Chemical transmission and drug action in the central nervous
advertisement

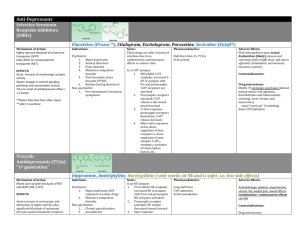
Neurotransmission and drug action in the central nervous system Neuroleptics Anton Kohút 1845 FREUD cocaine from 1933 insulin and electric shocks 1943 Hoffmann LSD 1949 lithium treatment of psychosis 1952 chlorpromazine 1954 meprobamat 1957 benzodiazepine - chlordiazepoxide 1958 iproniazid (inhibítor MAO) imipramin (tricyclic antidepressive drug) Actions of drugs in CNS Nonspecific Anesthetic gases and vapors, The aliphatic alcohols, Some hypnoticsedative drugs. Specific Act on specific receptors in CNS Neurotransmiters in CNS Fast (ligand gated ion Inhibitory: GABA Excitatory: NMDA (glutamate) channels) – NMDA, GABA Slow (G-protein coupled receptors Receptors and neurotransmiters in CNS Transmiters Receptors Glutamate NMDA, and non NMDA GABA GABAA,GABAB Glycine Glycin Acetylcholine nicotinic, muscarinic 5-HT HT1a-d 5-HT 2-7 Noradrenaline 1 2 , 1-3 Dopamine D1-5 Cholecystokinin CCKA ,CCKB NO activation of guanylate cyclase Serotoninergic neurotransmission 5-HT-R classification and function in CNS 5HT-R Action Agonist Antagonist 1A, B neuronal inhibition, behavioural effects: sleep, feeding, anxiety, thermoregul. Buspirone, Sertindole Ergotamine Metiotepine 1D vasoconstriction Sumatriptan Ergotamine Metiotepine 2A neuronal excitation LSD Ketanserine Cyproheptadine (increase in the number in suicides) Nefazodone 3 neuronal excitation, vomiting, anxiety -Metyl-5HT Ondanzetrone Granizetrone Tropizetrone 7 not known LSD Ketanserine Cyproheptadine Biogenic monoamine hypothesis Dopamine and Parkinsonism Subunits of GABA receptor GABA receptor – inhibitory Excitotoxicity has been implicated as a pathophysiologic mechanism in many diseases, including neurodegenerative syndromes, stroke and trauma, hyperalgesia, and epilepsy. Although the clinical applications of interrupting excitoxicity remain limited, it is hoped that better understanding of glutamate-induced excitotoxicity will lead to the development of new approaches to treatment of these diseases. Classification of drugs influencing CNS 1. Neuroleptic drugs (D receptors) antipsychotic drugs, antischizophrenic drugs Increase of dopaminergic activity in the brain is the cause of schizoprenia, 2. Antidepressive drugs – antidepressans (NA, 5HT) Depression and bipolar disorders are pervasive mood altering ilnesses affecting energy, sleep, appetite, libido and the ability to function. Depression is due to a decrease of noradrenaline and serotonine, Mania is due to oposite changes, 3. Anxiolytic and sedative - hypnotic drugs (GABA) Unpleasant state of tension, apprehension, or uneasiness. Disorders involving anxiety are the most common mental disturbances. The role of GABA receptors, Agonists of GABA receptors – benzodiazepines a effecive in the treatment of anxiety. 4. Psychomimetics -psychomotor stimulants (NA, D) 5. Psychotomimetic drugs – halucinogenes (5-HT) 6. Antiepileptics, antiparkinsonics -used to treat Parkinsonism and epilepsy (GABA, NMDA) Neuroleptics (antipsychotics) Chlorpromazine The spliting of the mind Antipsychotic drugs - neuroleptics - are the best treatment now available. They do not cure schizophrenia but they have greatly improved the outlook for individual patients. reduce the psychotic symptoms of schizophrenia, such as hallucinations and delusions, and usually allow the patient to function more effectively and appropriately. patients vary a great deal in the amount of drug needed to reduce symptoms without producing troublesome side effects. Dopaminergic bases of schisophrenia and mechanism of action of neuroleptics Schizophrenia in man is associated with dopaminergic hyperactivity (D2). - number of D2 receptors increase twoo-fold in schizophrenic patients - amphetamine, which release dopamine in brain, can produce in man syndrome similar as the symptoms of schizophrenia - all the neuroleptic drugs block dopamine receptor (brain, periphery) - there are at least twoo types of receptor: D1 and D2 - clinical efficacy correlates closely with relative ability to block D2 receptors Classification of neuroleptics I. Typical neuroleptics Phenothiazines 1. with aliphatic ring: chlorpromazine, levopromazine 2. with piperidine ring: thioridazine 3. with piperazine ring: prochlorperazine, perhenazine (510 x more active as CHPR, antiemetic action), trifluoperazine, flufenazín Thioxantines: chlorprothixen,flupentixol, Butyrophenones: haloperidol, droperidol, II. atypical neuroleptics Dibenzodiazepines- : clozapine, olanzepine, quetapine, ziprasidone, and risperidone - block D1, 4 a 5-HT2 ??? – Site of chlorpromazine action Actions of chlorpromazine antipsychotic actions: - reduction of hallucinations, - reduction of spontaneous physical movement - they do not depress intelectual function of the patient - antipsychotic effect usually take several veeks to occur extrapyramidal effects: parkinsonian symptoms, diskynesia antiemetic effects: block of D2 receptors of the chemoreceptor triger zone of the medulla antimuscarinic effects:- atropine like effect blockade of alfa-adrenoreceptor: orthostatic hypotension hypothermia: neuroleptics alter temperature-regulating mechanisms (poikilothermia) endocrine effect: - increase in prolactin release Atypical neuroleptics have a relatively low affinity for D2 receptor are more effective than typical antipsychotics at treating the “negative” symptoms of schizophrenia, some atypical antipsychotics also act as antagonists at 5-HT2 and D4 receptors Therapeutic uses and side effects Therapeutic uses Side effects treatment of schizophrenia: prevention of severe nausea and vomiting other: - neuroleptanalgesia (droperidol) - chronic pain (+ opioids) parkinsonian effects: CNS depresion: drowsiness occurrs during the firs twoo weeks of therapy antimuscarinic effects endocrinne depression of the hypothalamus > galactorhea, infertility, impotence