Sepsis
advertisement
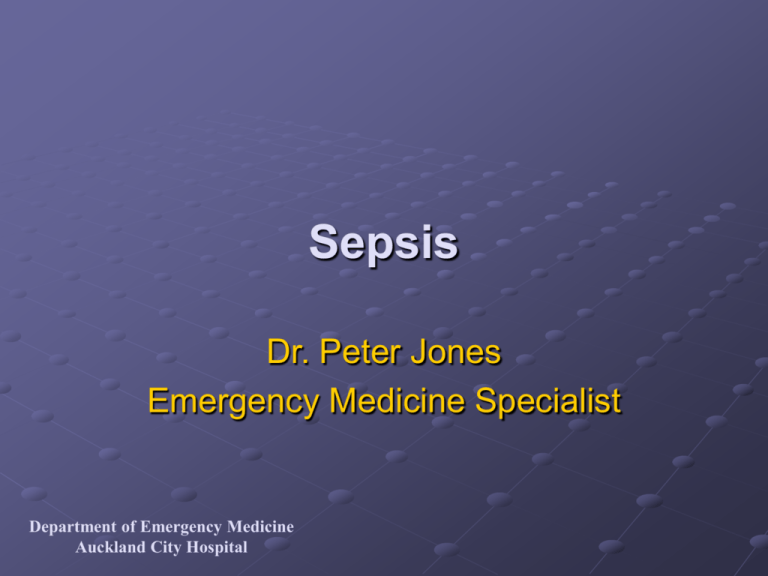
Sepsis Dr. Peter Jones Emergency Medicine Specialist Department of Emergency Medicine Auckland City Hospital Objectives Understand the current nomenclature Know the local organisms Understand the spectrum of presenting illness Get a handle on the basic treatment Introduce novel treatments Department of Emergency Medicine Auckland City Hospital Definitions Sepsis = SIRS + Infection SIRS = 2/4 of Temp >38 or <36 HR >90 Respiratory Rate >20 or PaCO2 <32 (4.3kPa) WCC >12 or <4 or >10% bands Infection = either Bacteraemia (or viraemia/fungaemia/protozoan) Septic focus (abscess / cavity / tissue mass) Department of Emergency Medicine Auckland City Hospital Definitions Cont. Severe sepsis = Sepsis + Organ Dysfunction Organ Dysfunction = Any of SBP <90 or 40 <usual or inotrope to get MAP 90 BE <-5mmol/L Lactate >2mmol/L Oliguria <30ml/hr for 1 hour Creatinine >0.16mmol/L Toxic confusional state FIO2 >0.4 and PEEP >5 for oxygenation Department of Emergency Medicine Auckland City Hospital Definitions Cont. Septic Shock = Severe sepsis + Hypotension Hypotension = either SBP <90 or 40<usual Inotrope to get MAP >90 Department of Emergency Medicine Auckland City Hospital Dear SIRS I don’t like you... Department of Emergency Medicine Auckland City Hospital Definitions Cont. Department of Emergency Medicine Auckland City Hospital High Risk Patients For Sepsis Post op / post procedure / post trauma Post splenectomy (encapsulated organisms) Cancer Transplant / immune supressed Alcoholic / Malnourished For Dying Genetic predisposition (e.g. meningococcus) Delayed appropriate antibiotics Yeasts and Enterococcus Site For Both Cultural or religious impediment to treatment Department of Emergency Medicine Auckland City Hospital Case 1 54yr Samoan male 24 hr Fever and delirium, Arrive 1300hr Initial Obs HR 162, RR 30, sats 95% on 15l, BP 116/82, GCS 13/15 History Migratory abdominal pain and fever 1/7 Examination GCS 15, CNS, CVS, RS, GIT normal 160kg Department of Emergency Medicine Auckland City Hospital Differential Diagnosis (this list is not exhaustive) Pancreatitis Ischeamic Gut Hypovolaemic shock GI bleed / AAA rupture / ectopic / dehydration Cardiogenic shock AMI / Myocarditis / Tamponade PE Toxic Shock Syndromes Staph Aureus Group A Strep Addisonian crisis (note relative adrenocorticoid insufficiency in many septic patients) Thyroid Storm Toxidromes Anticholinergic / serotoninergic Department of Emergency Medicine Auckland City Hospital Investigations Basic WBC Platelets Coags Renal function Glucose Albumin LFT ABG Department of Emergency Medicine Auckland City Hospital Specific ?Source Urine CxR Blood Cultures x 2 LP Aspirate Biopsy May all be normal early on! Treatment Specific Antibiotics Empiric based on source Know local pathogens Use the RMO guidelines / pharmacy handbook for best guess treatment Ideal to get cultures 1st but do not delay antibiotics Surgery Get the pus out! All of it! Early definitive care will improve survival Department of Emergency Medicine Auckland City Hospital Treatment Supportive Oxygenate / Ventilate (6ml/kg) Volume Will need more than ‘maintenance’ + replace losses with like fluid Colloid v Chrystalloid (SAFE trial awaited – know the results!) Inotropes Noradrenalin is inotrope of choice, dopamine next Early ICU referral Department of Emergency Medicine Auckland City Hospital Treatment Supportive Electrolyte homeostasis THAM for pH <7.2 1-2mL / kg over 20min Address co-morbidities ß-Blocker & reduced inotropy DM / COAD Alcoholism / malnutrition / steroids Stop nephrotoxins (NSAIDs) Early ICU referral Department of Emergency Medicine Auckland City Hospital Case 1 54yr Samoan male Investigations FBC, U and E, BC, MSU ABG Treatment IV Fluids 3l 0.9% Saline in 1.5 hours 1l Gelofusin in 1.5hrs IDUC Antibiotics Gentamicin 320mg, Augmentin 1.2gm Past History April 2003 Left ureteric stone, 6mm Referred urology, discharge next day “GP FU” for US Department of Emergency Medicine Auckland City Hospital