of Objective Ischemia - Clinical Trial Results
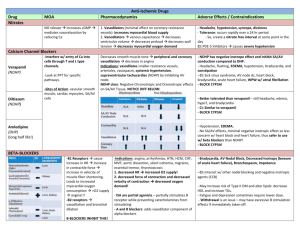
advertisement

The “Truth and Consequences” of Objective Ischemia: The COURAGE Trial Nuclear Substudy Dean J. Kereiakes, M.D. Medical Director, The Christ Hospital Heart and Vascular Center and the Lindner Research Center Chairman,Executive Committee, The Ohio Heart and Vascular Center, Cincinnati, Ohio Professor of Medicine, Ohio State University Objectives • Identify pivotal observation(s) from the COURAGE trial nuclear substudy • Is this observation(s) novel? • Is the obsevation realistic and applicable to clinical practice? • What are the limitations & caveats regarding COURAGE observations? • Summary and Conclusions Nuclear Substudy (n=314 / 2,287) Hypothesis: Reduction in ischemia will be greater for patients Randomized to PCI+OMT than for those randomized to OMT Serial rest/stress myocardial perfusion SPECT (MPS) To compare patient management strategy for ischemia reduction •Pre-Rx = off meds •Post-Rx = on meds Documented Pre-Rx Ischemia PCI + OMT (n=159) OMT (n=155) Repeat MPS* at 6-18m Repeat MPS* at 6-18 m *Timing chosen to occur beyond window of instent restenosis and delayed to allow effects of medical Rx to be observed Source: Shaw et al. J Nucl Cardiol 2006;13:685 MPS Ischemia Based on Total Perfusion Defect (TPD) • • • • • TPD: Quantitative measure of defect extent and severity % Ischemic myocardium = (Stress TPD-Rest TPD) < 5%: Minimal (“no ischemia”) 5.0%-9.9%: Mild 10%: Moderate to severe Defect Extent Defect Severity • Significant reduction in ischemia • 5% reduction in ischemic myocardium* Source: Simoka et al. J Nucl Cardiol 2005;12:66 TPD Lower NI Limit *Threshold exceeds test repeatability Pre-Treatment Clinical Characteristics and MPS Results Compared to main trial, substudy patients more often CCS* class I-II angina (p=0.013) & less multivessel CAD (p=0.05); with similar % of MPS ischemia (p=0.55) PCI + OMT N=159 OMT N=155 P value Angina CCS* Class I-II 74% 73% 0.99 Angiographic 2-3 vessel CAD 73% 77% 0.38 57%11% 58%9% 0.97 8.2% 8.6% 0.63 (7.2-9.3%) (7.5-9.8%) 34% 33% Rest gated LVEF % Ischemic myocardium (95% CI) Moderate to Severe Ischemia** *CCS=Canadian Cardiovascular Society 0.81 ** 10% ischemic myocardium Primary Endpoint: % with Ischemia Reduction 5% Myocardium (n=314) Ischemia Reduction 5% 50 40 33.3 30 P=0.004 19.8 20 10 0 PCI + OMT (n=159) OMT (n=155) % with Low Risk* MPS Ischemia Normalization* on Follow-Up MPS In Patients with Significant Ischemia Resolution 50 P=0.007 40 31.4 30 17.8 20 10 0 PCI + OMT (n=53) *1% ischemic myocardium OMT (n=29) Rates of Death or MI by Ischemia Reduction Death or MI rate (%) 50 RR=0.47 (95% CI=0.23-0.95) 40 30 20 24.7 13.4 P=0.037 10 0 Ischemia Reduction 5%* n=82 No Ischemia Reduction n=232 *primary