MS Diagnostic Coding
advertisement

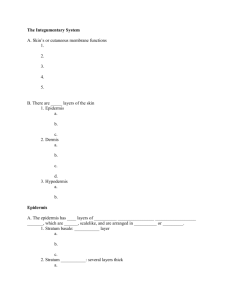
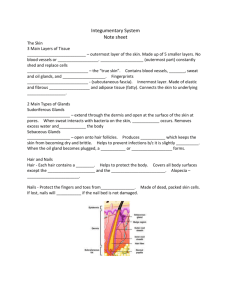
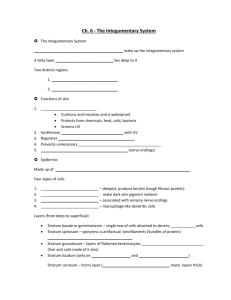
Integumentary Anatomy and Physiology ©Irene Mueller, EdD, RHIA Montana Hospital Association June 6, 2012 http://etc.usf.edu/clipart Objectives • Review Integumentary System Anatomy and Physiology for ICD-10-CM/PCS Coding – Functions of Integumentary System – Layers of Skin – Cells of Integumentary System – Skin Tissues – Nerves – Glands – Hair & Nails – Breast Overview • Integument = Skin L, a covering • Largest Organ of Human Body – Weighs about 8 pounds (3.6 kgs) – Covers 22 sq feet – Contains 11 miles of blood vessels • Worldwide, dead skin accounts for about one billion tons of atmospheric dust • Excretes up to 3 gallons of sweat on hot day Functions of Skin • Protection (physical & immuno-regulation) • Contains Touch and pressure receptors • Thermoregulation • Secretion of Antibacterials & Synthesis of Vitamin D • Excretion of metabolic wastes Protection Against … • • • • • • Microorganisms Chemicals Heat UV radiation Dehydration Mechanical stresses Sense of Touch • Touch is composed of various senses – Somatic - sensations of temperature, pressure, & pain – Kinesthetic - give conception of body in space (proprioception) – Visceral - such as stomach aches or nausea Touch Sense • In humans, about 90% of somatosensory cortex processes touch signals from hands & face • Touch senses in these areas is correspondingly sensitive/high-resolution • Palm can detect presence of fraction of gram Touch receptors • Hairless skin (Glabrous) has finest receptors – Mechanoreceptors translate physical force into nerve impulses – Four main mechanoreceptors in hairless skin areas • Pacinian corpuscles • Meissner's corpuscles • Merkel's discs • Ruffini corpuscles Touch processing • Processed in postcentral gyrus – About top middle area of brain – Often referred to as primary somatosensory cortex – More direct sensory input information than any other part of brain Thermoregulation • Skin is major organ controlling heat & moisture flow to/from surrounding environment • Skin also has thermal sensors – participate in thermoregulatory control – affect person’s thermal sensation & comfort Heat production • Most of body’s heat production is in – Liver – Brain – Heart – Skeletal muscles during exercise • Human body is only 25% efficient – loses approximately 75% of energy as heat Regulating Body Temperature • Heat is transferred – Through network of blood vessels & tissue – To skin • Heat exchange mechanisms include – Heat transfer at skin surface via • Conduction (sitting on cold surface) • Convection (air temperature colder than body) • Radiation (long-wave and short-wave) – Via moisture evaporating/diffusing through skin – Sweat evaporation on skin surface – Respiration from lungs Brain and Body Heat • Brain is about 2% of body mass, BUT produces about 15% of body’s total metabolism – During high mental activity, this neuron metabolism can more than double – Head has specialized thermoregulatory physiology • Assures high rates of heat loss • Keeps brain temperature constant Thermoregulation • Core temperature regulated by brain’s hypothalamus (AKA body’s thermostat) • Hypothalamus responds to various temperature receptors located thruout body • Makes physiological adjustments to maintain constant core temperature – EX: On a hot day, temperature receptors located in skin send signals to hypothalamus to increase sweat rate Sweating • Average person has 2.6 million sweat glands • Sweat is made up of water & electrolytes such as sodium, chloride, and potassium • When hypothalamus senses increase in core temperature – increases blood flow to skin – stimulates sweat glands • Result - increase in rate of water lost through