Drugs & Neurotransmitters
advertisement

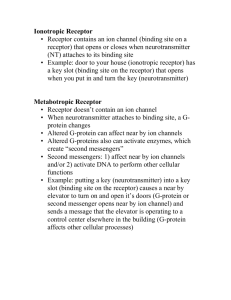
Drugs & Neurotransmitters At a substrate level Nerve condution nonspecific irreverseible inhibition - MAOIs specific reversible MAO A (5HT) - moclobemide MAO B (NA, DA) seleziline Neurotransmitter release Serotonin/SSRIs N.A./Serotonin - SSRIs; TCAs MAO more is less and less is more (SSRIs & neurolepts) Neurotransmitter reuptake ~ Role ions; Ca++ & ?Mg+ to stabilise ? One site of Li action subsequent reduced neurotransmitter release Presynoptic Autoreceptors ~ Tryptophan increases serotonin substrate potentiation of other serotonergic meds Amphetamine & DA; serotonin & ecstasy Neurotransmitter breakdown in synapse Tacrine inhibits those relevant cholinesterases Receptors Note various classes; all have some common features cross tolerance - compounds other than the usual neurotransmitters may act on them eg etoh, phenobarbitone bind to the same ion channel is GABA and diazepam to Agonise it. Penicillin and picrotoxin bind and turn it off. Chronically this will affect the receptor sensitivity Up & Down Regulation Chronic exposure to high and low concentrations of neurotransmitters (or any substance acting as a receptor) will result in adaptation. Too much for a long time makes the receptors less sensitive and vice versa. The mechanism for this varies; receptor number, receptor shape, and second messenger systems all involved. Autoreceptors on the presynoptic neorone when stimulated provide negative feedback to reduce release of neurotransmitters Agonism/Antagonism If a compound binds to a receptor, it will have some effect. “Full” agonist when bound to a receptor, will turn it on fully. Partial agonist when bound will only partially stimulate the effects. Thus, no matter how much you give, maximal effect (as compared to full agonist) won’t happen. Antagonist binds to a receptor and doesn’t turn it on. Because its occupying the site, no one else (even the usual neurotransmitter) can’t get on. Reduced effect. Note that things that bind to receptors may bind as firmly and not be removable; or loosely and be ‘knocked’ off if enough competition is present. Second messengers Probably some agents work here. Lithium appears to reduce the second messenger response to catecholamines; it reduces the response to TSH & ADH. Thus, the receptors are there in normal numbers; but nothing happens. This system can also be increased eg. Theophylline phosphodiesterase inhibition AMP Neurolepts At least in typical neurolepts, potency correlates to D2 receptor blockade Relevant Dopaminergic pathways mesolimbic • ~ emotion, cognition ~ = effect mesocortical nigrostriatial = parkinsonian S/E tube - hyothalamus - pituitary = Prolectin Around 70% D2 receptor occupation/blockade ~ correlates to maximal antipsychotic effect At 80% occupancy movement disorders occur in most Mechanism Recently focused as Autoreceptor blockade, thus reduced negative feedback & subsequent increased initial DA secretion; eventual adaptive response (“depolarisation blockade’) results in reduced dopominergic transmssion. Recent experimental drugs which specifically stimulate autoreceptors appear to be antipsychotic (by increasing negative feedback - reduced DA transmission) SSRI’s/TCAs Clozapine and olanzapine, binding to D4 more than D2 imply that this receptor, with different pathwyas, may be more important in psychosis and possible role of serotonin, NMDA and other receptors Tardive dyskinesia ~ at present thought to result from D2 receptor upregulation due to chronically reduced transmission. Thus they are supersensitive and react excessively to normal, or subnormal amounts of DA. Block reuptake at serotonin/noradrenaline variosly. Not only do they vary in which neurotransmitter system they affect; they also vary in potency at different sites (much like partial vs full agonists). Thus a flat dose response curve may occur; each drug can only block reuptake so much; after that no further benefits, but potential side effects. Mode of action 1. Inhibition of reuptake of neurotransmitter amines increases the amount in synaptic cleft, increasing transmission. Delay in onset of action due to part synaptic adaptation. 2. Presynoptic autoreceptors stimulated by excess serotonin. Initial reduction in serotonergic transmission, less serotonin in synoptic cleft and subsequent autoreceptor down regulation. Eventually neurone adapts to increase serotonergic transmission and not be inhibited by normal concentrations of serotonin. Reverse of neurolepts : more is less and less is more. Diazepines At least we understand this mechanism. Diazepines, like many other drugs, bind at a specific site on the GABA receptor to increase chloride ion flux into the neurone, making it hyperpolarised and refractory to stimulation. Alcohol, barbiturates and some other sedatives also act on GABA, and their chronic use potentiates tolerance to diazepines. Penicillin and pirotoxin bind to the receptor to reduce its effect - a mechanism of penicillin related seizures. Cross tolerance is common here. Lithium multiple theories, not sure appears to increase serotonin secretion in some models reduces postsynoptic response to noradrenaline (inhibits AC) ? Direct effect on nerve membrane