439EnFemRepro16
advertisement

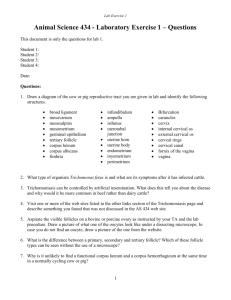
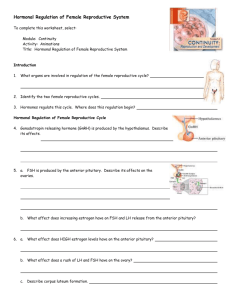
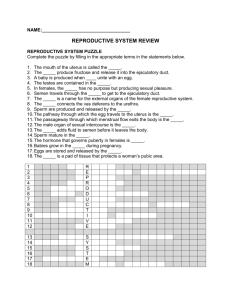
FEMALE REPRODUCTIVE SYSTEM FEMALE REPRODUCTIVE SYSTEM TO REVIEW THE COMPONENTS OF THE FEMALE REPRODUCTIVE SYSTEM TO CHARACTERIZE THE GENERAL ORGANIZATION OF THE OVARIES TO UNDERSTAND THE HORMONAL REGULATION OF OOGENESIS, OVULATION, AND THE UTERINE CYCLE Hormones of the Female Reproductive Cycle • Control the reproductive cycle • Coordinate the ovarian and uterine cycles Hormones of the Female Reproductive Cycle • Key hormones include: – FSH • Stimulates follicular development – LH • Maintains structure and secretory function of corpus luteum – Estrogens • Have multiple functions – Progesterones • Stimulate endometrial growth and secretion FEMALE REPRODUCTIVE SYSTEM OVARIES OVIDUCT (UTERINE TUBES) UTERUS VAGINA Female Reproductive Organs • Ovary: female gonad • Uterine Tubes (fallopian tube, oviduct) - three parts: infundibulum, ampulla, isthmus The Female Reproductive System in Midsagital View Figure 28.13 The Ovaries and Their Relationships to the Uterine Tube and Uterus Figure 28.14a, b The Uterine Tubes Figure 28.17a-c The Uterus • Muscular organ – Mechanical protection – Nutritional support – Waste removal for the developing embryo and fetus • Supported by the broad ligament and 3 pairs of suspensory ligaments Uterine Wall Consists of 3 Layers: • Myometrium – outer muscular layer • Endometrium – a thin, inner, glandular mucosa • Perimetrium – an incomplete serosa continuous with the peritoneum • The site of implantation of developing embryo • And 3 parts: fundus, body, and cervix Female Accessory Sex Organs: Uterus • Uterine endometrium has two layers: - basal layer - functional layer: built up and shed each cycle The Uterus Figure 28.18a, b The Uterus Figure 28.18c The Uterine Wall Figure 28.19a The Uterine Wall Figure 28.19b The Uterine Cycle To be discussed below Figure 28.20 Functions of the Ovary • Production of a mature oocyte, capable of fertilization and embryonic development. • Production of ovarian steroids (estradiol, progesterone). • Production of gonadal peptides (inhibin, activin). Structural Organization of the Ovary • The main functional unit of the ovary is the follicle. • Follicles are composed of the oocyte, granulosa cells, and theca cells. Stages of Follicular Growth • Follicles are present in a number of different stages of growth: - primordial follicles (resting) - primary, secondary, and antral follicles - preovulatory (Graafian) follicles The Corpus Luteum • After the preovulatory follicle ovulates (releases its egg), it forms the corpus luteum. FEMALE REPRODUCTIVE SYSTEM OVIDUCT (UTERINE TUBES) INFUNDIBULUM, AMPULLA, ISTHMUS, UTERINE UTERUS FUNDUS, BODY (CORPUS), CERVIX Oogenesis and Oocyte Maturation • Recall that germ cells must go through meiosis in order to produce unique haploid cells. • From one spermatogonia, end up with four spermatozoa. • Oocytes must also go through meiosis, but they do it during the course of follicular development. • Primordial follicles contain primary oocytes that are arrested in prophase I, prior to the first meiotic division (diploid). • How do they go through the rest of meiosis? Oocyte Maturation • Oocytes remain in prophase I until the preovulatory surge of LH, which initiates completion of the first meiotic division. • The primary oocyte does not split into two cells, but instead gives off a very small first polar body, containing half of the chromosomes. LH surge zona pellucida first polar body Oocyte Maturation • Thus, the ovulated “egg” is actually not completely mature (hasn’t completed meiosis II). • Maturation goes to completion only if the oocyte is fertilized. • Fertilization causes completion of meiosis II, and expulsion of a second polar