lipid metabolism (catabolic, supply and storage processes)
advertisement

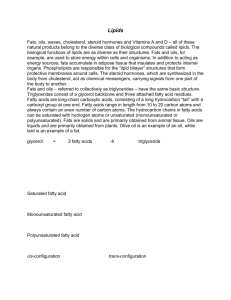
LIPID CATABOLISM (BREAKDOWN, STORAGE AND SUPPLY PROCESSES) References: Garrett/Grisham Biochemistry (4th ed), chs. 23 and sections of 24 Berg, Tymoczko & Stryer Biochemistry (6ht ed)., sections of ch 26 Lupton et al Dietary Reference Intakes, National Academies Press, 2005. LIPIDS ARE A PART OF OUR DIET THAT CONTRIBUTE A LOT OF FLAVOR (PIZZA!) ….AND SOME PROBLEMS WITH STORAGE ACCUMULATION (FAT & PLAQUE!). WE CANNOT DO WITHOUTLIPIDS IN OUR DIETS. THIS LECTURE IS NOT ABOUT WEIGHT CONTROL – IT IS A BIOCHEMICAL EXPOSE’ OF HOW LIPIDS ARE “DIGESTED”. OUTLINE: 1) INGESTION AND BREAKDOWN OF LIPIDS 2) TRANSPORT OF DIETARY LIPIDS TO CELLS --WITH THE CHOLESTEROL CONNECTION 3) STORAGE OF LIPIDS AND VARIATIONS 4) MOBILIZATION OF LIPIDS FROM STORAGE 5) CONVERSION TO ENERGY LIPIDS ARE INGESTED INTO THE BODY IN BASICALLY TWO FORMS: TRIACYLGLYCEROLS AND CHOLESTERYL ESTERS. (This is in an approximate ratio of 9:1.) THE BODY WILL USE THE FATTY ACIDS FROM THE TRIACYLGLYCEROLS FOR: 1) ENERGY 2) MEMBRANE SYNTHESIS WHILE THE CHOLESTEROL FROM THE CHOLESTERYL ESTERS WILL BE USED FOR: 1) MEMBRANE SYNTHESIS 2) HORMONE FORMATION INGESTION THREE AREAS IN THE GASTROINTESTINAL TRACT IN WHICH LIPIDS COULD BE BROKEN DOWN OR PROCESSED: B A: THE STOMACH B: THE DUODENUM C: THE INTESTINAL EPITHELIUM DUODENAL LIPIDS and cholesteryl esters A C THE STOMACH IS THE 1st ORGAN IN WHICH TRIACYLGLYCEROLS AND CHOLESTEROL/ ESTERS RESIDE, BUT VERY LITTLE CHANGE OCCURS HERE DUE TO STOMACH ACIDITY (& ENZYME ABSENCE). THE DUODENUM CONTAINS ALKALINE PANCREATIC & GALL BLADDER SECRETIONS MADE UP OF PANCREATIC LIPASES , ESTERASES & BILE SALTS TO BREAK DOWN TRIACYLGLCEROLS & CHOLESTERYL ESTERS. PANCREATIC LIPASES & ESTERASES NOTE: n-sp LIPASES REMOVE THE FATTY ACID FROM THE 2 POSITION AND AS WELL AS THE FATTY ACIDS FROM CHOLESTERYL ESTERS. RELEASED FATTY ACIDS INTESTINAL EPITHELIUM (mucosal cells) 1) SHORT CHAIN FATTY ACIDS (<10 C) ARE DIRECTLY TAKEN UP INTO THE INTESTINAL MUCOSAL CELLS WHILE LONGER CHAIN FATTY ACIDS + BILE SALTS (MIXED MICELLES) ARE CARRIED TO THE EPITHELIAL CELLS (MUCOSAL CELLS) FOR UPTAKE. 1) LIPID UPTAKE Intestinal lumen 2) CONDENSATION 2) INSIDE THE EPITHELIAL CELLS NEW TRIACYLGLYEROLS AND CHOLESTERYL ESTERS ARE REFORMED (CONDENSED) BY THE ACTION OF AN ACYL TRANSFERASE. 3) THE NEW LIPID ESTERS ARE COMBINED WITH APOLIPOPROTEINS TO FORM CHYLOMICRONS FOR TRANSPORT THROUGH THE LYMPH AND BLOOD VESSELS. 