Endocrine-Nursing - Unsri

Endocrine-Nursing
dear d34r123@yahoo.co.id
KOMUNITAS BLOGGER UNIVERSITAS SRIWIJAYA
ENDOCRINE SYSTEM The ANATOMY of the Endocrine System The endocrine system is composed of ductless glands that release their hormones directly into the bloodstream The
Hypothalamus controls most of the endocrinal activity of the pituitary gland The pituitary gland controls most of the activities of the other endocrine glands The Hypothalamus This part of the DIENCEPHALON is located below the thalamus and is connected to the pituitary gland by a stalk The PHYSIOLOGY of the Endocrine System: Hypothalamus Secretes
RELEASING HORMONES for the pituitary gland Secretes OXYTOCIN that is stored in the
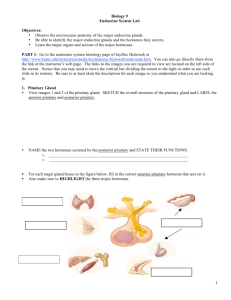
Posterior pituitary gland Secretes Anti-Diuretic Hormone or VASOPRESSIN that is stored also in the posterior pituitary gland The Pituitary Gland Is a gland located below the hypothalamus at the base of the brain The optic chiasm passes over this structure Is divided into two parts- the anterior or adenohypophysis and the posterior or the neurohypophysis
Anterior Pituitary secretes the following hormones: 1. Growth hormone 2. Prolactin 3.
Gonadotrophins- LH and FSH 4. Stimulating hormones and trophic hormones ACTH TSH
MS Posterior Pituitary stores and releases 1. OXYTOCIN 2. ADH/Vasopressin The
THYROID gland Located in the anterior neck lateral to the trachea Contains two lobes connected by the isthmus Microscopically composed of thyroid follicles where the hormones are produced and stored The PHYSIOLOGY of the Endocrine System: Thyroid Produces the thyroid hormones by the thyroid follicles: 1. Tri-iodothyronine or T3 2. Tetra-iodothyronine or thyroxine or T4 The Parafollicular cells secrete CALCITONIN The PARAthyroid glands
Located at the back of the thyroid glands Four in number Secretes PARATHYROID hormone
(PTH) that controls calcium and phosphorus levels The ANATOMY of the Endocrine System
The Adrenal Glands Located above the kidneys Composed of two parts- the outer Adrenal
Cortex and the inner Adrenal medulla Adrenal Cortex Secretes three types of STERIOD hormones 1. Glucocorticoids- like Cortisol, cortisone and corticosterone 2.
Mineralocorticoids- like Aldosterone 3. Sex hormones- like estrogen and testosterone
Adrenal Medulla Essentially a part of the SYMPATHETIC autonomic system Secretes
Adrenergic Hormones: 1. Epinephrine 2. Nor-epinephrine The Pancreas This retroperitoneal organ has both endocrine and exocrine functions The endocrine function resides in the
ISLETS of Langerhans The islets have three types of cells- alpha, beta and delta cells The
ALPHA cells secrete GLUCAGON The BETA cells secrete INSULIN The DELTA cells secrete SOMATOSTATIN The GONADS- Ovaries These two almond-shaped glands are found in the pelvic cavity attached to the uterus by the ovarian ligament The GONADS-
Testes These two oval-shaped glands are found in the scrotum Gonads The Ovaries contains Granulosa and Theca cells which secrete ESTROGEN and Progesterone The testes contains Leydig cells that secrete Testosterone COMMON LABORATORY
PROCEDURES Hormone Levels Assay These are blood examinations fro the levels of individual hormones Measurements can also be done after stimulation and suppression of the secretions- Stimulation and Suppression tests Hormone Levels of T3/T4 Usually done to diagnose hypo/hyperthryroidism If T3 is elevated, T4 is elevated and TSH is depressed-
Primary HYPERthyroidism If T3 is depressed,T4 is depressed and TSH is elevated- Primary