body. • Meiosis of the oocyte results in only one gamete. fertilization first polar body first polar body second polar body FEMALE REPRODUCTIVE SYSTEM OVARY GERMINAL EPITHELIUM TUNICA ALBUGINEA - thin connective tissue capsule underlying germinal epithelium CORTEX - surrounds the medulla and contains maturing follicles MEDULLA - central connective tissue containing vascular supply and nervous innervation The Ovarian Cycle FEMALE REPRODUCTIVE SYSTEM OVARY The Ovarian Cycle 3 to 5 million OOGONIA differentiate into PRIMARY OOCYTES during early development OOCYTES becomes surrounded by squamous (follicular) cells to become PRIMORDIAL FOLLICLES most PRIMORDIAL FOLLICLES undergo atresia leaving 400,000 at birth oocytes at birth arrested at Meiosis I (prophase) FEMALE REPRODUCTIVE SYSTEM OVARY THREE STAGES OF OVARIAN FOLLICLES CAN BE IDENTIFIED FOLLOWING PUBERTY: (each follicle contains one oocyte) (1) PRIMORDIAL FOLLICLES OOGENESIS - very prevalent; located in the periphery of the cortex - a single layer of squamous follicular cells surround the oocyte (2) GROWING FOLLICLES - three recognizable stages: (a) early primary follicle (b) late primary follicle (c) secondary (antral) follicle (3) MATURE (GRAAFIAN) FOLLICLES - follicle reaches maximum size FEMALE REPRODUCTIVE SYSTEM OVARIAN FOLLICLES (1) PRIMORDIAL FOLLICLES (2) GROWING FOLLICLES (a) early primary follicle - follicular cells still unilaminar but now are cuboidal in appearance - oocyte begins to enlarge (b) late primary follicle - multilaminar follicular layer; cells now termed granulosa cells - zona pellucida appears; gel-like substance rich in GAGs - surrounding stromal cells differentiate into theca interna and theca externa (b) secondary (antral) follicle - cavities appear between granulosa cells forming an antrum - follicle continues to grow - formation of cumulus oophorus and corona radiata (3) MATURE (GRAAFIAN) FOLLICLES FEMALE REPRODUCTIVE SYSTEM OVARIAN FOLLICLES late primary follicle FEMALE REPRODUCTIVE SYSTEM OVARIAN FOLLICLES GRANULOSA (FOLLICULAR) CELLS OOCYTE ZONA PELLUCIDA FEMALE REPRODUCTIVE SYSTEM OVARY CORTEX MEDULLA CORPUS LUTEUM FEMALE REPRODUCTIVE SYSTEM TUNICA ALBUGINEA GERMINAL EPITHELIUM CORTEX OVARY PRIMORDIAL FOLLICLES TUNICA ALBUGINEA GERMINAL EPITHELIUM FEMALE REPRODUCTIVE SYSTEM OVARY FEMALE REPRODUCTIVE SYSTEM OVARY OVARY H&E PRIMORDIAL FOLLICLES EARLY 1º FEMALE REPRODUCTIVE SYSTEM OVARY OVARY H&E CORPUS ALBICANS EARLY PRIMARY FOLLICLES PRIMORDIAL FOLLICLE FEMALE REPRODUCTIVE SYSTEM OVARY LATE PRIMARY FOLLICLE multilaminar FEMALE REPRODUCTIVE SYSTEM OVARY MATURE (GRAAFIAN) FOLLICLE zona pellucida cumulus oophorus corona radiata theca interna and externa theca interna cells begin to produce androgens that are converted to estrogens FEMALE REPRODUCTIVE SYSTEM HORMONAL REGULATION OF OOGENSIS AND OVULATION HYPOTHALAMUS release of GnRF which stimulates release of LH and FSH from the adenohypophysis (ANTERIOR PITUITARY) Neuroendocrine Regulation of Ovarian Functions CNS hypothalamus GnRH Pituitary FSH LH E2, P inhibin, activin OVARY Follicle Development Ovulation Luteinization Effects of GnRH on Gonadotropins • GnRH is released in a pulsatile manner, stimulating the synthesis and release of LH and FSH. • GnRH acts through its receptor on the pituitary gonadotroph cells, stimulating production of phospholipase C. • Recall that IP3 pathway causes gonadotropin release, while the DAG/PKC pathway causes gonadotropin synthesis. Actions of FSH on Granulosa Cells FSH AC ATP cAMP Gs Gene Expression Steroidogenic enzymes PKA LH Receptor CREB CRE Inhibin Subunits Plasminogen Regulation of Estradiol Production • Recall the two-cell theory of estradiol production (lecture 4): - LH acts on theca cells to produce androgens - FSH acts on granulosa cells to increase aromatase activity, resulting in conversion