sweating Secretion of Antimicrobials • The skin generates a number of antimicrobial peptides/proteins (AMPs) • Provide a front-line component in innate immunity • Inhibit microbial invasion Synthesis of Vitamin D • UV rays from sun strike skin • D from sun exposure, food, & supplements is biologically inert • Must undergo 2 hydroxylations in body • Liver converts D to 25-hydroxyvitamin D [25(OH)D], AKA calcidiol • Kidney forms physiologically active 1,25dihydroxyvitamin D [1,25(OH)2D], AKA calcitriol Excretion of Wastes • Integumentary system supports excretory system in removal of waste • Skin provides for removal of – dead cells and sweat - contains waste products • Hair, fingernails & toenails – accumulations of dead epidermal cells • As more cells die – Need removal – Hair & nails grow Waste in Sweat • Sweat contains metabolic waste products—primarily – Sodium chloride – Urea – Lactic acid – Potassium ions Components of Integumentary System • Integument = average of 1 mm thick – Epidermis – Dermis – Hypodermis • Accessory Tissues (Dermal Appendages) – Sweat glands – Oil (sebaceous) glands – Hair – Nails Layers of Skin • Epidermis – Five layers – Keratin-producing cells • Dermis (Cuteus) – True skin • Hypodermis – Subcutaneous layer of connective tissue – Contains dermal appendages – Nerves – Blood vessels that supply dermis http://www.nlm.nih.gov/medlineplus/ency/imagepages/8912.htm Epidermis • About 0.012 cm thick • Can thicken for greater protection – Constant friction/pressure – Callus or Corn • Average turnover time for epidermis = ? Epidermis Strata • • • • • Stratum Corneum Stratum Lucidum Stratum Granulosum Stratum Spinosum Stratum Basele http://www.nku.edu/~dempseyd/skin%20layers.jpg Stratum Corneum • Outermost, Toughest layer of skin • First defense against – Microorganisms, UV, chemicals, heat • Flat, dead skin cells • Cells are cornified, filled with keratin Stratum Lucidum • Clear layer holding substance – Becomes keratin as cells ascend – Pre-keratin = Eleidin • Eleidin is found mostly in palms/soles – Thick skin Stratum Granulosum • Flattened cells – No nuclei • Granular appearance • Due to Keratohyalin – Also becomes Keratin Stratum Spinosum • • • • AKA Squamous Larger layer Produces keratin for epidermis Spinous processes projecting between adjacent, new Keratincytes Stratum Basale • AKA Germinativum • Single layer – Cuboidal and columnar cells – Undergo mitosis – Keratinocytes divide • Begin to move up Dermis • • • • AKA cuteus or corium 2 layers Papillary - L, papilla, nipple Reticular - L, reticulum, little net – having a netlike pattern or structure • Lymph vessels are in this layer Papillary layer • Top layer of Dermis • Fingerlike projections interface with Epidermis • Give texture to surface (form rete pegs) – Loss of rete pegs with aging – Skin gets thinner – Skin gets smooth, shiny, paper-thin – Lose fingerprints Reticular Layer • Main layer of Dermis • Rest of connective tissue in Dermis Hypodermis • AKA Subcutaneous • Layer of cushioning fat at base • Superficial fascia connecting dermis to muscle Epidermal Cells • Four types of cells – Keratinocytes Gk, keras, horn – Melanocytes Gk, melanin, black – Langerhans cells – Merkel cells • Each one can have specific types of tumors Keratinocytes • Produce Keratin – Scleroprotein, main component of – Hair, skin, nails – tough and insoluable – Hard, unmineralized structures on many animals • Scales, claws, horns, hooves, feathers, shells • Divide and grow in lower epidermal layers, then flatten, stack, and cornify as they ascend • Kerartinization (Cornification) – Outer epidermal layer is waterproof and prevents dehydration Melanocytes • Produce Melanin – Pigment that colors skin and hair – Melanocytes in darker-skinned people are more active; same number of melanocytes – Moles, freckles, suntans – Protects the skin against UV radiation • Located in lowest level of epidermis – Stratum basale Langerhans Cells • Paul Langerhans (1847 - 1888) German pathologist, physiologist & biologist • Migrate from bone marrow • Begin immune response against antigens due to infection – Similar to macrophages • Located in stratum spinosum layer Merkel Cells • Friedrich S. Merkel, German anatomist – Described in 1875 • Function not completely understood – Light touch for hand dexterity – Discrimination of shapes/structures – Both sensory and hormonal functions – Sometimes referred to as neuroendocrine cells • Located in basal layer Dermal Cells • 3 types of cells – Fibroblasts – Mast cells – Macrophages • Each type has different function Fibroblasts • Synthesize extracellular matrix precursors – Collagen – Reticular and elastic fibers – Glycoproteins • Determines properties of connective tissue • Structural framework of dermis; ability to move • Main function – Maintain structural integrity of skin Mast cells • • • • • • AKA mastocyte or labrocyte In tissues with some interface to outside Also found in digestive and respiratory tracts Do NOT circulate Hypersensitivity reactions of skin Contain/release chemical mediators (histamine, etc.) in response to triggers Mast cells, cont. • Triggers vary & are individual – External OR Internal – Can vary from day to day • Set off a mast cell response – Antibiotics, foods, food additives – Stress, fatigue, heat, cold, sunlight – Bacteria or fungi – Toxins, smells • When triggered • Degranulate – Release chemicals – All at once OR – Slow, leaky process Macrophages • • • • Gk, makros, large + phagein, to eat Ingest cellular debris, pathogens Key role in immune response Help destroy tumor cells, invading microgranisms (bacteria, protozoa) • Type of WBC – Derived from bone marrow – Reside in tissue, monocytes migrate via blood – Become marcrophages in tissue Macrophages, cont. • Integrates pathogen’s antigen into own cell membrane • Presents to other immune cells, causes • Creation of antibodies – Attach to antigen, destruction easier • Releases many types of chemicals – Enzymes – Complement proteins – Interleukin regulators • Stimulate lymphocytes Hypodermal Cells • Mainly fat cells • Cushioning layer • Some fibroblasts & macrophages Skin Tissues • Each Layer of Skin has different tissues with different functions • • • • • • • • • Epithelial Collagen Elastin Reticulin Follicles Glandular Nervous Blood vessels Fatty tissue Epidermis Tissue • Epithelial tissue only • Protects all exposed areas of body organs – Against Abrasion and injury • Surfaces & lining of ducts/cavities • Controls passage of material from outside into organ’s cells • Contains nerve fibers for sensory awareness Dermis • 3 types of fibrous connective tissues – Collagen, Elastin, Reticulin • Strength, Firmness, Flexibility • All arranged irregularly, haphazardly • Allows skin to flex, stretch, contract when stressed Collagen • • • • One of most abundant proteins in body Firmness Connects and Supports body structures Immense tensile strength Elastin • Helps keep skin flexible, tight • Ability to bounce back • Return to normal shape Reticulin • Protein fibers • Crosslinked supportive meshwork for soft tissue Break Time Dermis Accessory Tissues • Specialized Epithelial Tissues (Exocrine) – Sebaceous (Oil) glands – Sudoriferous (Sweat) glands • Hair follicles • Nerves Hair Structures • Tricho- Gk: hair [thread; filament; condition of the hair] • Integrated with sebaceous glands – Shaft = Hair above surface • Cornified (dead) by time leaves surface – Follicle = from matrix (bulb) in dermis extending to surface at angle – Erector Pilus = muscle attached to follicle • Protects and decreases heat loss Hair Structures http://etc.usf.edu/clipart Skin