HYPOthyoidism Radio-Active iodine uptake (RAI) This is a thyroid function test to measure the absorption of the injected iodine isotope by the thyroid tissue Increased uptake may indicate HYPERfunctioning gland Decreased uptake my indicate HYPOfunctioning gland
Thyroid Scan Performed to identify nodules or growth in the thyroid gland RAI is used
Pretest- Check for pregnancy, Thyroid medication may be withheld temporarily. NPO, Posttest- Ensure proper disposal of body wastes FASTING BLOOD GLUCOSE Aids in the diagnosis of Diabetes Pre-test; NPO for 8 hours Normal FBS- 80-109 mg/dL GLUCOSE tolerance test Aids in the diagnosis of DM Pre-test: Provide high-carbohydrate foods x 3 days, instruct to avoid caffeine, alcohol and smoking, NPO 10 hours prior to test Post-test: avoid strenuous activity for 8 hours Normal OGTT Glycosylated Hemoglobin A 1-C Blood glucose bound to RBC hemoglobin Reflects how well blood glucose is controlled for the past
3 months FASTING is NOT required! Normal level- expressed as percentage of total hemoglobin N- 4-7% Good control- 7.5%or less Fair control- 7.5 % to 8.9% Poor control- 9% and above DISORDERS OF THE ENDOCRINE GLAND Disorders are generally grouped into: 1. HYPER- when the gland secretes excessive hormones 2. HYPO- when the gland does not secrete enough hormones Hyper and Hypo can be classified as PRIMARY when the Gland itself is the problem or SECONDARY when the pituitary or the hypothalamus is causing the problem HYPOPITUITARISM Hyposecretion of the anterior pituitary gland
CAUSES: Congenital, Post-partal necrosis, infection and tumor PATHOPHYSIOLOGY:
Depends on the major hormone/s depleted ASSESSMENT Findings 1. Retarded physical growth due to decreased GH- dwarfism 2. Low intellectual development 3. poor development of secondary sexual characterisitcs NURSING INTERVENTIONS 1. provide emotional support to the family 2. encourage client and family to express feelings 3. administer prescribed hormonal replacement therapy HYPERPITUITARISM The hypersecretion of the gland also called ACROMEGALY/GIGANTISM CAUSES: tumor, congenital
PATHOPHYSIOLOGY Depends on the hormone/s that is/are increased ASSESSMENT
FINDINGS 1. Increased growth- Gigantism or Acromegaly 2. large and thick hands and feet
3. Visual disturbances 4. Hypertension, hyperglycemia 5. Organomegaly NURSING
INTERVENTION 1. provide emotional support to clients and family 2. provide frequent skin care 3. prepare patient for surgery- removal of pituitary gland NURSING INTERVENTIONS
Post-operative care 1. Monitor VS, LOC and neurologic status 2. Place patient on Semi-
Fowler’s 3. Monitor for Increased ICP, bleeding, CSF leakage 4. instruct patient to
AVOID sneezing, coughing and nose-blowing 5. Monitor development of DI- measure I and
O 6. Administer prescribed medications- antibiotics, analgesics and steroids DIABETES
INSIPIDUS A hyposecretion of ADH CAUSES: Conditions that increase ICP, Surgical removal of post pit, tumor PATHOPHYSIOLOGY Decreased ADH- failure of tubular reabsorption of water- increased urine volume ASSESSMENT findings 1. Polyuria of more than 4 liters of urine/day 2. Polydipsia 3. Signs of Dehydration 4. Muscle pain and weakness
5. Postural hypotension and tachycardia DIAGNOSTIC TEST 1. Urinary Specific gravity- very low, 1.006 or less 2. Serum Sodium levels- high NURSING INTERVENTIONS 1.Monitor
VS, neurologic status and cardiovascular status 2. Monitor Intake and Output 3. Monitor urine specific gravity 4. Provide adequate fluids 5. Administer Chlorpropamide or Clofibrate as prescribed to increase the action of ADH if decreased 6. Administer VASOPRESIN.