Case 1 54yr Samoan male Results Urine Dip: 500wbc, no nitirites, 200rbc FBC: wcc 4.67, pmn 3.85 (0.47bands) plt 177 Coag: Inr 1.1, Aptt 26, fibrinogen >7g/L U and E: Na 132, K 4.6, U 10.6, C 0.26 CRP 301.9 ABG: pH 7.36, po2 23, pco2 5.3, hco3 22, be -2.7 Lactate: 3.0 CXR Department of Emergency Medicine Auckland City Hospital Case 1 54yr Samoan male Progress 15:10 hours Urology referral (accepted) DCCM referral (declined) Renal imaging booked : CT 1 2 Progressively hypotensive 55mL urine over 7 hours Declined all treatment Department of Emergency Medicine Auckland City Hospital Case 2 59 Male 29/10 Back pain, lifting fridge Temp 37.3, HR 60 BP 130/60 Tender lumbar area with slight reduction SLR / R leg power PR normal Rx Analgesia, mobilised, discharged home 1/11 Represents 1400 Was getting better then worse again on mobilising Temp 35.8, HR 112 BP 150/80 Asleep when reviewed Findings as above →Treated with analgesia, handed over Kept overnight → Urine test done Department of Emergency Medicine Auckland City Hospital Case 2 59 Male Urine: Trace blood +ve nitrites LFT: “because patient thought he was jaundiced” Bili 23, GGT 167, ALP 157 (40-120) AST 60 (< 40), ALT 72 (< 45) U and E: Na 131. K 3.1, U8.4, C0.09 FBC: Normal (lympho 0.88) Reviewed: Mobilising Discharged with GP Follow up urine Department of Emergency Medicine Auckland City Hospital Case 2 59 Male 2/11/03 Self presented to White Cross Temp 38.8c, GP rang lab → Staph Aureus Referred medical ?pyelonephritis ?Discitis BC done Progress S/B med reg, Rx Flucloxacillin, stop NSAID Delirium / L elbow bursitis MRI: 4/11/03 L2-3 discitis, L psoas abscess, epidural collection - decided not for drainage Discharge with ongoing PICC antibiotics 6 weeks Department of Emergency Medicine Auckland City Hospital Local Susceptibilities There are current hospital recommendations based on local susceptibilities and presumed site of infection on the intranet – USE THEM! Look under Pharmacy, antimicrobial guidelines, best guess therapy Department of Emergency Medicine Auckland City Hospital Department of Emergency Medicine Amoxycillin Nitrofurantoin Norfloxacin Cefuroxime Ceftriaxone Gentamicin Aztreonam / Sulfamethoxazole Clavulanic Acid Trimethoprim Auckland City Hospital Case 1 54yr Samoan male Microbiology results Urine WCC >1000: RCC 310 million/L Bacteria : Present COLONY COUNT : 10 to 100 million/L CULTURE Mixed growth predominantly: (1) E. coli (1) (1) Amoxycillin R Cephalothin S Cefuroxime S Trimethoprim R Gentamicin S Cotrimoxazole R Norfloxacin S Amoxycillin/clav. S Nitrofurantoin S PERIPHERAL BLOOD CULTURE (1) E. coli (1) (1) Amoxycillin R Cephalothin S Cefuroxime S Ceftriaxone S Ceftazidime S Aztreonam S Trimethoprim R Gentamicin S Amikacin S Cotrimoxazole R Norfloxacin S Ciprofloxacin S Amoxycillin/clav. S Ticarcillin/clav. S Meropenem S Nitrofurantoin S Department of Emergency Medicine Auckland City Hospital Trimethoprim Tetracyclines Erythromycin Flucloxacillin Gentamicin Amoxycillin Penicillin Sulfamethoxazole Department of Emergency Medicine Auckland City Hospital Case 2 59 Male URINE MICROSCOPY WCC 170 RCC 30 Epithel. cells <10 million/L Bacteria Present Granular casts 2 million/L CHEMISTRY Protein : Moderate amount COLONY COUNT : > 100 million/L CULTURE (1) Staphylococcus aureus (1) (1) Penicillin R Flucloxacillin S Cotrimoxazole S Doxycycline S Nitrofurantoin S Trimethoprim S PERIPHERAL BLOOD CULTURE (1) Staphylococcus aureus (1) (1) Penicillin R Erythromycin S Flucloxacillin S Doxycycline S Department of Emergency Medicine Auckland City Hospital Metronidazole Clindamycin Augmentin Department of Emergency Medicine Auckland City Hospital Department of Emergency Medicine Auckland City Hospital Amphotericin Local Organisms 1999-2000 ED / AAU / DCCM Positive BC 18/12, n=428 80 Pathogens 70 60 E.Coli S Aureus S Pneumoniae Viridans Strep Klebsiella N Men S Pyo E Cloacae Number 50 40 30 20 10 Organsim IL st yp H FL U KO XY AC IS P PM I SA R G B SF SM Department of Emergency Medicine Auckland City Hospital AS B EC LO