endpoint Rates of Death or MI by Ischemia Reduction in Subset of 105 Patients with Moderate to Severe Pre-Rx Ischemia* Death or MI rate (%) 50 P=0.001 40 32.4 30 20 16.2 10 0 Ischemia Reduction 5% No Ischemia Reduction n=68 n=37 *50% reduction Rates of Death or MI by Residual Ischemia on 6-18m MPS P=0.002 Death or MI rate (%) 50 P=0.023 40 30 P=0.063 39.3 22.3 15.6 20 10 0 0.0 0% (n=23) 1 - 4.9% (n=141) 5 -9.9% (n=88) 10% (n=62) Conclusions • PCI added to OMT was more effective in reducing ischemia and improving angina than OMT alone, particularly in patients with moderate to severe pre-RX ischemia • Is this Observation Novel? Cardiac Death or Myocardial Infarction Rate/Year Stratified by SPECT Quantitative Ischemia 5 Myocardial Infarction Cardiac Death 4 Event Rate % 4.2* 2.9 2.7 ** 3 2.9* 2.3 2 1 0.3 0 0.5 Normal N= 2946 0.8 Mildly Normal 884 Moderately Abnormal 455 Severely Abnormal 898 * Statistically significant increase as function of scan result ** Increased rate of MI vs cardiac death within scan stratum Hachamovitch, Diamond et al. Circ 1998;97:535 Cardiac Death Rate Stratified by Spect Quantification of Ischemia and Treatment Modality† Medical RX Cardiac Death Rate (%) 10 Revasc * 8 6.7 § 6.3 6 4.8 3.7 4 2 2.9 1.0 0.7 3.3 2.0 1.8 0 7110 16 1331 56 718 109 545 243 252 267 0% 1-5% 5-10% 11-20% >20% *p < 0.0001 % Total Myocardium Ischemic †10,627 Consecutive patients followed 1.9 + 0.6 years. Hachamovitch et al. Circ 2003;107:2900 Mortality Hazard by Treatment Modality and % Ischemic Myocardium log Hazard Ratio (Mortality) 6 5 Medical Rx * 4 3 Revasc * 2 1 0 0 12.5% *p<0.001 Interaction: p=0.030 25% 32.5% 50% % of Total Myocardium Ischemic Hachamovitch et al. Circ 2003;107:2900 Relationship Between Baseline Findings and Treatment Strategies with Adverse Outcomes* to 1 Year: ACIP Study** O.R. (95% CI) P Ischemia Driven Medial Therapy 0.80 (0.39 – 1.61) 0.41 Revascularization 0.56 (0.26 – 1.2) 0.05 1.06 (1.01 – 1.12) 0.002 Strategy AECG Ischemia† 0.25 0.5 1.0 1.5 1.75 Adapted from Pepine et al. JACC 1997;29:1483 † 48 hours monitor qualifying visit *Death, non-fatal MI, hospital admission for ischemic event, **558 pts. Objective ischemia Ambulatory ECG and SPECT Perfusion Imaging: Lack of Concordance (ACIP Ancillary Study*) AECG + + - 45 / 48 33 / 34 20 / 17 8/7 SPECT - 50% Concordance ( 3% perfusion defect) 52% Concordance (+ any ischemic defect) Adapted from Mahmarian et al. JACC 1997;29:764-9 ACIP Study Two-Year Follow-Up Death or MI 16 12.1% Angina Guided Med Rx 12 percent 8.8% Ischemia Guided Med Rx 8 4.7% Revascularization * 4 0 0 4 8 12 16 20 Months of Follow-up *P<0.01 vs. angina guided med Rx 24 Davies et al. Circ 1997;95:2037 Cardiovascular Death or Myocardial Infarction Stratified by Self-Reported Angina and/or Inducible Ischemia*: The Heart and Soul Study Adjusted HR† (95% CI) p No angina or ischemia 1 (Reference) Angina alone 1.4 (0.7, 2.9) 0.31 Ischemia alone 2.2 (1.4, 3.5) 0.005 Angina & Ischemia 3.2 (1.4, 7.2) 0.006 0.5 1 2 3 4 5 6 7 8 9 *stress echo (937 pts. Stable CHD followed 3.9 yrs.) † Adjusted for age, sex, race, Hx MI, Hx CHF, HgA1c, CrCl, LVEF, SBP, DBP, CRP Adapted from Gehi, Schiller, Whooley et al. Arch Int Med 2008;168:1423 • Is the COURAGE Trial observation Realistic and Applicable to Practice? COURAGE : Demographics 19 US Non-VA Hospitals 387 pts (0.5 pts/mo/hosp) *(17% of total) 15 VA Hospitals 968 pts (1.6 pts/mo/hosp) (42% of total) 50 Hospitals 2,287 pts* enrolled between 6/99-1/04 1 pt per hospital 16 Canadian Hospitals per month 932 pts (1.5 pts/mo/hosp) (41% of total) * 15% women,14% non-caucasian Boden WE et al. NEJM 2007;356:1503-16 Does COURAGE Represent U.S. PCI Practice ? 2000 US VA US non VA 1800 1,422 1600 1400 (96.5%) 962,732 1,200,000 (98.5%) 1,000,000 800,000 1200 600,000 1000 800 600 400 400,000 52 200,000 (3.5%) 14,268 (1.5%) 200 0 0 Hospitals with PCI * * 2006 Total PCI Volume* Boden WE et al. NEJM 2007;356:1503-16 ; US data on file, Boston Scientific COURAGE : Inadequate and Incomplete PCI PCI success 1149 patients total 46 (4%) procedure not attempted 27 (2%) no lesions crossed 14% PTCA only 86% stents 97% BMS 3% DES 1077 pts had PCI attempted / 958 (89%) success [really 958/1149 (83.4%)or 958/1122(87%) success]* Complete Peri-PCI revascularization MIs 1577/1688(1730)* lesions had PCI success (93%) Few PCI pts received GPIIb/IIIa inhibitors, bivalirudin *Really <8991%*(add 1.6 or adequate clopidogrel pre-loading lesn x27 pts) 787 pts (69%) had 2 or 3 vessel ds. 416 pts (36%) received ≥2 stents At least 371 of 787 pts (47%) with multivessel disease had incomplete revascularization *SITE COURAGE : Variable PCI Outcomes by Location Original Trial Hypothesis: 22% reduction D/MI with PCI OMT Death/MI (%) at 4.6 years 30% PCI+OMT P≈0.02 25% 22% 22% 20% 15% 17% 21% 15% 14% 10% 5% 27%↑ 29%↓ Canada US VA US non-VA 0% COURAGE: Mortality by Healthcare System and Randomized Treatment Strategy % Mortality 14 OMT 12.1 12 P =0.07 10 8.6 8 7.9 PCI + OMT 7.7 6.0 6 4.7 4 2 0 USVA USNVA Canadian Adapted from Chaitman et al. JACC 2008;51:A222 (abstract) COURAGE Issues :? Geographic Selection Bias Original Projection: 3-year death/MI for OMT = 21% Death/MI (%) at 4.6 years 30% 25% 20% Very low risk pts! Hard to improve upon 22% 19% 21% 14% 15% Probably ~10% at 3 years 10% 5% N=2287 N=932 N=968 N=387 All Canada US VA US non-VA 0% ~ 0.4% /Yr Cardiac Mortality in COURAGE NEJM 2007;356:1503 AHJ 2006;151:1173 Imputed* Effect of Drug-Eluting Stents in the COURAGE Trial: Death / MI RR (95% CI) BMS+OMT vs. OMT (COURAGE) 1.05 (0.87,1.27) DES+OMT vs. BMS+OMT (historical