of androgens to estrogens (granulosa cells lack 17 hydroxylase activity) Ovarian Estradiol Production LH Theca cells androgens aromatase Granulosa cells FSH estradiol Regulation of Progesterone Production • Progesterone is produced from theca cells, mature granulosa cells, and from the corpus luteum. • In this case, gonadotropins induce expression of - steroidogenic acute regulatory protein - P450 side chain cleavage Actions of Estradiol • Estradiol plays an important role in feedback regulation of gonadotropin release. • Low estradiol levels exert negative feedback (via inhibition of GnRH release) Question: what happens to LH and FSH levels if you remove the ovary (increase, decrease, no change)? Answer: Actions of Estradiol • High estradiol levels exert positive feedback (via increase in GnRH receptors, stimulation of GnRH release, increased pituitary response to GnRH, and effects on LH) - increase in stimulatory neurotransmitters regulating GnRH neurons (ie, norepinephrine) - decrease in inhibitory neurotransmitters (ie, beta endorphin) - increased activity of GnRH neurons - increased expression of GnRH receptors - increased expression of LH gene Actions of Estradiol • Estradiol also has important actions in a number of other tissues: - causes proliferation of uterine endometrium - increases contractility of uterine myometrium - stimulates development of mammary glands - stimulates follicle growth (granulosa cell proliferation) - effects on bone metabolism, hepatic lipoprotein production, genitourinary tract, mood, and cognition • Effects are mediated through the intracellular estrogen receptors (alpha and beta), and possible membrane effects. Actions of Progesterone • Progesterone exerts positive and negative feedback effects on gonadotropin synthesis and release. • Progesterone also acts on many tissues: - stimulates secretory activity of the uterine endometrium - inhibits contractility of the uterine myometrium - stimulates mammary growth • The actions of progesterone are mediated through an intracellular P receptor, which acts as a transcription factor. Regulation of Follicle Growth • Primordial follicles can “rest” for many decades before being recruited for growth by an unknown mechanism. • The recruitment of primordial follicles and subsequent growth to the small antral follicle stage can occur without gonadotropin stimulation (gonadotropin-independent). • Small antral follicles (and larger) must be stimulated by FSH and LH in order to continue growth to the preovulatory stage (gonadotropin dependent). Regulation of Follicle Growth • Each day many follicles begin to grow (recruitment). • Each cycle, only one follicle is “selected” for continued development to the preovulatory stage, by an unknown mechanism. • This follicle is called the dominant follicle • The remaining recruited follicles become atretic and degenerate. Regulation of Follicle Growth recruitment selection preovulatory follicle atresia Follicular Ovulation • As the preovulatory follicle grows, it produces increasing amounts of estradiol. • When the preovulatory follicle is mature, plasma estradiol levels are very high. • High estradiol levels exert positive feedback on the hypothalamus and pituitary, resulting in LH and FSH surges. • These preovulatory gonadotropin surges cause ovulation of the preovulatory follicle (follicular rupture and release of the egg for fertilization). Mechanism of Gonadotropin-induced Ovulation • The preovulatory LH and FSH surges induce expression of enzymes in the preovulatory follicle which break down the follicle wall. • Tissue-type plasminogen activator: results in breakdown of fibrin. • Metalloproteinases: result in breakdown of collagen. • Result: follicle wall is ruptured, resulting in release of the oocyte into the peritoneal cavity. Formation of the