by
a television camera and a film camera and can be viewed on a computer
screen and
X-Ray tube
Cathode
Filament
Rotor
Anode
Vacuum envelope
The X-rays are produced from electrons that have been accelerated from in vac
from the cathode to the anode.
Emission occurs when filament is heated by passing current through it.
When the filament is hot enough, the electrons obtain thermal energy sufficient to
overcome the energy binding the electron to the metal of the filament.
After accelerated they will be stopped at a short distance. Most of the electron en
will produce heat at the anode. Some percentage will be converted to X-ray by tw
main methods.
Deceleration of charged particle results in the emission of electromagnetic field
called Bremmstralung radiation.
These rays will have wide, continuous distribution of energies with the maximum
being the total energy the electron had when reaching the anode.
The number of X-rays will be small at higher energies and increased for lower en
Contrast enhancement
Principle of contrast enhancement:
(a) intensity distribution along a line of an image;
(b) same distribution after injection of the contrast medium;
(c) intensity distribution
after subtraction;
(d) intensity distribution after contrast enhancement.
Example of digital subtraction angiography
(DSA) of the bifurcation of the aorta
An initial image mask is obtained digitized and stored
Contrast medium is injected
Number of images are obtained.
Mask is subtracted
The resulting image contains only the relevant information
The differences can be amplified so the eye will be able to perceive the the blood
vessels.
Quality of deteriorate due to movements of the body can be corrected to some ex
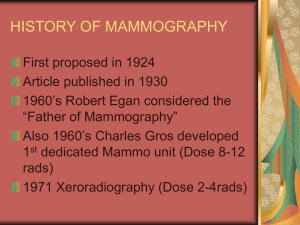
Mammography;
The mammogram is an X-ray shadowgram from a quasi-point source irradiate the breast
and the transmitted X-rays are recorded by an image receptor. A region of reduced
transmission corresponding to a structure of interest such as a tumor, a calcification or
normal fibroglandular tissue. The imaging system must have a sufficient spatial
resolution to delineate the edges of fine structures in the breast. Structural detail small
as 50 m must be resolved adequately. Because the breast is sensitive to ionization
radiation, which at least at high doses is known to cause breast cancer, it is desirable to
use the lowest radiation dose compatible with excellent image quality.
’
Grid
T
Scatter
t
Breast Lesion
Image
receptor
Simplified computer model of the mammographic image acquisition process:
For the simplified case of monoenergetic x-rays of energy E, the number of x-rays
recorded in a fixed area of the image is proportional to:
N B N 0 ( E )e
In the “background”
and:
N L N0 ( E )e
T
[ (T t ) ,t ]
The difference in x-ray transmission gives rise to subject contrast which can be
defined as:
NB NL
C0
NB NL
For monoenergetic x-rays and temporarily ignoring scattered radiation
C0
1 e
( , )t
1 e
( , ) t
For a given image recording system (image receptor) a proper exposure requires a
specific value of x-ray energy transmitted by the breast and incident on the receptor,
i.e. a specific value of NB. The breast entrance skin exposure required to produce an
image is therefore proportional to:
N 0 N B ( E )e
t
What Can Diagnostic Mammography
Show?
Diagnostic mammography may show that an abnormality (lesion) has
a high likelihood of being benign (not cancer). For these, it is
common to ask the woman to return earlier than usual for a recheck,
usually in 6 months. A diagnostic mammogram may show that the
abnormality is not worrisome at all and the woman can then return to
routine yearly screening mammography. In some cases, patients with a
cyst (fluid filled pocket) or other abnormality will also receive
ultrasound imaging to obtain further diagnostic information. Finally,
the diagnostic work-up may suggest that biopsy (tissue sampling) is
needed to tell whether or not the abnormality is cancerous. A
recommendation for biopsy does not necessarily mean that the
abnormality is cancer. About 65% of all breast lesions that are
evaluated with biopsy are found to be benign (non-cancerous) when
evaluated under the microscope.
What Abnormalities Does Mammography Detect and Diagnose?
Mammography is used to detect a number of abnormalities, the two
main ones being calcifications and masses. Calcifications are tiny
mineral deposits within the breast tissue that appear as small white
spots on the films. Calcifications are divided into two categories,
macrocalcifications and microcalcifications. A mass is any group of
cells clustered together more densely than the surrounding tissue. A
cyst or fluid collection may also appear as a mass on mammography.
The difference between a solid mass and a cyst can often be shown
with ultrasound.
Calcifications:
Macrocalcifications are coarse (larger) calcium deposits that are often associated with
fibrocystic change or with degenerative changes in the breasts, such as aging of the bre
arteries, old injuries, or inflammation. Macrocalcification deposits are associated with
benign (noncancerous) conditions and do not require a biopsy. Macrocalcifications are
in about 50 % of women over the age of 50.