meta-analysis) 1.30 (0.91,1.86) 1.03 (0.84,1.26) DES vs. OMT (indirect comparison) 0.00 BMS *Annals Int Med 2006Meta-analysis Favors Favors PCI OMT 0.50 1.00 1.50 SES (Cypher) 2.00 2.50 1.36 (0.91, 2.04) 1.08 (0.82, 1.43) PES (Taxus) Diamond, Kaul Viewpoint JACC 2007;50:1604-1609 Clinical Events Following BMS or DES*+ 24 20 16 TARGET LESION REVASCULARIZATION CLINICALLY DRIVEN TLR (Taxus IV Non-Angio Cohort) 24 BMS (EXP+Bx) PES SES BMS (Exp) n = 295 PES n = 287 20 16 12 12 % % p=0.0005) 8 8 4 4 0 0 0 SES vs. BMS: PES vs. BMS: SES vs. PES: BMS 4763 PES 6328 SES 6621 1 2 3 4 HR 0.30 (0.24-0.37; p<0.0001) HR 0.42 (0.33-0.53; p<0.0001) HR 0.70 (0.56-0.84; p=0.0021) 820/4746 53/2795 22/1871 448/6280 98/3950 15/1999 356/6580 68/3801 16/2153 *Stettler et al. Lancet 2007;370:937 n=18,023 patients / 38 trials 10/1543 6/832 14/999 0 1 PES vs. BMS: 2 3 4 HR 0.39 (0.23-0.67; p=0.0005) BMS 295 37/254 PES 287 8/272 5/249 3/239 1/229 2/218 4/271 3/258 2/246 3/235 +Boston Scientific data on file 5 Clinical Events Following BMS or DES* ALL DEATH Cumulative Incidence in % 10 14 BMS PES SES 8 6 DEATH OR MYOCARDIAL INFARCTION Cumulative Incidence in % BMS PES SES 12 10 8 6 4 4 2 2 0 0 0 SES vs. BMS: PES vs. BMS: SES vs. PES: 1 2 3 4 0 HR 1.00 (0.82-1.25; p=0.89) HR 1.03 (0.84-1.22; p=0.75) HR 0.96 (0.83-1.24; p=0.80) BMS 4921 109/4904 PES 6331 138/6283 SES 6771 139/6730 48/3340 78/4263 72/4041 *Stettler et al. Lancet 2007;370:937 n=18,023 patients/38 trials 31/2264 32/2187 38/2340 44/1875 15/869 24/10810 1 2 3 4 HR 0.92 (0.77-1.08; p=0.32) HR 1.00 (0.84-1.23; p=0.97) HR 0.92 (0.79-1.08; p=0.27) 4921 6331 6771 301/4904 62/3208 45/2161 46/1780 376/6283 115/4087 43/2082 22/833 356/6730 86/3888 44/2241 28/1032 Mortality (DES vs. BMS) from 29 Trials / Registries Patient Year Weighted Regression* Slope = 1.0 14 TSEARCH 2 BASKET 3 DEScover 4 STENT 5 Steinberg et al. 6 REAL 7 ONASSIS Slope = 0.85 8 [95% CI] 12 Slope = 0.79 19 24 8 6 29 26 27 4 18 2 12 17 10 7 17 Ortolani 18 Cypher meta-analysis 19 Taxus SR meta -analysis 20 Ontario PCI Registry 21 WAKE Forest DES Death = 0.79 BMS Death 22 ACUITY 95% CI Slope = 0.79 ± 0.06 R2 = 0.96 23 PASSION 24 RESEARCH 25 SESAMI 26 NY State 27 ASAN 28 GHOST 29 MIDAS 1 11 9 0 0 28 21% Decrease 16 13 2 4 6 8 % Death BMS SCANDSTENT MISSION 21 25 11 16 20 22 DIABETES SCAAR 3 2 10 15 5 8 PRISON II Western Denmark 14 23 9 14 15 4 6 Pache et al. Slope = 0.73 12 TYPHOON [95% CI] 13 SES Smart 10 % Death DES 1 10 12 14 Size of circle adjusted for number of patients DES vs. BMS Registries: All Cause Mortality % BMS 20 DES 18 11.0 7.9 7.8 Follow-up: 3 year 3 year 2 year 2 year 3 year 5,441 5,441 MIDAS NY STATE ONTARIO MASS-DAC STENT 3,751 GHOST 3,751 ASAN 6,384 5,399 5,719 4.8 6.4 5.7 5.5 871 483 0 4.2 p=0.004 9.4 5.6 5.2 p<0.001 4,061 3,180 2 11.9 8.6 5.9 