SP YO PA C N PA E ST R AS P M R SA vs M IC S P KL E C B O RS P N M EN E PR U O PS SA PN EC C SE PI N S 0 Local Organisms Approx 45-55% positive ED BC are skin organism contaminants Similar across the hospital This is approx 5% all BC done Always get at least 2 blood cultures Help sort out ?contaminants Department of Emergency Medicine Auckland City Hospital Case 1 54yr Samoan male Subsequently declared incompetent by pyschiatry, then consented to treatment Nephrostomy 21:30 DCCM admission (3 days) Noradrenalin CPAP (OSA) Creatinine 0.10 Discharged 2/12/03 Department of Emergency Medicine Auckland City Hospital Local Outcomes Mortality from sepsis varies (Age, co-morbidity, illness severity) DCCM data Auckland Hospital 5-15% for meningitis / brain abscess / pid 20-35% for pneumonia / uti / abdominal 45-50% for mediastinum / joints Data varies from other hospitals ? Due to Policies of DCCM for example Early tracheostomy Admission criteria Department of Emergency Medicine Auckland City Hospital Novel Therapies Steroids JAMA. 2002 Aug 21;288(7):862-71 Many (>50%) septic patients have relative adrenocortical insufficiency. Physiological hydrocortisone improves mortality in this group (63% → 53%, p=0.02 in this study, n=229) Antiinflammatory Department of Emergency Medicine Auckland City Hospital Novel Therapies Activated Protein C (Drotrecogin α) N Engl J Med. 2001 Mar 8;344(10):699-709 Antithrombotic, antiinflammatory, profibrinolytic 1690 patients, Mortality 30.8% →24.7% p<0.01 Increased bleeding 2% →3.5% p=0.06 Caution in meningococcal sepsis / trauma / ICH / pregnant! $17181 / patient Consensus in NZ is restricted last resort use in selected ICU patients Department of Emergency Medicine Auckland City Hospital Novel Therapies Tight glucose control with insulin N Engl J Med. 2001 Nov 8;345(19):1359-67. Mortality reduction 8→4.6% (p<0.04) all icu patients Biggest reductions in severe sepsis / long stayers Also reduced bacteraemic episodes / icu neuropathy Aim 4.4-6.1mmol/L Department of Emergency Medicine Auckland City Hospital Novel Therapies rBacteriocidal/Permeability-increasing protein In neutrophil granules Binds to and inactivates endotoxin Lancet. 2000 Sep 16;356(9234):961-7. 393 Children with clinical meningococcaemia Mortality 9.9% → 7.4% p=0.48 Amputations 7.4% → 3.6%, p=0.067 Better functional outcome 66.3% → 77.3% p=0.019 Department of Emergency Medicine Auckland City Hospital Novel Therapies Summary Reducing mortality in sepsis: new directions Critical Care 2002, 6(Suppl 3):S1-S18 (http://ccforum.com/content/6/S3/S1 ) This is highly recommended reading, concise reviews of Low tidal volume ventilation Early goal directed therapy Drotrecogin alfa (activated) Moderate dose corticosteroids Tight control of blood sugar Department of Emergency Medicine Auckland City Hospital Novel Therapies NAC Crit. Care. Med. 2003 31 (11) 2574-78 Nuclear factor-κB controls expression inflammatory mediators NAC inhibits NFKB in vitro Pilot trial 20 patients, randomised 72 hrs NAC or placebo IL-8 suppressed (may be implicated in lung injury) Recommend larger human trials Department of Emergency Medicine Auckland City Hospital Summary Sepsis may be obvious or subtle early There is a high mortality and morbidity Have a high index of suspicion Know local organisms / susceptibilities Take appropriate cultures Treat early and aggressively Investigate early and aggressively Refer early and aggressively Be aware of new developments Department of Emergency Medicine Auckland City Hospital Antimicrobial Therapy http://ahsl85_gl/FormularyGuide/ Best Guess Department of Emergency Medicine Auckland City Hospital More References Streat S Orientation Lectures for Medical Staff DCCM 12/1/2004 – This hospital’s approach Bone RC Chest 101: 1644, 1992 (Definitions) Vincent JL Crit Care med 1997 25(2) 372-74 Dear SIRS -editorial Angus DC Crit Care med 2001 29 (suppl) 7 s109-s116 – epidemiology Klinzing S Crit Care med 2003 31 (11) 2626-50 – inotropes Department of Emergency Medicine Auckland City Hospital