Microcalcifications are tiny (less than 1/50 of an inch) specks of calcium in the breast.
When many microcalcifications are seen in one area, they are referred to as a cluster an
indicate a small cancer. About half of the cancers detected by mammography appear as
of microcalcifications.
Microcalcifications are the most common mammographic sign of ductal carcinoma in s
(meaning the cancer has not spread or invade neighboring tissue). Almost 90% of cases
of ductal carcinoma in situ are associated with microcalcifications.
An area of microcalcifications seen on a mammogram does not always mean that
is present. The shape and arrangement of microcalcifications help the radiologist
the likelihood of cancer being present. In some cases, the microcalcifications do not
indicate a need for a biopsy. Instead, a doctor may advise a follow-up mammogram withi
months. In other cases, the microcalcifications are more suspicious and a stereotactic bi
is recommended. Only 17% of calcifications requiring biopsy are cancerous.
Masses: Another important change seen on a mammogram is the presence of a mass, wh
may occur with or without associated calcifications. A mass is any group of cells clustered
together more densely than the surrounding tissue. Masses can be due to many things, in
cysts, which are non-cancerous collections of fluid in the breast. A cyst cannot be diagnos
by physical exam alone nor can it be diagnosed by mammography alone, although certain
can suggest the presence of a cyst or cysts. To confirm that a mass is a cyst, either breast
ultrasound or aspiration with a needle is required. If a mass is not a cyst, then further imag
may be obtained. As with calcifications, a mass can be caused by benign breast condition
By breast cancer. Some masses can be monitored with periodic mammography while othe
may require biopsy. The size, shape, and margins (edges) of the mass help the radiolo
in evaluating the likelihood of cancer. Breast ultrasound is often helpful. Prior mammog
may help show that a mass is unchanged for many years, indicating a benign condition an
helping to avoid unnecessary biopsy. Having prior mammograms available to the radiologi
as discussed above, is very important.
Mammography alone cannot prove that an abnormal area is cancer although some
abnormalities are very characteristic of malignancy.
If mammography raises a significant suspicion of cancer, tissue must be removed for
examination under the microscope to tell if it is cancer.
This can be done with one of several breast biopsy techniques.
Ductography, also know as a Galactogram, is special type of contrast enhanced mammog
used for imaging the breast ducts. Ductography can aid in diagnosing the cause of an abn
nippledischarge and is valuable in diagnosing intraductal papillomas.
Digital Mammography
One of the most recent advances in x-ray mammography is digital mammography. Digital
(computerized) mammography is similar to standard mammography in that x-rays are use
produce detailed images of the breast. Digital mammography uses essentially the same
mammography system as conventional mammography, but the system is equipped with a
receptor and a computer instead of a film cassette. Several studies have demonstrated th
Mammography is at least as accurate as standard mammography.
Digital spot view mammography allows faster and more accurate stereotactic biopsy. This
in shorter examination times and significantly improved patient comfort and convenience s
the time the patient must remain still is much shorter. With digital spot-view mammography
images are acquired digitally and displayed immediately on the system monitor. Spot-view
systems have been approved by the U.S. Food and Drug Administration (FDA) for use in g
breast biopsy. Traditional stereotactic biopsy requires a mammogram film be exposed, dev
and then reviewed, greatly increasing the time before the breast biopsy can be completed
In addition to spot-view digital mammography, the FDA has recently approved a "full-field"
digital mammography system to screen for and diagnose breast cancer. Currently, only ha
copy printouts of the digital mammographic images maybe used by radiologists. With cont
improvements, the "full-field" mammography systems may eventually replace traditional
mammography.
How Does Digital Mammography Differ From Standard Mammography?
In standard mammography, images are recorded on film using an x-ray cassette. The film
viewed by the radiologist using a "light box" and then stored in a jacket in the facility’s arch
With digital mammography, the breast image is captured using a special electronic
x-ray detector, which converts the image into a digital picture for review on a computer mo
The digital mammogram is then stored on a computer. With digital mammography, the
magnification, orientation, brightness, and contrast of the image may be altered after the e
completed to help the radiologist more clearly see certain areas.
Digital mammography provides many benefits over standard mammography equipment.
These benefits include:
•
faster image acquisition
•
shorter exam time
•
easier image storage
•
physician manipulation of breast images for more accurate
detection of breast cancer
•
transmittal of images over phone lines or a computer network for remote consultati
other physicians
Digital mammography has the potential to significantly reduce the amount of time required
acquire a mammogram from 10 to 15 minutes to less than a minute. This will provide a sh
more comfortable exam for the woman and possibly allow mammography facilities to cond
more mammograms in a day. Digital images can also be manipulated to correct for under
over exposure. If under or over exposure occurs with a standard film-based mammograph
System women have to undergo a repeat mammogram before leaving the facility.