Muscles • Arrector pili (sing.) • Contraction – Goose bumps/gooseflesh – AKA Horripilation or cutis anserina L goose skin – Caused by stimulus (cold or fear) • Causes nerve discharge from sympathetic nervous system, part of ANS (involuntary) • nerve discharge causes contraction of arrectores pilorum (hair erectors) • Benefits ? – Part of fight or flight reaction? Types of Hair • Lanugo – soft downy hair covering fetus of some mammals • Vellus hairs – fine hairs appearing after lanugo hairs cast off – persist until puberty • Terminal hairs – coarse hair on various areas of adult body Hair Growth Cycle • 3 Phases of the life of a hair – Anagen (about ½ inch/month, about 5 years) 1st phase of hair cycle, in which synthesis of hair occurs – Catagen (2-3 weeks) Transitional phase of hair cycle between growth and resting of follicle – Telogen Resting phase of follicle in hair cycle Hair cell growth • The cells of hair bulb divide every 23 to 72 hours, faster than any other cell in body • Chemotherapy and hair? Gland tissue • Sebum = oily substance – Lipids – Oils skin and hair – Prevents drying/cracking – Limits growth of bacteria • Sweat – Watery, has salts – Cools body, Role in thermoregulation – Delivers metabolic waste to surface Sweat Glands • 2 main types of sudoriferous or sweat glands – Eccrine glands – (palms, soles, forehead) • temperature control – Apocrine glands - sweat, fats, proteins • slightly more viscous sweat (scent glands) • mainly present in armpits and around anogenital area ears, hands, cheeks, navel, and areolas • 2 other types of sudoriferous glands – produce modified sweat – Ceruminous glands - ear wax – Mammary glands - milk Nervous tissue • Deep in dermis • Many different types of sensory receptors • Perceive stimuli • Transmit impulses to brain Nerve Tissue • Pacinian corpuscles – Detect vibrations/heavy touch • Meissner’s corpuscles – Detect light touch – Provide protection – painful/harmful Nerve Tissue • Ruffini corpuscle – specialized sensory nerve organs in skin & mucous membranes for perceiving heat • Krause corpuscle (end bulb) – bulboid encapsulated nerve endings located in mucous membranes and activated by cold • Free nerve ending – receptor nerve ending NOT enclosed in a capsule Hypodermis Tissue • Connective tissue – Connects overlying epidermis/dermis to underlying muscle • Dermal appendages – Hair, sweat and oil glands • Blood vessels • ANS nerves • Fatty tissue Skin and Aging • Epidermis thins, although number of cell layers remains unchanged • Number of melanocytes decreases • Remaining melanocytes get larger • Large pigmented spots (age spots, liver spots, or lentigos) – may appear in sun-exposed areas Skin and Aging • Elastosis or Solar elastosis – skin's strength and elasticity is reduced • changes in connective tissue strength & elasticity • Leathery, weather-beaten appearance – Farmers – Sailors – Others • Spend a large amount of time outdoors • Tanning beds Skin and Aging • More fragile Dermal Blood vessels – Bruising, bleeding under skin (often called senile purpura), cherry angiomas, etc. • Less oil produced by Sebaceous glands – Men experience a minimal decrease • usu. after 80 – Women gradually produce less oil at menopause – May make it harder to keep skin moist • Cause of dryness and itchiness Skin and Aging • Thinning of subcutaneous fat layer – Reduces normal insulation and padding – Increases risk of skin injury – Reduces ability to maintain body temperature – Increases risk of hypothermia in cold weather • Less sweat produced by sweat glands – Harder to keep cool – Increases risk for becoming overheated Skin and Aging • Thinning skin reduces – Ability to sense touch, pressure, vibration, heat and cold – Ability to repair itself • Wound healing may be 4X slower – Higher risk of injury • Thinning