DRUGS OF ABUSE
advertisement
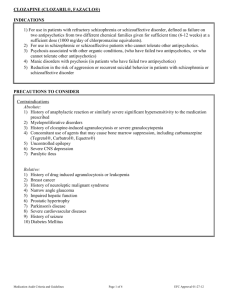
DRUG TREATMENT OF PSYCHOSIS Psychosis Psychosis is a thought disorder characterized by disturbances of reality and perception, impaired cognitive functioning, and inappropriate or diminished affect (mood). Psychosis denotes many mental disorders. Schizophrenia is a particular kind of psychosis characterized mainly by a clear sensorium but a marked thinking disturbance. Psychosis-Producing Drugs 1) Levodopa 2) CNS stimulants a) Cocaine b) Amphetamines c) Khat, cathinone, methcathinone 3) Apomorphine 4) Phencyclidine Schizophrenia • Pathogenesis is unknown. • Onset of schizophrenia is in the late teens early ‘20s. • Genetic predisposition -- Familial incidence. • Multiple genes are involved. • Afflicts 1% of the population worldwide. • May or may not be present with anatomical changes. Schizophrenia • A thought disorder. • The disorder is characterized by a divorcement from reality in the mind of the person (psychosis). • It may involve visual and auditory hallucinations, delusions, intense suspicion, feelings of persecution or control by external forces (paranoia), depersonalization, and there is attachment of excessive personal significance to daily events, called “ideas of reference”. Schizophrenia Positive Symptoms. Hallucinations, delusions, paranoia, ideas of reference. Negative Symptoms. Apathy, social withdrawal, anhedonia, emotional blunting, cognitive deficits, extreme inattentiveness or lack of motivation to interact with the environment. These symptoms are progressive and non-responsive to medication. Etiology of Schizophrenia Idiopathic Biological Correlates 1) Genetic Factors 2) Neurodevelopmental abnormalities. 3) Environmental stressors. Etiology of Schizophrenia Characterized by several structural and functional abnormalities in the brains of schizophrenic patients: 1) Enlarge cerebral ventricles. 2) Atrophy of cortical layers. 3) Reduced volume of the basal ganglia. Dopamine Theory of Schizophrenia Many lines of evidence point to the aberrant increased activity of the dopaminergic system as being critical in the symptomatology of schizophrenia. There is a greater occupancy of D2 receptors by dopamine => greater dopaminergic stimulation Dopamine Theory of Schizophrenia Dopamine Correlates: • Antipsychotics reduce dopamine synaptic activity. • These drugs produce Parkinson-like symptoms. • Drugs that increase DA in the limbic system cause psychosis. • Drugs that reduce DA in the limbic system (postsynaptic D2 antagonists) reduce psychosis. • Increased DA receptor density (Post-mortem, PET). • Changes in amount of homovanillic acid (HVA), a DA metabolite, in plasma, urine, and CSF. Pharmacodynamics Anatomic Correlates of Schizophrenia... Areas Associated with Mood and Thought Processes: Frontal cortex Amygdala Hippocampus Nucleus accumbens Limbic Cortex Dopamine Theory of Schizophrenia Evidence against the Theory? • Antipsychotics are only partially effective in most (70%) and ineffective for some patients. • Phencyclidine, an NMDA receptor antagonist, produces more schizophrenia-like symptoms in nonschizophrenic subjects than DA agonists. • Atypical antipsychotics have low affinity for D2 receptors. • Focus is broader now and research is geared to produce drugs with less extrapyramidal effects. Dopamine System There are four major pathways for the dopaminergic system in the brain: I. II. III. IV. The Nigro-Stiatal Pathway. The Mesolimbic Pathway. The Mesocortical Pathway. The Tuberoinfundibular Pathway. THE DOPAMINERGIC SYSTEM Catecholamines Tyrosine Tyrosine hydroxylase L-Dopa Dopa decarboxylase Dopamine (DA) Dopamine hydroxylase Norepinephrine (NE) (Noradrenaline) Phenylethanolamine- -N-methyltransferase Epinephrine (EPI) (Adrenaline) Tyrosine Tyrosine L-DOPA DA Dopamine Synapse Dopamine System • DOPAMINE RECEPTORS – There are at least 5 subtypes of receptors: – D1 and D5: mostly involved in postsynaptic inhibition. – D2, D3, and D4: involved in both pre-and postsynaptic inhibition. D2: the predominant subtype in the brain: regulates mood, emotional stability in the limbic system and movement control in the basal ganglia. Dopamine Reuptake System Antipsychotic treatments SCHIZOPHRENIA IS FOR LIFE There is no remission Antipsychotic treatments Schizophrenia has been around perhaps, since the beginning of humankind, however, it was not until the