Many radiologists support digital mammography as an effective tool to
screen for breast cancer.
The contrast resolution of these devices is inherently better, "In addition, the extra features
digital mammography will ultimately provide, such as telemammography, tomosynthesis, a
computer-aided diagnosis will prove invaluable to patients and their doctors,”
Telemammography (also called teleradiology) allows radiologists to share digital images vi
phone or network connection for remote consultation with other physicians;
tomosynthesis allows radiologists to add or subtract digital mammography images using a
computer workstation for enhanced diagnostic capability. Computer-aided detection (CAD)
was approved by the FDA in June 1999. CAD helps radiologists more accurately
detect breast cancer by marking suspicious areas on digitized mammograms.
Promising Developments in Digital Mammography
The FDA has approved the first "full-field" digital mammography scanner to screen for and
diagnose breast cancer in February 2000. Before applying for FDA certification, data was
gathered from 662 patients at four institutions: the University of Colorado, the University
of Massachusetts Medical Center, Massachusetts General Hospital, and the Hospital of the
University of Pennsylvania. The data compared hard copies of digital breast images on film
conventional mammography films finding that digital mammography is as effective at detec
breast cancer as standard film mammograms. A separate study revealed that the digital
mammography scanner showed a slight advantage in the visibility of breast tissue at the sk
Disadvantages to Digital Mammography
While digital mammography is quite promising, it still has additional hurdles to undergo b
it replaces conventional mammography. Digital mammography must:
provide higher detail resolution (as standard mammography does)
become less expensive (currently several times more costly than
conventional mammography)
provide a method to efficiently compare digital mammogram
images with existing mammography films on computer monitors
Standard mammography using film cassettes has the benefit of providing very high deta
resolution (image sharpness), which is especially useful for imaging microcalcifications
(tiny calcium deposits) and very small abnormalities that may indicate early breast
cancer. While full-field digital mammography may lack the spatial resolution of film, clinic
trials have shown digital mammography to be at least equivalent to standard film screeni
mammography. This is because digital mammography has the benefit of providing impro
contrast resolution, which may make abnormalities easier to see. Various manufacturers
trying to develop digital mammography systems with detail resolution equivalent to
standard film mammography while also providing the benefits of digital mammography n
above.
The high cost of digital mammography is a major obstacle. Digital mammography system
costs roughly four to five times as much as standard mammography equipment. Standar
mammography systemsare currently installed in over 10,000 locations across the United
It may take years for this current equipment to be updated or replaced
and for digital mammography to become widespread after its approval
by the FDA.
Benign lesion - Fibroadenoma
Computerized Tomography
Imaging of a cross sectional slice of the body using X-rays.
Invented by Dr. G. N. Housfield in 1971. Received the Nobel prize in
medicine in 1979.
The method is constructing images from large number of measurements
of x-ray transmission through the patient. The resulting images are
tomographic maps of the X-ray linear attenuation coefficient.
First generation CT
Single X-ray source
Translate – rotate
movement
Single detector
4th generation CT Fan beam, stationary detectors.
Moving X-ray source
source
Stationary Detectors
(600-4800)
Fifth generation CT
(Image data are acquired in as little as 50 mSEC).
DAS
Detector ring
Gun
Patient table
Electron
beam
Target rings
CT (by Picker)
Colonoscopy with spiral CT
Spiral scan
Example of cross-sections through several parts of the body:
skull, thorax, and abdomen,
obtained by computed tomography.
Visualization of the values of the attenuation coefficients by way
of gray values produces an anatomic image.
The principle of CT
The intensity of the transmitted beam as a function of the attenuation
coefficient of the pixels traversed. Upper part, the intensity after crossing
one volume element; middle part, after traversing n volume elements;
lower part, the analog case.
Upper left, density distribution of a point absorber along a line through the objec
lower left, the resulting intensity profiles;
lower right, the back- projection;
upper right, reconstructed density distribution on a line through the object.
Back projection method
Starts with the assumption that the absorbing medium is uniformly distributed.
with several intensity profile we get a star-like reconstructed image.
By increasing the number of angles, the intensity in the center decreases and we
back projected image but less sharp.
Instead of showing one attenuation pixel,
The neighboring pixels are visible in the reconstructed image as well.
This blurring is corrected with filtering techniques.
Some Mathematics:
y
t
s
(x,y)
x
P(t,) - Projection data into each detector (Radon transform)
p( t , ) c
z
f ( x , y ) ds
The relationship between the source position (x,y) the projection angle and
position of the detection on the 1D detector array is given by:
t y cos x sin
In 2D tomographic imaging, The 1D detector rotates around the object.