skin increases – Risk of pressure ulcers Skin and Aging • MOST skin changes are related to SUN exposure • PREVENTION is important throughout life Nails http://etc.usf.edu/clipart Nails • Nail plate – Emerges from proximal nail fold, bordered either side by lateral nail folds (paronychium) – Hard, keratinized, squamous cells loosely adherent to germinal matrix – Strongly attached to sterile matrix • Nail fold – Most proximal aspect of perionychium – Composed of dorsal roof & ventral floor – Found approximately 15 mm distal to DIP Nail fold • Dorsal roof rests above forming nail – Houses cells that give shine to nail • Ventral floor lies beneath nail – Immediately distal to insertion of extensor tendons – Site of germinal matrix – Responsible for 90% of nail production • Eponychium – Skin proximal to nail that covers nail fold • Cuticle – Tissue distal to eponychium in contact w/nail Lunula • Half-moon shaped white arc – Proximal to distal on nail • Distal extent of germinal matrix • Characteristic color change – Due to persistence of nail cell nuclei in germinal matrix • Distal to this location – Nuclei absent – Nail transparent Sterile matrix • Area of nail bed distal to lunula • 2ndary site of nail production • Tightly adherent to – Nail plate – Periosteum of distal phalanx Hyponychium • Junction formed bet. sterile matrix & fingertip skin beneath nail margin – Susceptible to contamination from environmental interactions – Keratin plug acts as mechanical barrier to protect against infectious innoculation • Has polymorphonuclear leukocytes & lymphocytes • Contributing immunologic barrier to mechanical barrier Nail Blood Supply • Perionychium – Arterial blood supply from terminal branches of radial & ulnar proper palmar (volar) digital arteries – These originate proximal to metacarpophalangeal joint from common palmar digital arteries • Proper palmar digital arteries – Branch proximal to DIP joint – Have branch that travels dorsal to DIP joint – Supplies superficial arcade that feeds nail fold & proximal matrix Nail anatomy Section of last bone of finger 5, Fat, forming the cushion at the end of the finger 2, The nail 1, The cuticle continued under and around the 3 Root of the nail Breast • ICD -9/10-CM – part of Reproductive System Chapter • CPT – part of Surgery/Integumentary System Section Female Breast http://training.seer.cancer.gov/breast/anatomy/ Male Breast http://www.cancer.gov/images/cdr/live/CDR694414-750.jpg Breast Anatomy • Located in upper ventral region – Over pectoralis major muscles – Extends from 2nd to 6th rib – Superior lateral quadrant extends diagonally upwards into axillary area • To Tail of Spence • AKA Spence's tail, axillary process, axillary tail • James Spence (1812-1882), Scottish surgeon – Thin layer of mammary tissue • From clavicle to 7th/8th rib • From midline to edge of latissimus dorsi posterior Breast Quadrants • For clinical purposes, the breast is divided into four quadrants • Upper inner • Upper outer (largest) • Lower inner • Lower outer Breast Tissue • Breast is a combination of – Lactiferous (milk-producing) ducts – Connective tissue – Adipose tissue – Cooper's ligaments • help support the breast Breast Anatomy • Blood supply – Internal thoracic (internal mammary) artery – Lateral thoracic, thoraco-acromial and posterior intercostals arteries • Blood drainage – Axillary, internal thoroacic, & intercostal veins • Nerves – Anterior/lateral cutaneous branches of 4th -6th intercostal nerves Breast Components • Contains mammary glands – Various sizes, distributed thru out breast – Modified sweat glands • • • • Nipple and areola Connective tissue Adipose tissue Cooper ligaments Nipple • Nipple surrounded by areola – Drainage point for lactiferous ducts – Each duct has own opening – Large # of blood vessels – Large # of