p<0.001 2 year 2 year 3,548 10 4 p<0.001 11.5 12 6 p<0.05 12.9 14 8 p<0.0001 8,847 p=0.052 1,359 5,996 p<0.001 7,834 16 Western Denmark 2 year DJK Late (3 Year) Results of the SCANDSTENT Randomized Trial* p<0.001 SES BMS 40 p<0.001 p<0.001 37.6 34.4 33.8 35 Events, % 30 25 20 p=0.14 p=0.69 p=0.04 12.3 15 10 5 0 9.6 5.6 1.9 Death 2.5 1.3 3.7 Cardiac death Myocardial infarction * CTO, ostial, bifurcation, angulated 8 4.9 TLR TVR MACE Kelbaek et al. JACC 2008;51:2011 DES Outcomes (2 Years) in the Elderly: Medicare Case-Control Comparison* 50 p<0.001 DES BMS p<0.001 p<0.001 p<0.001 % Patients 40 34.4 29.8 30 17.2 19.1 20 10.7 13.5 10 0 Death 9.2 11.2 Myocardial Infarction *n=76,525 DES Rx vs. contemporary (April-Dec 2003) controls Coronary Combined Revascularization Endpoints Adapted from Groeneveld et al. JACC 2008;51:2017 Outcomes Following Coronary Stenting in Medicare Beneficiaries* Repeat Revascularization 0.30 Death/STEMI 0.12 Cumulative Hazard 0.10 0.20 0.08 0.06 0.10 0.04 0.02 0.00 0.00 1 90 180 # at risk BMS 38917 35610 33155 DES 28086 25660 24386 365 30437 22737 730 26822 19943 1 90 180 365 38917 38001 37362 28086 27473 27021 36332 26301 730 34275 24311 *BMS 38,917 10/02 - 3/03 DES 28,086 09/03 - 12/03 BMS era DES era Malenka et al. JAMA 2008;299:2868 DES Versus BMS and All-Cause Mortality: CCF Experience Non-Propensity Matched* Event Free Propensity Matched Event Free 1.0 1.0 0.9 0.9 0.8 0.8 0.7 0.6 1 Drug-Eluting Stent Bare-Metal Stent Confidence Interval 0.7 HR (95% CI) 0.62( 0.53 - 0.73) 0.0 0.5 1.0 1.5 2.0 2.5 3.0 3.5 4.0 No. At Risk Years after Procedure Drug Eluting Stent: 6053 5467 4771 3939 3145 2295 1552 791 170 Bare-Metal Stent: 1983 1538 1241 1082 990 905 815 723 515 *p<0.001 0.6 1 0.0 Drug-Eluting Stent Bare-Metal Stent Confidence Interval 0.5 1.0 1.5 2.0 HR (95%CI) 0.54(0.45-0.66) 2.5 3.0 3.5 4.0 No. At Risk Years after Procedure Drug Eluting Stent: 1801 1654 1466 1251 1037 791 536 261 57 Bare-Metal Stent: 1801 1390 1117 969 884 809 733 653 471 Shishenbor et al. JACC 2008 52:1041 COURAGE : Freedom from Angina with OMT PCI + OMT 100 OMT P=NS Angina free (%) 80 74 40% P<0.001 72 CCS Class 0 / 1 P=NS 60 42 43 <10% crossovers* prespecified! 40 32 22 20 0 Angina free at 5 years Baseline absent or minimal symptoms Revascularization after discharge *due to severe / progressive angina ; remain OMT by ITT Multivariate Predictors of Crossover to PCI OR (95% CI) Hypercholesterolemia 1.4 (1.0 - 2.0) 3 VD 1.6 (1.1-2.3) SAQ angina frequency score 0.5 0.86 (0.81-0.91) 1.0 1.5 2.0 2.5 Adapted from Spertus et al. JACC 2008;51:A264 (abstract) COURAGE : “COURAGE” OMT not Realistic Compliance Follow-up Aspirin Statins Beta blockers 1 years 95% 95% 89% 3 years 95% 92% 86% 5 years 94% 93% 86% Treatment to Targets LDL < 85 mg per deciliter in ~70% of