Desmopressin or Lypressin. Pitressin is given IM SIADH Hypersecretion of ADH abnormally
CAUSES: tumor, paraneoplastic syndromes PATHOPHYSIOLOGY: Increased ADH- water reabsorption- water intoxication, hypervolemia DIAGNOSTIC TEST 1. urine specific gravity is increased 2. Hyponatremia 3. CBC shows hemodilution ASSESSMENT findings 1. Signs of
Hypervolemia 2. Mental status changes 3. Abnormal weight gain 4. hypertension 5.
Anorexia, Nausea and Vomiting 6. HYPOnatremia NURSING INTERVENTIONS 1. Monitor
VS and neurologic status 2. provide safe environment 3. Restrict fluid intake (less than
500cc/day) 4. Monitor I and O and daily weight 5. Administer Diuretics and IVF carefully 6.
Administer prescribed Demeclocycline to inhibit action of ADH in the kidney DISORDERS OF the ADRENAL GLAND HYPOSECRETION: ADDISON’S DISEASE Decreased secretion of adrenal cortex hormones, especially glucocorticoids and mineralocorticoids
CAUSE: tumor, idopathic PATHOPHYSIOLOGY Decreased Glucocorticoids- decreased resistance to stress Decreased mineralocorticoids- decreased retention of sodium and water
ASSESSMENT Findings for Addison’s disease 1. Weight loss 2. GI disturbances 3.
Muscle weakness, lethargy and fatigue 4. Hyponatremia 5. hyperkalemia 6. hypoglycemia 7. dehydration and hypovolemia 8. Increased skin pigmentation NURSING INTERVENTIONS
1. Monitor VS especially BP 2. Monitor weight and I and O 3. Monitor blood glucose level and
K 4. Administer hormonal agents as prescribed 5. Observe for ADDISONIAN crisis 6.
Educate the client regarding lifelong treatment, avoidance of strenuous activities, stress and seeking prompt consult during illness 7. Provide a high-protein, high carbohydrate and increased sodium intake ADDISONIAN CRISIS A life-threatening disorders caused by acute severe adrenal insufficiency CAUSES: Severe stress, infection, trauma or surgery
PATHOPHYSIOLOGY Overwhelming stimuli- mobilize body defense- decreased stress hormones- inadequate coping ASSESSMENT Findings for Addisonian Crisis 1. Severe headache 2. Severe pain 3. Generalized weakness 4. Severe hypotension 5. Signs of Shock
NURSING INTERVENTIONS 1. Administer IV glucocorticoids, usually hydrocortisone 2.
Monitor VS frequently 3. Monitor I and O, neurological status, electrolyte imbalances and blood glucose 4. Administer IVF 5. Maintain bed rest 6. Administer prescribed antibiotics
HYPERSECRETION: CUSHING’S DISEASE A condition resulting from the hypersecretion of glucocorticoids from the adrenal cortex CAUSES: Pituitary tumor, adrenal tumor, abuse of steroids PATHOPHYSIOLOGY: Increased Glucocorticoids- exaggerated effects of the hormone ASSESSMENT FINDINGS for Cushing 1. generalized muscle weakness and wasting 2. truncal obesity 3. moon-face 4. buffalo hump 5. easy bruisability 6.