last century that it was established as a separate entity amongst other mental disorders. Many treatments have been devised: Hydrotherapy: “The pouring of cold water in a stream, from a height of at least four feet onto the forehead, is one of the most certain means of subsiding violent, maniacal excitement that we have ever seen tried”... wrote an anonymous physician in the early 1800’s. Antipsychotic treatments Lobotomies (Egaz Moniz). In 1940’s Phenothiazenes were isolated and were used as pre-anesthetic medication, but quickly were adopted by psychiatrists to calm down their mental patients. In 1955, chlorpromazine was developed as an antihistaminic agent by Rhône-Pauline Laboratories in France. In-patients at Mental Hospitals dropped by 1/3. Antipsychotics treatment Antipsychotics/Neuroleptics • • Antipsychotics are the drugs currently used in the prevention of psychosis. They have also been termed neuroleptics, because they suppress motor activity and emotionality. ** These drugs are not a cure ** • Schizophrenics must be treated with medications indefinitely, in as much as the disease in lifelong and it is preferable to prevent the psychotic episodes than to treat them. Antipsychotics/Neuroleptics Although the antipsychotic/neuroleptics are drugs used mainly in the treatment of schizophrenia, they are also used in the treatment of other psychoses associated with depression and manic-depressive illness, and psychosis associated with Alzheimer’s disease. These conditions are life-long and disabling. Antipsychotics/Neuroleptics NON-compliance is the major reason for relapse. Antipsychotic/Neuroleptics OLDER DRUGS Three major groups : 1) Phenothiazines 2) Thioxanthines 3) Butyrophenones Antipsychotics/Neuroleptics Tyrosine Tyrosine Dopamine Synapse L-DOPA DA dopamine receptor antagonist D2 • Old antiphsychotics /neuroleptics are D2 dopamine receptor antagonists. Although they are also effective antagonists at ACh, 5-HT, NE receptors. Antipsychotics/Neuroleptics • It appears that the specific interaction of antipsychotic drugs with D2 receptors is important to their therapeutic action. • The affinities of most older “classical” agents for the D2 receptors correlate with their clinical potencies as antipsychotics. Antipsychotic/Neuroleptics Correlations between therapeutic potency and affinity for binding D2 receptors. promazine chlorpromazine clozapine thiothixene haloperidol spiroperidole Clinical dose of drug [mg d-1] Antipsychotics/Neuroleptics • Both D1 and D2 receptors are found in high concentrations in the striatum and the nucleus accumbens. • Clozapine has a higher affinity for the D4 receptors than for D2. • Recently it has been found that most antipsychotic drugs may also bind D3 receptors (therefore, they are non-selective). Antipsychotics/Neuroleptics • Antipsychotics produce catalepsy (reduce motor activity). – • BLOCKADE OF DOPAMINE RECPTORS IN BASAL GANGLIA. Antipsychotics reverse hyperkinetic behaviors (increased locomotion and stereotyped behavior). – • BLOCKADE OF DOPAMINE RECPTORS IN LIMBIC AREAS. Antipsychotics prevent the dopamine inhibition of prolactin release from pituitary. – BLOCKADE OF DOPAMINE RECEPTORS IN PITUITARY. hyperprolactinemia Pharmacokinetics Absorption and Distribution • Most antipsychotics are readily but incompletely absorbed. • Significant first-pass metabolism. • Bioavailability is 25-65%. • Most are highly lipid soluble. • Most are highly protein bound (92-98%). • High volumes of distribution (>7 L/Kg). • Slow elimination. **Duration of action longer than expected, metabolites are present and relapse occurs, weeks after discontinuation of drug.** Pharmacokinetics Metabolism • Most antipsychotics are almost completely metabolized. • Most have active metabolites, although not important in therapeutic effect, with one exception. The metabolite of thioridazine, mesoridazine, is more potent than the parent compound and accounts for most of the therapeutic effect. Pharmacokinetics Excretion • Antipsychotics are almost completely metabolized and thus, very little is eliminated unchanged. • Elimination half-lives are 10-24 hrs. Antipsychotic/Neuroleptics 1) Phenothiazines • Aliphatic Piperidine Piperazine* Chlorpromazine Thioridazine Fluphenazine Trifluopromazine Piperacetazine Perfenazine Mesoridazine Acetophenazine Carphenazine Prochlorperazine Trifluoperazine * Most likely to cause