The goal of image reconstruction is to solve the inverse Radon
transform.
The solution is the reconstructed image estimate of the object distribution f(x,y)
The measured projection data is given by:
p , ( t , ) ct I 0 exp[
z
( x , y )ds]
I0 - intensity of the incident x-ray.
(x,y) - 2D attenuation coefficient
ct - gain factor which transforms x-ray intensity
to detected signals.
We’ll write again the reconstruction problem:
I
p( t , ) ln[ , 0
]
p (t , )
z
( x , y )ds
With the goal to solve the for the attenuation coefficient.
Image reconstruction algorithms from
projections
Simple backprojection:
m
f ( x , y ) p( y cos j x sin j , j )
j 1
Where:
j - the jth projection angle.
m - number of projection views.
- The angular spacing between adjacent projections.
This backprojected image is a poor approximation of the
true object. It is equivalent to the true objection object, blurred
by a blurring function in the form 1/r.
Filtered backprojection
• Filter the measured projection data at different projection
angles with a special function.
• Backproject the filtered projection data to form the
reconstructed image.
Filtering can be implemented in 2 ways, in the spatial domain, the filter operation
equivalent to to convolving the measured projection data using a special convolv
function h(t)
p , ( t , ) p( t , ) h( t )
More efficient multiplication will be in the spatial frequency domain.
• FFT the measured projection data into the frequency domain:
p(,)=FT {p(t, )
• Multiply the the fourier transform projections with the special function.
•Inverse Fourier transform the product p’(,).
The solution of the inverse Radon transform specifies the form
of the special function.
This function is given below:
h( x )
1 R Lx O
R
U
U
L
O
sin
c
S
V
S
V
M
P
M
P
4
(
x
)
2
x
N
Q
N
Q
T
W T
W
1
x
sin
c
2( x ) 2
x
2
Where X is the linear sampling interval and sinc (z) =sin(z)/z. The function h
consists of a narrow central peak with high magnitude and small negative side
It removes the blurring from the I/r function found in the simple backprojected
images. In the frequency domain H() is given by:
H()= ||rect()
where || is the ramp function and
1 ||0.5
rect ()= {
0 ||>0.5
The rectangular function rect() when the absolute value of is less than the
Nyquist frequency at 0.5 cycles per pixel.
Additional smoothing function may be applied for noisy data.
Attenuation coefficients of several tissues expressed
in Hounsfield units.
Magnetic resonance imaging (MRI)
Joe
N
S
S
N
S
N
N
S
N
S
Magnetic resonance imaging exploits the existence of induced nuclear magnetism in the
patient. Magnets with an odd number of photons or neutrons possess a weak but observable
nuclear magnetic moment. Most commonly photons (H) are imaged, although
(13C, Phosphorous (P) sodium (Na) and Fluorine (F) are also of significant interest.
The nuclear moments are normally randomly oriented, but they align when placed in a strong
magnetic field (typically 0.2-1.5 T).
The NMR signal from a human is due predominantly to water protons. Since these
protons exists in identical magnetic environments, they all resonate at the same frequency.
Hence the NMR signal is simply proportional to the volume of the water. The key innovation
for MRI is to impose spatial variation on the magnetic field to distinguish spins by their
location. Applying a magnetic field gradient causes each region of the volume to oscillate at
a distinct frequency.
The primary contrast mechanisms exploit relaxation of the magnetization are T1 and T2.
Spin-lattice relaxation T1: The exponential rate constant describing the decay of the z
component of magnetization towards the equilibrium magnetization. Typical values in the
body are between 300 and 3000 ms.
Spin-Spin relaxation T2: The exponential rate contrast describing the decay of the transverse
components of magnetization (Mx and My).
MR images provide excellent contrast between various forms of soft tissues. For patients
who have no ferromagnetic foreign bodies within them, MRI scanning appears to be
perfectly safe and can be repeated as often as necessary without danger. The NMR signal is
also not blocked by air like US and there is no need for radioactive tracers as in the case of
nuclear medicine scanning. Typical imaging studies range from 1 to 10 minutes but new fast
imaging techniques acquire images in less than 50 msec.
MRI by Picker
Spinal cord
Brain section
Functional MRI
fMRI is a technique that images intrinsic blood signal change with magnetic
Resonance imagers.
Changes in neuronal activity are accompanied by focal changes in cerebral
blood flow (CBF), blood volume (CBV), blood oxygenation and metabolism. These
physiological changes can be used to produce functional maps of mental operations.
There are two basic techniques used:
1 Saturation or inversion of incoming blood signal to quantify
absolute blood flow.