Corpus Luteum • After the follicle ovulates, the remaining granulosa cells and theca cells luteinize. • Luteinization: accumulation of cholesterol and lipid, cells swell. • Luteinized cells switch the ovary from predominant production of estradiol to production of progesterone and estradiol. • This prepares the uterine endometrium for pregnancy. FEMALE REPRODUCTIVE SYSTEM The Menstrual Cycle HORMONAL REGULATION OF OOGENSIS AND OVULATION FOLLICULAR PHASE OVULATION LUTEAL PHASE 10-20 primordial follicles begin to develop in response to FSH and LH levels theca and granulosa cells transform into the corpus luteum and secrete large amounts of progesterone FSH and LH stimulate theca and granulosa production of estrogen and progesterone if fertilization does not occur, corpus luteum degenerates ... if fertilization does occur, HCG released from the embryo maintains corpus luteum surge of LH induces ovulation FEMALE REPRODUCTIVE SYSTEM The Menstrual Cycle HORMONAL REGULATION OF OOGENSIS AND OVULATION OVULATION: sharp surge in LH with simulataneous increase in FSH Meiosis I resumes; oocyte and surrounding cumulus break away and are extruded oocyte passes into oviduct ECTOPIC IMPLANTATIONS The Menstrual Cycle • Women have ovulatory cycles of about 28 days in length. • Day 1 of the cycle is defined as the first day of menstruation. • There are two phases of the cycle, named after ovarian and uterine function during that phase: - first two weeks: follicular or proliferative stage - second two weeks: luteal or secretory stage • The preovulatory gonadotropin surges occur in the middle of the cycle (around day 14). The Menstrual Cycle: The Ovary • Follicular phase: small antral follicles develop, a dominant follicle is selected and grows to the preovulatory stage. • Midcycle: the gonadotropin surges cause ovulation of the dominant follicle. • Luteal phase: the corpus luteum forms and becomes functional, secreting large amounts of progesterone, followed by estradiol (results in negative feedback, not positive feedback, because P increases before E2). • If pregnancy does not take place, the corpus luteum regresses, and P and E2 levels decrease. The Menstrual Cycle: The Uterus • Proliferative stage: increasing estradiol levels stimulate proliferation of the functional layer of the uterine endometrium. - Results in increased thickness of the endometrium. - Increased growth of uterine glands (secrete mucus) and uterine arteries. • Secretory stage: progesterone acts on the endometrium. - uterine glands become coiled and secrete more mucus - uterine arteries become coiled (spiral arteries) The Menstrual Cycle: The Uterus • If pregnancy doesn’t occur, P and E2 levels decrease at the end of the secretory stage. - vasospasm of arteries causes necrosis of tissue - loss of functional layer with bleeding of uterine arteries (menstruation) FEMALE REPRODUCTIVE SYSTEM CORPUS LUTEUM FORMED FROM FOLLICLE WALL WHICH REMAINS FOLLOWING OVULATION TRANSFORMED CELLS SECRETE ESTROGENS AND PROGESTERONE: (1) GRANULOSA LUTEIN CELLS - large, light cells derived from granulosa cells (2) THECA LUTEIN CELLS - strands of small cells derived from theca interna FEMALE REPRODUCTIVE SYSTEM CORPUS LUTEUM (1) GRANULOSA LUTEIN CELLS CORPUS LUTEUM H&E (2) THECA LUTEIN CELLS (1) (2) FEMALE REPRODUCTIVE SYSTEM OVIDUCT TRANSMITS OVA FROM OVARY TO UTERUS MEIOSIS II IN PROGRESS AND ULTIMATELY ARRESTS UNLESS FERTILIZED SITE OF FERTILIZATION MUCOSA EPITHELIUM AND LAMINA PROPRIA MUSCULARIS INNER CIRCULAR; OUTER LONGITUDINAL INCREASES AS APPROACH UTERUS SEROSA FEMALE REPRODUCTIVE SYSTEM OVIDUCT SIMPLE COLUMNAR EPITHELIUM TWO CELL TYPES: (1) CILIATED (2) PEG CELLS (NONCILIATED) FEMALE REPRODUCTIVE SYSTEM UTERUS PERIMETRIUM, MYOMETRIUM, ENDOMETRIUM FEMALE REPRODUCTIVE SYSTEM UTERUS ENDOMETRIUM undergoes cyclic changes which prepare it