pts SBP <130 mmHg in ~65% of pts DBP <85 mmHg in ~ 94% of pts HgBA1C <7.0% in ~45% of diabetic pts Medication Compliance CRUSADE Registry (1-Year) vs. 95% in COURAGE vs. 95% vs. 89% vs. >90% vs. >90% Mehta HR et al. Circulation 2005;112:II-793. Compliance with Guideline Recommended Therapies in Patients with Established Atherosclerosis: The REACH International Registry Previous PCI (n=12,759) Previous Medical Rx (n=13,784) 100 90 % Patients 80 70 82 69 86 70 66 55 60 50 40 30 20 10 0 Aspirin B-Blocker Statin/Lipid Lowering Adapted from Steinberg, et al. Am J Cardiol 2007;99:1212 Medical Compliance Effects Survival in CAD 1.00 0.95 0.90 0.85 0.80 0.75 0.70 0.65 0.60 0.55 0.50 BETA-BLOCKERS Survival (adjusted) Survival (adjusted) STATIN 0 1 2 3 4 5 6 Years Adherent 7 8 1.00 0.95 0.90 0.85 0.80 0.75 0.70 0.65 0.60 0.55 0.50 0 1 2 3 4 5 6 7 8 Years Non-Adherent Ho et al. Am Heart J 2008;155:772 % Patients Optimal (<140/90 )* Blood Pressure Control in Clinical Practice 1J 31% 37% 33% Three City Study1 Silvia Study2 NHANES 2003 – 20043 (n=9090) (n=2775) (n=1614) HTN 2006;24:51, 2J HTN 2004;22:2387, 3HTN 2007;49:69 * < 130(65%) / 85(94%) COURAGE Freedom from Angina ( SAQ ) Stratified by Treatment 60 PCI + OMT OMT P<0.001 P<0.001 P=0.005 P=0.010 P=0.30 50 Angina-free (%) P<0.001 40 30 P=0.35 20 10 0 Baseline n = 21 23 1 3 42 33 53 42 6 12 24 36 56 47 57 50 59 53 59 56 Months Weintraub et al. N Engl J Med 2008;359:677 Angina Stability and Frequency by SAQ over Time Stratified by Treatment Strategy Angina Stability Angina Frequency 90 PCI + OMT 90 OMT 80 * * * Mean Score 100 Mean Score 100 * 70 60 50 0 0 * 70 60 50 6 12 24 Months from Baseline *p<0.01 80 * * * * 36 0 0 6 12 24 36 Months from Baseline Weintraub et al. N Engl J Med 2008;359:677 Quality of Life by SAQ Over Time Stratified by Treatment Strategy PCI + OMT OMT 100 Mean Score 90 80 * * * 6 12 * * 70 60 50 0 0 24 36 Months from Baseline *p<0.01 Weintraub et al. N Engl J Med 2008;359:677 COURAGE Objective Ischemia : Conclusions • Ischemia (SPECT,AECG,SECHO) is qualitatively and quantitatively correlated with adverse clinical outcomes (CVD,MI) • Revascularization (PCI) is more effective in reducing ischemia than medical therapy (OMT) • COURAGE PCI was inadequate (83-87% per-patient ; <89-91% per-lesion success rate) and incomplete (47% MVD) with suboptimal technology (14% POBA, 3% DES) COURAGE Objective Ischemia : Conclusions • COURAGE OMT was unrealistic (>90% compliance through 5 years) in part due to free nurse case management and free medications • Contemporary “real world practice management” (more complete revascularization with DES, less optimal medical compliance) would likely enhance the relative magnitude and durability of demonstrated PCI benefit (angina relief, improved QOL, ischemia reduction)