By focusing on blood flow change and not steady state flow, it is possible to
image brain visual functions associated with quantitative perfusion change.
At this way common baseline artifact can be subtracted.
Measuring changes in blood oxygenation during neuronal activity.
The study of changes in blood flow is done also with injection of contrast agents
(i.e. gadolinium-DTPA).
Two relaxation rates are measured in fMRI T1 and T2* (represents the rate of decay of
MRI signal due to magnetic field in-homogeneities and changes in used to measure
blood oxygenation change.
T2* changes reflect the interplay between changes in cerebral blood flow, volume and
oxygenation. As hemoglobin becomes deoxygenated, it becomes more paramagnetic
than the surrounding tissue and thus creates a magnetically inhomogeneous
A functional map (in color) in the cerebellum during performance of a cognitive pegboard puzzle task, overlaid on a T2*-weighted axial image in gray scale. The dentate
nuclei appear as dark crescent shapes at the middle of the cerebellum due to iron
deposits. fMRI images were acquired by conventional T2*-weighted FLASH techniques
with a spatial resolution of 1.25x1.25x8 mm3 and a temporal resolution of 8 seconds.
Each color represents a 1% increment, starting at 1%. R, right cerebellum; L, left
cerebellum. A left-handed subject used the left hand to perform the task. Bilateral
activation in the dentate nuclei and cerebellar cortex was observed. The activated area
in the dentate nuclei during performance of pegboard puzzle was 3-4 times greater than
that seen during the visually guided peg movements. (see details in Kim et al., 1994b).
Whole brain functional imaging study during a visuo-motor error detection and correction task.
Functional images were acquired by the multi-slice single-shot EPI imaging technique with
spatial resolution of 3.1x3.1x5 and temporal resolution of 3.5 seconds. The skull and associated
muscles were eliminated by image segmentation. The 3-D image constructed from multi-slice
images was rendered by Voxel View program (Vital Images, Fairfield, Iowa).The task was to
move a cursor from the central start box onto a square target by moving a joystick. Eight targets
were arranged circumferentially at 450 angles and displaced radially at 200 around a central start
box. Activation (in color) is observed at various brain areas. Top image displays the brain as a
3-D solid object so that only the cortical surface is seen. In the bottom image, a posterior section
was removed at the level of the associative visual cortex to display activation not visible from the
surface (Kindly provided by Jutta Ellermann, Jeol Seagal, and Timothy Ebner).
Open MRI units
Nuclear Imaging
Use of G rays, Radionuclides and
Radiopharmaceuticals in medical
imaging.
Nuclear imaging looks at physiological processes rather than at
anatomical structures. In nuclear imaging, short-lived
radiopharmaceuticals (radioactive drugs that emit gamma rays and
that are attracted to the organ of interest) are injected into a patient's
bloodstream (in amounts of picomolar concentrations thus not having
any effect on the process being studied). The half life of these
materials is between few minutes to weeks. The time course of the
process being studied and the radiation dose to the target are
considered. The nuclear camera then, in effect, takes a time-exposure
"photograph" of the pharmaceutical as it enters and concentrates in
these tissues or organs. By tracing this blood flow activity, the
resulting nuclear medicine image tells physicians about the biological
activity of the organ or the vascular system that nourishes it. Nuclear
Medicine has a wide variety of uses, including the diagnosis of cancer,
studying heart disease, circulatory problems, detecting kidney
malfunction, and other abnormalities in veins, tissues and organs.
Nuclear camera
Whole body nuclear image
SPECT
(single photon emission computerized tomography
SPECT is based on the conventional nuclear imaging technique and tomographic
reconstruction methods.
a
b
d
c
Collimator
Electronics
NaI(Ti)
crystal
PMT
Y
X
Counts/pixel
The most important tool in nuclear medicine is the scintillation camera (anger
camera) based on a large area (~40 cm in diameter) NaI(Tl) crystal.When a
photon hits and interact with the crystal, the scintillation generated and detected
by the area of PMTs. An electronic circuit evaluates the relative signals from the
PMTs and determines the location of the signal.
Performance characteristics of Nuclear
Imaging Systems
Spatial resolution - A measure for the degree of detail the final
reconstructed image provides and hence the size of lesions that m
potentially be detected. In other words: how fine the details are that
be separated.
Sensitivity, dead time - describes how well the radioactive decays
tracer distribution are exploited to form image counts.
A source radiated isotropically into all directions. The camera collec
part that is entering into its solid angle less the photon which will
impinge the collimators.
Some of the events are lost because the system is still processing
previous event (dead time).
Signal to Noise ratio (SNR) - The relative strength of the informatio
and the noise. If the lesion is small compared with the spatial resol
the contrast is reduced because the high lesion activity blurred int
neighborhood by the detector response.
