Slide 1
advertisement
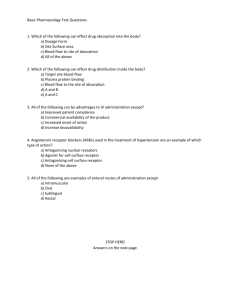
Nomenclature: Every drug has three names: 1) Chemical Name: The drug is named according to its chemical structure. 2) Generic name (common name): Non proprietary name is assigned to the drug to be easy to remember. It should reflect some important pharmacologic or chemical characteristics of the drugs. 3) Brand name (trade name): Proprietary name is privately owned by the manufacturer to distinguish certain drug product from the other. The name may have an indication to its therapeutic use or the name of the manufacture. e.g. Aspirin Chemical name: Acetyl salicylic acid Generic name: Aspirin Brand name: Rivo Aspocid Juspirin Alexoprin e.g. Acetaminophen Chemical name: N-acetyl-p-amino phenol Generic name: Acetaminophen (USP) or Paracetamol (BP) Brand name: Abimol Paramol Panadol e.g. Ketoprofen Chemical name 2-(3-benzoylphenyl) propanoic acid Generic name: Ketoprofen Brand name: Ketofan Alcofan Profenid Pharmacodynamics How do drugs act? Drugs can produce their effects through one or more of the following mechanisms. 1) Drug-receptor interactions: The cells in certain tissue contain structures called receptors. Receptors are macromolecules component of the cell that bind the drug to produce a response. Receptors are located at cell membranes or in the cell nucleus. The drug is thought to fit onto a receptor like a key fits a lock. The ability of the drug to bind to the receptor depends on the bond formed between the drug and the receptor. [D] + [R] [DR] Response Agonist: A drug which can bind to a receptor to produce a response. Antagonist: A drug which bind to receptor and produce no effect (compete with the agonist and inhibit its effect). 2) Antimetabolites/cytotoxic: Drug act by impairing cell reproduction. This means that the affected cells may remain alive and may continue to carry out many of their functions, but are unable to reproduce successfully, leading to cell death (Methotrxate, Cyclophosphamide). The drug may resemble substances which are used by the cells for nutrition and when absorbed, the cells can not used them and so failed to multiply. The sulphonamides which are used to stop the multiplication of bacteria are good example. They are very similar in structure to para- aminobenzoic acid and certain bacteria can not distinguish between them and sulphonamides and stop generation. absorb the 3) Action on enzymes: Enzymes are substances which speed up many chemical processes within the body. Drugs may produce their effects through inhibition or stimulation of certain enzymes. Sulphonamides are used as antibacterial agents as they inhibit folate synthase enzyme so decrease the synthesis of folic acid by bacteria death 4) Action on cell membrane: The action of nerves and muscles depends on ions passing across the membranes surrounding these cells. Certain drugs interfere with the movement of these ions and thus prevent nerve or muscle function (local anaesthetics). 5) Chelating agents: Adsorb drugs, substances in electrolytes the or intestine to biological form non- absorbable complex that is excreted in the feces (Cholestyramine). Activated charcoal is used as a non-specific antidote in treatment of poisoning as it adsorbs poisons on its surface absorption from the GIT. and inhibit their Pharmacokinetics I. Drug Absorption II. Drug Distribution III. Drug Metabolism IV. Drug Excretion These factors determine the drug dose frequency administration and of I. Drug Absorption Absorption is the transport of drug from the site of administration to the blood stream. Drugs must be librated and dissolved before it can be absorbed into systemic circulation. Absorption involves the passage of the drug across cell membranes. II. Drug Distribution After the drug reaches the blood stream, the drug is distributed through the body fluids and tissues. Drugs exist in two forms: bound and unbound (free) forms. The protein-bound drug is inactive and not subjected to metabolism or excretion. The binding capacity of plasma protein is limited. Once saturation has been reached, a small increase in drug dose increase in free drug concentration pharmacological activity. Competition of drugs for binding to plasma protein serious drug interactions. Aspirin + Warfarin Aspirin displaces warfarin from plasma protein bleeding.