extrapyramidal effects. Antipsychotic/Neuroleptics Piperazine Piperidine Aliphatic [Drug dose] Antipsychotic/Neuroleptics 2) Thioxanthines Thiothixene Chlorprothixene Closely related to phenothiazines Antipsychotic/Neuroleptics 3) Butyrophenones Haloperidol Droperidol* *Not marketed in the U.S. Antipsychotic/Neuroleptics Butyrophenone Phenothiazine Thioxanthene [Drug dose] Antipsychotics/Neuroleptics • Newer drugs have higher affinities for D1, 5HT or -AR receptors. • NE, GABA, Glycine and Glutamate have also been implicated in schizophrenia. Antipsychotics/Neuroleptics The acute effects of antipsychotics do not explain why their therapeutic effects are not evident until 4-8 weeks of treatment. Blockade of D2 receptors Short term/Compensatory effects: Firing rate and activity of nigrostriatal and mesolimbic DA neurons. DA synthesis, DA metabolism, DA release Antipsychotics/Neuroleptics Presynaptic Effects Blockade of D2 receptors Compensatory Effects Firing rate and activity of nigrostriatal and mesolimbic DA neurons. DA synthesis, DA metabolism, DA release. Postsynaptic Effects Depolarization Blockade Inactivation of nigrostriatal and mesolimbic DA neurons. Receptor Supersensitivity Antipsychotic/Neuroleptics Newer Drugs Pimozide Molindone Loxapine Clozapine Olanzapine Qetiapine Risperidone Sertindole Ziprasidone Olindone Antipsychotic/Neuroleptics Drug ClinicalEx. Py. Potency toxicity Sedation Hypote. Chlorpromaz. Haloperidol Thiothixene Clozapine Ziprasidone Risperidone Olanzapine Sertindole Low High High Medium Medium High High High Medium Very High Medium Very low Very Low Low Very Low Very Low Medium Very High Medium Low Low Low Medium Very low High Low Medium Medium Very low Low Very low Very Low Antipsychotic/Neuroleptics Chlorpromazine: 1 = 5-HT2 = D2 > D1 > M > 2 Haloperidol: D2 > D1 = D4 > 1 > 5-HT2 >H1>M = 2 Clozapine: D4 = 1 > 5-HT2 = M > D2 = D1 = 2 ; H1 Quetiapine: 5-HT2 = D2 = 1 = 2 ; H1 Risperidone: 5-HT2 >> 1 > H1 > D2 > 2 >> D1 Sertindole: 5-HT2 > D2 = 1 Antipsychotic/Neuroleptics Clinical Problems with antipsychotic drugs include: 1) 2) Failure to control negative effect Significant toxicity a) b) c) d) e) 3) Parkinson-like symptoms Tardive Dyskinesia (10-30%) Autonomic effects Endocrine effects Cardiac effects Poor Concentration The Nigro-Striatal Pathway DA neuron Striatum ACh neuron + Substantia Nigra GABA - neuron - Inhibition of Motor Activity - GABA neuron Antipsychotic/Neuroleptics Some antipsychotics have effects at muscarinic acetylcholine receptors: • • • • dry mouth blurred vision urinary retention constipation Clozapine Chlorpromazine Thioridazine Antipsychotic/Neuroleptics Some antipsychotics have effects at adrenergic receptors: • orthostatic hypotension Chlorpromazine Thioridazine Some antipsychotics have effects at H1histaminergic receptors: • sedation Risperidone Haloperidol Antipsychotic/Neuroleptics Blockade of D2 receptors in lactotrophs in breast increase prolactin concentration and may produce breast engorgement and galactorrhea. Antipsychotic/Neuroleptics Neuroleptic Malignant Syndrome Is a rare but serious side effect of neuroleptic (antipsychotic) therapy that can be lethal. It can arise at any time in the course of treatment and shows no predilection for age, duration of treatment, antipsychotic medication, or dose. Antipsychotic/Neuroleptics Neuroleptic Malignant Syndrome • • • • • • Occurs in pts. hypersensitive to the Ex.Py. effects of antipsychotics. Due to excessively rapid blockade of postsynaptic dopamine receptors. The syndrome begins with marked muscle rigidity. If sweating is impaired, a fever may ensue. The stress leukocytosis and high fever associated with this syndrome may be mistaken for an infection. Autonomic instability with altered blood pressure and heart rate is another midbrain manifestation. Creatine kinase isozymes are usually elevated, reflecting muscle damage. Antipsychotic/Neuroleptics Neuroleptic Malignant Syndrome Treatment Vigorous treatment with antiparkinsonian drugs is recommended as soon as possible. Muscle relaxants such as diazepam, dantrolene or bromocriptine may be helpful. Antipsychotic/Neuroleptics Drug Interactions • • • • • Additive effects with sedatives. Additive effects with anticholinergics. Additive effects with antihistaminergics. Additive effects with -AR blocking drugs. Additive effects with drugs with quinidine-like action (thioridazine).