Uniformity, Linearity - The image of an object should be independe
of its position in the field of view. This is not true in real systems.
This can be assessed in calibration measurements to derive correc
factors. This reduces non-uniformity from 10% to 3%.
The conventional nuclear medicine imaging process.
Typical radionuclides used are 140 KeV Tc-99m and 70 KeV photons
from Tl-201.
The gamma ray photons emitted from the radiopharmaceutical
penetrate through the patient body and are detected by a set of
collimated radiation detectors. The emitted photon experience
interaction within the body by the photoelectric effect which stops
their emergence from the body or compton scattering which
transfers part of the energy to free electrons and the photon is
scattered into a new direction. These photons are also detected
by the camera and cause blurring of the image if un-treated with
image reconstruction and processing tools.
In SPECT projection data are acquired from different views
around the patient. Similar to X-ray CT, image processing and
reconstruction methods are used to obtain transaxial or cross
sectional images from multiview projection data.
Camera based SPECT systems can be one of the
configurations below:
SPECT Machine
Discrete geometry used for iterative
reconstruction methods
Pixel I
Activity ai
Intersected area fi
r
P(r,)
In 2-D tomographic imaging, the 1D detector array rotates around
the object distribution f(x,y) and collects projection data from various
projection angles . The integral transform of the object distribution
to its projections is given by:
z
p'(t , ) ct I 0 exp[ ( x, y)ds]
Which is called the Radon transform. The goal of image
reconstruction is to solve the inverse Radon transform. The solution
is the constructed image estimate f(x,y) of the object distribution
f(x,y).
The measured projection data can be written as the integral of
radioactivity along the projection rays.
The measured projection data can be written as the integral of
radioactivity along the projection rays.
z
p(t , ) ce ( x, y)ds
In SPECT attenuation coefficient is not so important, so it can
be considered as constant in the body region under inspection.
z
p(t , ) ce ( x, y) exp[ l ( x, y)]ds
l(x,y) is the pathlength between the point (x,y) and the edge of the
attenuator (or patient’s body) along the direction of the projection
ray.
The image reconstruction problem is further complicated by the non
stationary properties of the collimator detector and scatter response
functions and their dependence on the size and composition of the
patient’s body.
Brain and Liver Tomographic
Reconstruction and 3D Rendering
Positron emission tomography
PET enables physicians to assess chemical or physiological changes
related to metabolism. Since the origins of many diseases are
biochemical in nature, these functional changes often predate or exceed
structural change in tissue or organs. PET imaging utilizes a variety of
radiopharmaceuticals, called "tracers," to obtain images. PET tracers
mimic the natural sugars, water, proteins, and oxygen found in our
bodies. These tracers are injected into a patient and collect in various
tissues and organs. The PET system takes a time-exposure of the tracer
and generates a "photo" of cellular biological activities. PET images
can be used to measure many processes, including sugar metabolism,
blood flow and perfusion, receptor-ligand binding rates, oxygen
utilization and a long list of other vital physiological activities.
PET TRACER PRODUCTION SYSTEMS
PET scanning uses artificial
radioactive tracers and
radionuclides. Their lifetime is
usually rather short, thus they
need to be produced on site.
Some examples of such materials are:
Radionuclide
Carbon-11
Copper –64
Half life
20.3 min
12.8 hours
Iodine –122
Iodine –131
Iron - 52
Nitrogen – 13
3.76 min
8.1 days
8.2 hours
9.9 min
Strontium – 85
Oxygen – 15
Technetium – 99m
64 days
123 sec
6 hours
Application
Positron emitter for metabolism studies
clinical diagnostic agent for cancer and
metabolic disorder
Positron emitter for blood flow study
Diagnose thyroid disorders including cancer
Iron tracer for PET bone marrow imaging
Positron emitter used as 13NH for heart
perfusion studies
Study of bone formation metabolism
Positron emitter used for blood flow
The most widely used radiopharmaceutical
In nuclear medicine
Radiopharmaceutical
EtOOC
N O NH
COOEt
99mTc
S
S
Application: Brain perfusion
PET has a million fold sensitivity advantage over MRI in tracer study
and its chemical specificity, PET is used to study neuroreceptors in
the brain and other body tissues. It is efficient in the nanomolar range
where much of the receptor proteins in the body. Clinical studies
include tumors of the brain, breast, lung, lower GI tract. Additional
study of Alzheimer’s disease, Parkinson’s disease, epilepsy and
coronary artery disease affecting heart muscle metabolism and flow.
Parkinson’s disease study
PET studies has immeasurably added to the understanding of oxygen
utilization and metabolic changes that accompany disease.
