Histology of Muscle
advertisement

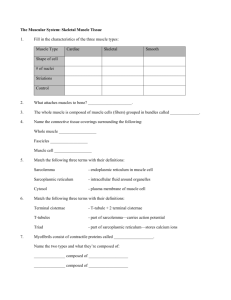
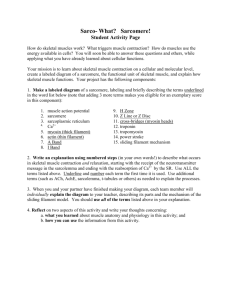
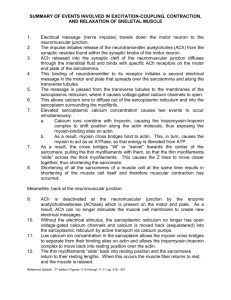
Biology 211 Anatomy & Physiology I Dr. Thompson Histology of Muscle Three types of Muscle Tissue Skeletal Muscle Myocytes Very long Unbranched Nuclei Cardiac Muscle Shorter Branched Hundreds per cell One or two per Peripheral cell Central Striations Yes Voluntary Smooth Muscle Short, Unbranched Spindle-shaped One per cell Central Yes No Involuntary Involuntary Muscle: Special Terminology: Prefixes = Cell = Myo- / Sarco- Myocyte ("Fiber") Plasma membrane = Sarcolemma Endoplasmic reticulum = Sarcoplasmic reticulum Cytoskeletal Filaments = Myofilaments We will discuss cardiac muscle and smooth muscle in later lectures. Let’s focus on Skeletal Muscle: Always voluntary: Each myocyte connected to and controlled by an axon from a motor neuron. High metabolism, so myocytes very close to capillaries. Myocytes are all oriented parallel to long axis of muscle which is Parallel to direction which muscle pulls when it contracts & lengthens when it relaxes Skeletal Muscle Anatomy: Each myocyte surrounded by, and firmly attached to, layer of loose connective tissue called endomysium Endomysium Skeletal Muscle Anatomy: Myocytes grouped together into bundles called fascicles; each fascicle surrounded by, and firmly attached to, layer of dense irregular connective tissue called perimysium Perimysium Skeletal Muscle Anatomy: Entire muscle surrounded by, and firmly attached to, layer of dense irregular connective tissue called epimysium Epimysium Skeletal Muscle Anatomy: All three layers of connective tissue blend together at each end of muscle. Thus, force is transmitted from: Myocytes Endomysium Perimysium Epimysium Tendon, bone, etc. I A I A I H Z Z Z Sarcomere A I Z Myocyte Contraction Requires: Stimulus from motor neuron (nerve cell) Spread of stimulus along sarcolemma and into myocyte through transverse tubules Release of Ca++ from sarcoplasmic reticulum into cytoplasm of myocyte Binding of calcium to thin myofilaments Formation of cross-bridges between thin myofilaments and thick myofilaments Myoneural junction or Neuromuscular junction Stimulation of the myocyte begins when the neuron releases a chemical neurotransmitter from its synaptic vesicles into the synaptic cleft between the neuron and the myocyte. The neurotransmitter diffuses across the synaptic cleft and binds onto receptors located on the sarcolemma of the myocyte. This causes an electrical change of the sarcolemma called “depolarization” When resting, the sarcolemma of the myocyte is polarized. Sodium ions concentrated on its outer surface & potassium Ions concentrated on its inner surface. Large negative ions (proteins, phosphate, sulfate, etc) also concentrated on the inner surface. Net effect: outer surface of sarcolemma more positive inner surface of sarcolemma more negative Sodium channels and potassium channels are closed. When neurotransmitter binds onto its receptors on the sarcolemma, sodium gates (or "gated channels") open. For now, don't worry about what causes this to happen. Sodium ions, carrying their positive charges, flow into the cell, making the inner surface of the sarcolemma more positive. The sarcolemma has begun to depolarize. A few milliseconds later, potassium gates on the sarcolemma open while the sodium gates close. Potassium ions, with their positive charges, flow out of the cell, again making the outer surface of the sarcolemma more positive. but Sodium and potassium ions are mixed together on both sides of the sarcolemma After both the sodium gates and the potassium gates have closed, “sodium potassium pumps” - Push sodium ions back to the outside of the sarcolemma and - Push potassium ions back to the inside of the sarcolemma. This returns the sarcolemma to its original “polarized” condition. It is ready to depolarize again. This depolarization / repolarization spreads along the sarcolemma in all directions away from the myoneural junction When the signal reaches the openings of transverse tubules, these carry it deep into the myocyte As the signal travels along the transverse tubules, it stimulates the sarcoplasmic reticulum to release large amounts of calcium ions (Ca++) into the cytoplasm of the myocyte This calcium binds onto troponin of the thin myofilament which moves the tropomyosin to expose active sites on actin Myosin head groups can now bind to the actin, forming cross bridges, after which they flex to move the thin filament These cross-bridges form between myosin molecules of the thick filaments and actin molecules of the thin filaments where these overlap in the A-band As long as calcium ions bind to troponin of the thin myofilament: - Cross-bridges will continue to form between thin and thick myofilaments, so - Myocyte will remain contracted Therefore: To make myocyte relax (no crossbridges form), calcium ions must be removed from thin myofilaments Which means The calcium ions must be removed from the cytoplasm of the myocyte Relaxation occurs when calcium ions are removed from the cytoplasm. by being pumped into the sarcoplasmic reticulum (thus out of the cytoplasm), where it is not available to bind to troponin. Sarcoplasmic reticulum takes up calcium ions only if no electrical signals are travelling down transverse tubules which Happens only if the sarcolemma is not being stimulated by a motor neuron Quick Summary Contraction Relaxation Motor neuron stimulates sarcolemma of myocyte Motor neuron stops stimulating sarcolemma Stimulus spreads along sarcolemma & into myocyte through transverse tubules Sarcolemma stays polarized This causes release of Ca++ from sarcoplasmic reticulum into cytoplasm of myocyte Calcium binds to thin myofilaments Cross-bridges can now form between thin myofilaments and thick myofilaments Sarcoplasmic reticulum pumps calcium back into its lumen, removing it from the cytoplasm Thin myofilaments change shape Cross-bridges break between thin and thick myofilaments One motor neuron + All myocytes it innervates = one Motor Unit Skeletal Muscle: 1. Myocytes and muscles always pull (exert force by contraction), they never push. They usually, although not always, pull on bone through a tendon. 2. If a sarcomere shortens, it always does so completely "All-or-none" 3. All of the sarcomeres in the entire myocyte shorten at the same time. "All-or-none" But: 4. All of the myocytes in a muscle don't always contract at the same time. No "all-or-none" Skeletal Muscle: The total force produced by a myocyte is equal to the sum of the forces produced by individual sarcomeres. Thus: More sarcomeres = more force The total force produced by a muscle is equal to the sum of the forces produced by individual sarcomeres. Thus: More myocytes = more force