for implantation of a fertilized ovum TWO LAYERS: (1) FUNCTIONAL LAYER (stratum functionalis) - BORDERS UTERINE LUMEN - SLOUGHED OFF AT MENSTRATION - CONTAINS UTERINE GLANDS (2) BASAL LAYER (stratum basale) - RETAINED AT MENSTRATION - SOURCE OF CELLS FOR REGENERATION OF FUNCTIONAL LAYER STRAIGHT AND SPIRAL ARTERIES FEMALE REPRODUCTIVE SYSTEM HORMONAL REGULATION OF UTERINE CYCLE (1) PROLIFERATIVE PHASE concurrent with follicular maturation and influenced by estrogens (2) SECRETORY PHASE concurrent with luteal phase and influenced by progesterone (3) MENSTRUAL PHASE commences as hormone production by corpus luteum declines FEMALE REPRODUCTIVE SYSTEM UTERUS PROLIFERATIVE PHASE cells in basal layer begin to proliferate to regenerate functional layer spiral arteries begin to lengthen and revascularize developing layer functional layer becomes thicker than basal layer during late proliferative phase developing uterine glands are tubular in arrangement FEMALE REPRODUCTIVE SYSTEM UTERUS PROLIFERATIVE PHASE tubular uterine glands simple columnar lining FEMALE REPRODUCTIVE SYSTEM UTERUS PROLIFERATIVE PHASE tubular uterine glands UTERUS H&E PROLIFERATIVE PHASE simple columnar lining UTERINE GLANDS FEMALE REPRODUCTIVE SYSTEM UTERUS SECRETORY PHASE functional layer thickens glands become coiled and accumulate large quantities of secretory product FEMALE REPRODUCTIVE SYSTEM UTERUS SECRETORY PHASE UTERUS H&E SECRETORY PHASE functional layer thickens glands coiled COILED UTERINE GLANDS FEMALE REPRODUCTIVE SYSTEM UTERUS SECRETORY PHASE functional layer thickens glands become coiled and accumulate large quantities of secretory product FEMALE REPRODUCTIVE SYSTEM VAGINA MUCOSA STRATIFIED SQUAMOUS EPITHELIUM LAMINA PROPRIA ---------------- no glands ---------------MUSCULARIS INNER CIRCULAR OUTER LONGITUDINAL ADVENTITIA FEMALE REPRODUCTIVE SYSTEM LABIA MINORUM LABIA MINORUM H&E Endocrinology of Pregnancy • To maintain the uterine endometrium and inhibit contraction of myometrium, must maintain plasma progesterone levels during pregnancy. • Early in pregnancy, this is accomplished by the action of human chorionic gonadotropin (hCG) on the corpus luteum (first 8 weeks of pregnancy). • Later in pregnancy, progesterone is produced by the placenta. Early Embryonic Development • After fertilization, the embryo spends the first four days in the oviduct (fallopian tube). • The developing embryo then goes to the uterus, and implants in the uterine endometrium on Day 6 (blastocyst stage of development). • By day 6, the trophoblast cells of the embryo begin to produce hCG. • In a normally developing embryo, hCG levels (in maternal circulation) will double every 3 days, reaching peak at about 2 months of pregnancy. Actions of Human Chorionnic Gonadotropin (hCG) • hCG binds to the LH receptor in the corpus luteum, maintaining luteal steroidogenesis during the first 8 weeks of pregnancy. • In addition, hCG may act to stimulate testosterone production from the developing testes in male embryos. Role of the Fetal-Placental-Maternal Unit in Steroid Production • Later in pregnancy, the placenta becomes the major steroidogenic organ of pregnancy. • However, the placenta requires maternal LDL as a source of cholesterol for progesterone production. • The placenta also produces estrogens during pregnancy (primarily estriol). However, the placenta is dependent upon the maternal and fetal adrenal as a source of androgens for aromatization to estrogen. • Estrogens may be important in increasing uterine blood flow to the fetus, and in the maturation of fetal organ systems. Parturition: The Process of Childbirth • The mechanisms signaling the onset of labor are not clearly understood, although several theories exist. • Potential role of progesterone?: - decreasing progesterone prior to labor would allow uterine