Theory
PET imaging starts with the injection of metabolically active tracer – a biologic
molecule that carries with it a positron emitting isotope. Over a few minutes the
isotope accumulates in an area of the body for which the molecule has an affinity.
i.e. glucose labeled with 11C or glucose analogue labeled with 18F, accumulates in the
brain or tumors, where glucose is used as the primary source of energy. The
radioactive nuclei then decay by positron emission. In positron (positive electron) ,
a nuclear proton changes into a positive electron and a neutron. The atom maintains
its atomic mass but decreases its atomic number by 1. The ejected positron combines
with an electron almost instantaneously, and these 2 particles undergo the process of
annihilation. The energy associated with the masses of the positron and electron
particles is 12.022MeV in accordance with E=MC2 . This energy is divided equally
between 2 photons which fly away from one another at 1800 angle. Each photon has
an energy of 511 keV. These high energy gamma rays emerge from the body in
opposite directions and recorded simultaneously by pair of detectors.
The annihilation event that gave rise to them must have occurred somewhere
along the line connecting the detectors. Of course if one of the photons is scattered,
then the line of coincidence will be incorrect. After 100,000 or more annihilation
events are detected, the distribution of the positron-emitting tracer is calculated by
tomographic reconstruction procedures. PET reconstructs a 2 dimensional image
from the one dimensional projections seen at different angles. 3-D reconstructions
can be done using 2D projections from multiple angles.
Tagged
metabolic
activity
Positron annihilation
photons (1800 0.250)
+
N
P
11C
nucleus
Lead
shield
Scintillator
Tungsten
septum
Resolution factors are:
•
•
•
•
•
Detector crystal width
Anger logic
Photon noncolinarity
Positron range
Reconstruction algorithm
Overall data flow during PET acquisition
and processing
Acquisition
Calibration data
Sinogram
Correction data
Counts/ray
Reconstruction
Image
Whole body PET
Study for cardiomyopathy
SA reconstructed slices
Measurements:
• Blood volumes
• Oxygen consumption
• Perfusion
• Glucose consumption
Ultrasound Imaging
Ultrasound operates much the same as sonar, using high-frequency sound waves as its
imaging source. Ultrasound is the reflection of a sound wave as it collides with the
anatomy being studied. The resulting pattern of that reflection is converted into
diagnostic information via a hand-held transducer passed over the area being imaged.
First utilized some 50 years ago, this medical technology's non-radioactive nature has
made it the modality of choice for ob-gyn procedures; in fact, it is most commonly
associated with fetal imaging. Advances in ultrasound technology have resulted in
applications that extend far beyond fetal imaging to include cardiac, vascular and
breast imaging, as well as cyst identification and guidance of a variety of surgical
and other therapeutic procedures.
Ultrasound
examination
Ultrasound
machine
Convex 3.5 MHz
For abdominal and
OB/GYN studies
Micro-convex: 6.5MHz
For transvaginal and
transrectal studies
Ultrasound transducers generate acoustic waves by converting magnetic, thermal, or
electric energy into mechanical energy. The most efficient technique for medical
ultrasound uses the piezoelectric effect. Applying stress on a crystal creates electrical
potential and vise versa. The transducer developed when linear arrays were developed.
To implement real time imaging, rapid steer of the acoustic beam is needed. Linear
sequential arrays were designed to electronically focus the beam in a rectangular image
region. Linear phased area transducers were designed to electronically steer and focus
the beam at high speed in a sector image format.
The standard material fot medical ultrasound for many years is the ferroelectric ceramic
lead-zirconate-titanate (PZT) it has a high electromechanical conversion efficiency and
low intrinsic losses. The properties of the PZT can be adjusted by modifying the ratio of
zirconium to titanium and introducing small amounts of other substances, such as
Tantalum. PZT is mechanically strong and can operate at temperatures up to 1000 C
and it’s stable for a long period of time. The disadvantage is high acoustic impedance
(Z=30 Mrayls) compared with body tissue (1.5 Mrayls). This is compensated with
acoustic matching layers. Other materials are used as well (i.e. PVDF-Polyvinylidene
difluoride).
Array transducers use the same principal as acoustic lenses to focus an acoustic beam.
In both cases variable delays are applied across the transducer aperture.
Focusing and steering is done by delayed excitation signals as follows:
Transmit focus
Excitation signals
The acoustic signal from all elements reach the focal point at the same time. According
to Huygens principle the net acoustic signal is the sum of all signals. For receiving an
ultrasound echo, the phase array works in reverse. The echo from a receive focus is
incident on each array element at a different time interval. The received signals are
electronically delayed so that the delayed add in phase for an echo originating at the
focal point.