Reddish-purplish striae on the abdomen and thighs 7. Hirsutism and acne 8. Hypertension 9. hyperglycemia 10. Osteoporosis 11. Amenorrhea DIAGNOSTIC TEST 1. Serum cortisol level
2. Serum glucose and electrolytes NURSING INTERVENTIONS 1. Monitor I and O , weight and VS 2. Monitor laboratory values- glucose, Na, K and Ca 3. Provide meticulous skin care
4. Administer prescribed medications like aminogluthetimide to inhibit adrenal hyperfunctioning 5. Prepare client for surgical management- pituitary surgery and adrenalectomy 6. protect patient from infection Hypersecretion: CONN’S DISEASE
Hypersecretion of Aldosterone from the adrenal cortex CAUSES: pituitary tumor, adrenal tumor PATHOPHYSIOLOGY: Increased Aldosterone- exaggerated effects ASSESSMENT findings in CONN’S disease 1. Symptoms of HYPOkalemia 2. hypertension 3. hypernatremia 4. Headache, N/V 5. Visual changes 6. Muscles weakness, fatigue and nocturia DIAGNOSTIC TEST 1. Urine gravity- low 2. Serum Sodium- high 3. Serum
Potassium- low 4. Increased urinary Aldosterone NURSING INTERVENTIONS 1. Monitor
VS, I and O and urine sp gravity 2. Monitor serum K and Na 3. Provide Potassium rich foods and supplements 4. Administer prescribed diuretic- Spironolactone 5. Maintain sodiumrestricted diet 6. Prepare patient for possible surgical interventions Hypersecretion:
Pheochromocytoma Increased secretion of epinephrine and nor-epinephrine by the adrenal medulla CAUSE: tumor PATHOPHYSIOLOGY: Increased Adrenergic hormones- exaggerated sympathetic effects ASSESSMENT Findings in Pheochromocytoma 1.
Hypertension 2. Severe headache 3. Palpitations 4. Tachycardia 5. Profuse sweating and
Flushing 6. Weight loss, tremors 7. Hyperglycemia and glycosuria NURSING
INTERVENTIONS 1. Monitor VS especially BP 2. Monitor for HYPERTENSIVE crisis 3.
Avoid stimulation that can cause increased BP 4. Administer Anti-hypertensive agents like alpha-adrenergic blockers- Phenoxybenzamine 5. Prepare Phentolamine for hypertensive crisis 6. Monitor blood glucose and urine glucose 7. promote adequate rest and sleep periods 8. provide HIGH calorie foods and Vitamins/mineral supplements 9. Prepare patient for possible surgery DISORDERS OF the THYROID GLAND HYPOsecretion:
HYPOTHYROIDISM A hypothyroid state characterized by decreased secretions of T3 and
T4 CAUSES: Hypofunctioning tumor, IDG, Pituitary tumor, Ablation therapy, Surgical removal of thyroid PATHOPHYSIOLOGY: Decreased T3 and T4- decreased basal metabolism ASSESSMENT findings for Hypothyroidism 1. Lethargy and fatigue 2. Weakness and paresthesia 3. COLD intolerance 4. Weight gain 5. Bradycardia, constipation 6. Dry hair and skin, loss of body hair 7. Generalized puffiness and edema around the eyes and face 8.
Forgetfulness and memory loss 9. Slowness of movement 10. Menstrual irregularities and cardiac irregularities NURSING INTERVENTIONS 1. Monitor VS especially HR 2. Administer hormone replacement: usually Levothyroxine-should be taken on an empty stomach 3.
Instruct patient to eat LOW calorie, LOW cholesterol and LOW fat diet 4. Manage constipation appropriately 5. Provide a WARM environment 6. Avoid sedatives and narcotics because of increased sensitivity to these medications 7. Instruct patient to report chest pain promptly HYPERfunctioning: HYPERTHYROIDISM Called GRAVE’S DISEASE A hyperthyroid state characterized by increased circulating T3 and T4 CAUSES: Auto-immune disorder, toxic goiter, tumor PATHOPHYSIOLOGY: Increased hormone activity- increased
Basal Metabolism ASSESSMENT Findings for Hyperthyroidism 1. Weight loss 2. HEAT intolerance 3. Hypertension 4. Tachycardia and palpitations 5. Exopthalmos 6. Diarrhea 7.
Warm skin 8. Diaphoresis 9. Smooth and soft skin 10. Fine tremors and nervousness 11.
Irritability, mood swings, personality changes and agitation NURSING INTERVENTIONS 1.
Provide adequate rest periods 2. Administer anti-thyroid medications that block hormone synthesis- Methimazole and PTU 3. Provide a HIGH-calorie diet 4. Manage diarrhea 5. provide a cool and quiet environment 6. Avoid giving stimulants 7. Provide eye care 8.