nerves • Erection in response – Sexual stimuli – Cold – Touch – Enabled by nerve and blood supply Areola • Areola – varies in color – pink to dark brown – Contains sebaceous glands • Mammary glands and milk – Milk at back of breast – Suckling makes smooth muscles of mammary glands to be pushed to ducts, and then to nipple – 15-25 openings in nipple Breast lymph nodes • Lymph travels from breast to – Ipsilateral axillary lymph nodes – Parasternal nodes – Other breast lymph nodes – Abdominal lymph nodes • Axillary lymph nodes – Pectoral – Subcapsular – Humeral • Central axillary, then to Apical axillary Breast growth • Due to changing sex hormones (puberty) – Estrogen • Pregnancy changes – Larger, firmer – hypertrophy of mammary glands • Prolactin hormone – Nipples may enlarge, become darker • Menstrual cycle – Also may cause breast/nipple changes Homework • Test Your Anatomy IQ – 12 questions – http://www.webmd.com/healthy-beauty/rmquiz-anatomy • Integumentary System. Quizlet. – http://quizlet.com/806630/integumentarysystem-flash-cards/ • Skin, Hair, Nails. Quizlet. – http://quizlet.com/6233503/skin-hair-nails-chp10-flash-cards/ imueller@email.wcu.edu Resources • Alaiti, S. Hair Anatomy. MedScape. – http://emedicine.medscape.com/article/835470overview#showall • Aging changes in skin. MedlinePlus. – http://www.nlm.nih.gov/medlineplus/ency/article/ 004014.htm • Anatomy and Function of the Female Breast. Breast Cancer Causes, cures, and biology. – http://www.celtnet.org.uk/cancer/breastfunction.html Resources • Arens, E A, & Zhang, H. 2006. The skin's role in human thermoregulation and comfort. Center for the Built Environment, University of California, Berkeley. – http://escholarship.org/uc/item/3f4599hx • The Body’s Protective Cover. National Geographic. (Interactive review of skin) http://science.nationalgeographic.com/scienc e/health-and-human-body/human-body/skinarticle/ Resources • California Dept. of Public Health. Anatomy and Pathology. Breast Cancer Review. – http://qap.sdsu.edu/education/bcrl/Bcrl_anatp ath/bcrl_anatpath_index.html • Definition of Arrectores pilorum. MedicineNet.com – http://www.medterms.com/script/main/art.asp ?articlekey=6856 Resources • Markey, Sean. 20 things you didn’t know about skin. Discover, 2/2007 – http://discovermagazine.com/2007/feb/20-things-skin/ • Niyonsaba, F. et.al. Antimicrobial Peptides Human β-Defensins and Cathelicidin LL-37 Induce the Secretion of a Pruritogenic Cytokine IL-31 by Human Mast Cells. The Journal of Immunology April 1, 2010 vol. 184 no. 7 35263534 – http://www.jimmunol.org/content/184/7/3526.full Resources • Philips, B. Z., et. al. Nail Anatomy. MedScape. – http://emedicine.medscape.com/article/1948841overview#a1 • Vitamin D: Dietary Supplement Fact Sheet. NIH. Office of Dietary Supplements. – http://ods.od.nih.gov/factsheets/VitaminDHealthProfessional/ Videos • Components of skin. MedlinePlus. – http://www.nlm.nih.gov/medlineplus/ency/anat omyvideos/000029.htm • What is skin? The layers of human skin. Clinuvel http://www.clinuvel.com 3.48 minutes video – http://www.youtube.com/watch?v=yKAzVC0W cmI&feature=related Videos • The Integumentary System - The Derivatives of the Integumentary System. Rapid Learning Center. 9.21 minute video. – http://www.youtube.com/watch?v=nRH8MarC58&feature=channel&list=UL • The Integumentary System - What is Histology? Rapid Learning Center. 2.40 minute video. – http://www.youtube.com/watch?v=wrJwOoNdd1I&feature =relmfu Videos • The Integumentary System - What's the Epidermal Layer of the Skin? Rapid Learning Center. 7.44 minute video. – http://www.youtube.com/watch?v=R7_arNsaxPs&feat ure=related • The Integumentary System - What is the Dermal Layer of the Skin? Rapid Learning Center. 8.30 minute video. – http://www.youtube.com/watch?v=bmLxUnpdK9I&feat ure=relmfu