In the receive mode, the focal point can be dynamically adjusted so that it coincides with
the range of returning echoes. After transmission of acoustic pulse, the initial echoes
return from targets near the transducer. Therefore, the scanner focuses the phase array
on these targets, located at the first focus. As echoes return from from more distance
targets, the scanner focuses at a greater depth. Focal zones are established with adequate
depth of field so targets are always in focus to receive. This process is called dynamic
receive focusing.
f1
S
f2
time
time
Arrays can be configured as :
Linear sequential array (~512 elements)
Curvilinear (convex) arrays.
Linear phased arrays.
1.5D arrays
2D arrays.
Linear
phased
Linear
Backing
2D array
PZT
Matching
layer
Face plate
Ultrasound is a frequency over 20Khz which is the maximum frequency heard.
But Frequency and wavelength (therefore resolution) are inversely related so the lowest
frequency used is 1 MHz. Axial resolution is approximately wavelength so at 1Mhz it’s
1.5 mm in most soft tissues. So one must go to 1.5 MHz for 1 mm resolution.
Attenuation of ultrasound signals increases with frequency in soft tissue and so tradeoff
must be made between penetration to a particular application. Deep penetration like in
cardiology and Gynecology request 2-8 MHz and application with shallow penetration
like ophthalmology and peripheral vascular use 20 MHz, Intra-arterial uses 20-50 MHz
and in ultrasonic microscopy for inspection of structures within individual cells go up
to 200 MHz.
High frequencies: Good resolution but small penetration.
Low frequencies: Bad resolution but deep penetration.
Two basic equations used in ultrasonic imaging:
1
d tc
2
Where:
d = the one way distance of an object that cause the echo
t = time delay (for the round trip)
c - speed of sound in tissue (between 1450 and 1520 m/s)
The other equation:
S (t ) T (t ) B(t ) A(t ) (t )
Where:
S(t) - Received signal strength.
T(t) - Transmitted signal
B(t) - transducer properties
A(t) - The attenuation of signal path to and from the scatterer
(t) - The strength of the scatterer
In the frequency domain it turns to be:
S ( f ) T ( f ) B( f ) A( f ) ( f )
Definition of terms:
A-mode - The original display mode of ultrasound measurements, in which the
amplitude of the returned echoes along a single line is displayed on an oscilloscope.
B-mode (2-D) - The current display mode of choice. This is produced by sweeping the
transducer from side to side and displaying the strength of the returned echoes as bright
spots in their geometrically correct direction and distance.
M-mode - Followed A mode by recording the strength of the echoes as dark spots on
moving light sensitive paper. Object that move, such as the heart cause standard patters
of motion to be displayed. And a lot of diagnostic information such as valve closure
rates, whether valves opened and closed completely, and wall thickness could be
obtained from this mode.
Transducer
Ribs
Chest wall
Heart in cross section
(diastole-relaxation)
M-line
Heart in cross section
(systole-contraction)
Ultrasound line of sight
Ultrasound is also used for measurement of blood flow in the
blood vessels as shown below:
Returned signal
Transducer
Skin surface
Layers of intervening
tissue
Vessel
Blood flow
Beam
The target is red blood cells in a smallest region as
possible.
One type of system uses the Doppler effect.
The Doppler shift frequency is equal to 2fcvc
fc - transducer center frequency
v - velocity components of the blood cells
c - Speed of sound within tissue.
Color flow mapping - A pseudo color velocity
display overlaid on a 2D gray scale image.
Here simultaneous amplitude and velocity
information is presented.
Ultrasound contrast agents
Reflection of sound waves depend on the acoustic impedance which are defined by
its density and the velocity of sound in the medium.
Acoustic impedances differences are very small between soft tissues.
Echofarnaceuticals (US Cas) have been proposed to increase acoustic impedance
differences at tissue interfaces. Secondly to increase the respective echo intensities.
The most effective principle by far that has emerged is the diffraction of ultrasonic
waves on gas bubbles (microbubble containing solutions ) and colloidal, sometimes
temperature dependent diphasic systems.
Ultrasound contrast agents
Form
Substances
Properties, Indications
Solutions
Shaken saline
Indocyanine green
Gas bubbles, short half life,
difficult reproducabilty,
cavitation and shaking effects
Colloidal emulsions
(foam)
Perfluorooctylbromide,
lipid emulsions
High density, low acoustic
velocity, lower solubilty in
blood, prolongs Doppler
enhancement.
Colloidal suspensions
Iodipamide, ethyl ester,
microparticles
Aqueous microparticle
suspension with very fine gas
bubbles.
Suspensions with gas
microbubbles
Galactose
microparticles
suspension forming
microbubbles
Right heart disease
diagnostics
Fetus Ultrasound