contractions to occur - however, there is no decline in progesterone before labor in humans - some studies suggest there is a decline in uterine progesterone receptors, resulting in decreased progesterone action, leading to labor Potential Role of Oxytocin in Parturition? • Oxytocin causes uterine contraction. • However, oxytocin levels do not increase until after labor starts, according to more recent studies. • Oxytocin may play a role in uterine contraction following labor, resulting in decreased blood loss. Potential Role of Relaxin in Parturition? • Relaxin acts on the cervix, causing dilatation and softening. • In some animals relaxin increases before labor starts. • In humans, relaxin is high beginning early in pregnancy and stays elevated until labor. • Relaxin does act to soften connective tissues, such as the ligaments connecting the pelvic bones, to allow increase in size of the birth canal. • Relaxin also decreases uterine contractility during pregnancy. Potential Role of Prostaglandins in Parturition • Prostaglandins cause dilation and softening of the cervix. • Prostaglandins also cause uterine contractions. • The levels of prostaglandins increase in fetal membranes before the onset of labor. • It is believed that some (unknown) signal from the fetus causes increased prostaglandin production from fetal membranes, which then act on the uterus and cervix to initiate labor. Lactation • Lactation is the delivery of milk from the mammary gland. • There are four main stages of lactation, controlled by different hormones: - milk synthesis in alveolar cells - secretion of milk from alveolar cells to alveolar lumen - maintainance of established milk production and release into alveolar lumen - milk ejection: movement of milk from alveoli into the duct system and out of the breast Lactation: Milk Synthesis • Milk Synthesis: Production of breast milk is stimulated by increased levels of prolactin (pituitary) and human placental lactogen (from the placenta) during pregnancy. • Milk release from alveolar cells is inhibited by the high levels of progesterone and estrogen during pregnancy. • Estrogen and progesterone also act with prolactin to increase alveolar duct growth during pregnancy. Lactation: Lactogenesis • Lactogenesis: secretion of milk from alveolar cells into the alveoli of the breast. • Stimulated by prolactin, and occurs after parturition when estradiol and progesterone levels are decreased. Lactation: Galactopoiesis and Milk Ejection • Galactopoiesis: the maintenance of established milk production, caused by prolactin. • Milk Ejection: movement of milk from alveolar ducts into the main duct system and out of the breast. Induced by oxytocin. Oxytocin causes contraction of myoepithelial cells in the breast, causing milk release. Regulation of Oxytocin and Prolactin During Lactation • There is a positive feedback effect of breastfeeding on the production of oxytocin and prolactin. • Oxytocin levels increase due to suckling of the breast by the infant. In addition, sight, sound, or thought of the infant can also increase oxytocin levels, causing milk ejection. • Prolactin release is also increased by suckling of the breast by the infant (but not by audiovisual stimuli). Associated with suppression of dopamine release. Hormonal Induction of Labor Estrogen From ovaries Induces oxytocin receptors on uterus Baby in utero Oxytocin (+) From fetus and mother’s post pit Positive feedbac k Stim uterus to contract Stim placenta to make PGs (+) Stim more vigorous contractions of uterus Physical/emotional stress (+) Milk Letdown Reflex Suckling stim pressure receptors, which lead to efferents to mother’s hypothalamus (+) Feedback cycle continues till suckling stops. Hypo Pit oxytocin stim breast myoepithelial cells to contract Alveolar glands respond by releasing milk