Administer PROPRANOLOL for tachycardia 9. Administer IODIONE preparation-
Lugol’s solution and SSKI to inhibit the release of T3 and T4 10. Prepare clients for
Radioactive iodine therapy 12. Prepare patient for thyroidectomy 13. Manage thyroid storm appropriately THYROID STORM An acute LIFE-threatening condition characterized by excessive thyroid hormone CAUSE: Manipulation of the thyroid during surgery causing the release of excessive hormones in the blood ASSESSMENT Findings for Thyroid Storm 1.
HIGH fever 2. Tachycardia, Tachypnea 3. Systolic HYPERtension 4. Delirium and coma 5.
Severe vomiting and diarrhea 6. Restlessness, Agitation, confusion and Seizures NURSING
INTERVENTIONS 1. Maintain PATENT airway and adequate ventilation 2. Administer antithyroid medications such as Lugol’s solution, Propranolol, and Glucocorticoids 3.
Monitor VS 4. Monitor Cardiac rhythms 5. Administer PARACETAMOL ( not Aspirin) for
FEVER 6. Manage Seizures as required. Provide a quiet environment THYROIDECTOMY
Removal of the thyroid gland PRE-OPERATIVE CARE - Thyroidectomy 1. Obtain VS and weight 2. Assess for Electrolyte levels, glucose levels and T3/T4 levels 3. Provide preoperative teaching like coughing and deep breathing, early ambulation and support of the neck when moving 4. Administer prescribed medications POST-OPERATIVE CARE -
Thyroidectomy 1. Position patient: Semi-Fowler’s 2. Monitor for respiratory distress- apparatus at bedside- tracheostomy set, O2 tank and suction machine! 3. Check for edema and bleeding by noting the dressing anteriorly and at the back of the neck 4. LIMIT client talking 5. Assess for HOARSENESS 6. Monitor for Laryngeal Nerve damage –
Respiratory distress, Dysphonia, voice changes, Dysphagia and restlessness 7. Monitor for signs of HYPOCALCEMIA and tetany due to trauma of the parathyroid 8. Prepare Calcium gluconate 9. Monitor for thyroid storm DISORDERS OF the PARATHYROID GLAND
Hypofunctioning: HYPOPARATHYROIDISM Hyposecretion of parathyroid hormone
CAUSES: tumor, removal of the gland during thyroid surgery PATHOPHYSIOLOGY:
Decreased PTH- deranged calcium metabolism ASSESSMENT Findings for
HypoParaThyroidism 1. Signs of HYPOCALCEMIA 2. Numbness and tingling sensation on the face 3. Muscle cramps 4. (+) Trosseau’s and Chvostek’s signs 5.
Bronchospasms, laryngospasms, dysphagia 6. Cardiac dysrhythmias 7. Hypotension 8.
Anxiety, irritability ands depression NURSING INTERVENTIONS 1. Monitor VS and signs of
HYPOcalcemia 2. Initiate seizure precautions and management 3. Place a tracheostomy set.
O2 tank and suction at the bedside 4. Prepare CALCIUM gluconate 5. Provide a HIGHcalcium and LOW phosphate diet 6. Advise client to eat Vitamin D rich foods 7. Administer
Phosphate binding drugs Hyperfunctioning: HYPERPARATHYROIDISM Hypersecretion of the gland CAUSE: Tumor PATHOPHYSIOLOGY: Increase PTH- increased CALCIUM levels in the body ASSESSMENT Findings for Hyperparathyroidism 1. Fatigue and muscle weakness/pain 2. Skeletal pain and tenderness 3. Fractures 4. Anorexia/N/V epigastric pain
5. Constipation 6. Hypertension 7. Cardiac Dysrhythmias 8. Renal Stones NURSING
INTERVENTIONS 1. Monitor VS, Cardiac rhythm, I and O 2. Monitor for signs of renal stones, skeletal fractures. Strain all urine. 3. Provide adequate fluids- force fluids 4.
Administer prescribed Furosemide to lower calcium levels 5. Administer NORMAL saline 6.
Administer calcium chelators 7. Administer CALCITONIN 8. Prepare the patient for surgery
DOWNLOAD