3) “PACKAGING” TRANSPORT LIPIDS AS TRIACYLGLYCEROLS, CHOLESTEROL AND CHOLESTERYL ESTERS BEGIN TO MOVE THROUGH THE BODY AS CHYLOMICRONS – SPHERICAL BODIES THAT ALSO CONTAIN PHOSPHOLIPIDS AND APOLIPOPROTEINS BOUND AT THE SURFACE. THE PHOSPHOLIPIDS COME FROM THE MUCOSAL CELL PMs WHILE THE APOLIPOPROTEINS ARE FROM THE MUCOSAL CELL INTERIOR. THE APOLIPOPROTEINS ACT AS MARKERS AND ACTIVATORS FOR THE RELEASE OF CHYLOMICRON CONTENTS AT SPECIFIC KINDS OF CELLS. IN THE TRANSPORT OF LIPIDS, CHYLOMICRONS DELIVER LIPIDS TO ADIPOSE TISSUE AND PERIPHERAL TISSUES (1) WHILE THE REMNANTS GO TO THE LIVER (2). VERY LOW DENSITY LIPOPROTEINS LEAVE THE LIVER AND DELIVER LIPIDS TO ADIPOSE AND PERIPHERAL TISSUES (3). THE REMNANTS ARE CONVERTED TO LOW DENSITY LIPOPROTEINS (LDL) AND GO TO PERIPHERAL TISSUES AND THE LIVER (4). AT PERIPHERAL TISSUES, HIGH DENSITY LIPOPROTEINS (HDL) ARE FORMED FROM PRECURSORS AND GO TO THE LIVER (5). HDL precursor 1 3 1 3 4 2 5 THE MOST “SIGNIFICANT” LIPOPROTEINS IN MEDICAL RESEARCH ARE PRESENTLY THE LOW DENSITY LIPOPROTEINS (CONTAINING SO CALLED “BAD” CHOLESTEROL) AND HIGH DENSITY LIPOPROTEINS (CONTAINING SO CALLED “GOOD” CHOLESTEROL). DELIVERY OF LIPIDS TO/ FROM CELLS & BLOOD CHOLESTEROL LEVELS WHAT ARE THE ROLES OF THE LDL AND HDL LIPOPROTEINS? LDL LIPOPROTEINS CARRY CHOLESTEROL MOLECULES TO PERIPHERAL TISSUES AND REGULATE NEW CHOLESTEROL SYNTHESIS AT THESE SITES. HDL LIPOPROTEINS PICK UP CHOLESTEROL RELEASED INTO BLOOD PLASMA FROM DYING CELLS AND FROM CELL MEMBRANE TURNOVER. HDL IS A CHOLESTEROL SCAVENGER AND DETERS BUILD-UP OF CHOLESTEROL PLAQUE INSIDE OF BLOOD VESSELS BY TAKING IT TO THE LIVER. IT IS IMPORTANT THAT LDL IS ABLE TO DELIVER CHOLESTEROL TO ITS TARGET CELLS AND HDL IS ABLE TO PICK UP DISCARDED CHOLESTEROL. AN INDICATION OF HOW WELL THIS IS WORKING CAN BE SEEN IN A LAB TEST OF THE HDL/ LDL RATIO WHICH IDEALLY IS 3.5:1. THIS FUNCTIONAL ABILITY IS RELATED TO THE APOLIPOPROTEINS THAT ARE FOUND ON LDL (B100) AND HDL (A). B100 CAUSES CHOLESTEROL UPTAKE INTO CELLS, BUT AN ABSENCE OF RECEPTORS FOR B1OO LEADS TO FAMILIAL HYPERCHOLESTEROLEMIA. DELIVERY MECHANISM OF CHOLESTEROL TO ADIPOCYTES AND MUSCLE CELLS THE UPTAKE OF CHOLESTEROL INTO ITS TARGET CELLS USES RECEPTOR MEDIATED ENDOCYTOSIS FOR LDL LIPOPROTEINS. THE PROCESS BEGINS (1) WITH THE BINDING OF AN LDL BODY IN A COATED PIT WITH AN LDL RECEPTOR. AFTER INVAGINATION (1) & REMOVAL OF A (3) COAT PROTEIN (2), THE TRAPPED LDL IS FUSED WITH A LYSOSOME(LYS). THE LYS HAS DEGRADATIVE ENZYMES (**) THAT DEGRADE ITS apo-B & CHOLESTEROL ESTERS INTO AMINO (2) (4) ACIDS & FREE CHOLESTEROL (3). CHOLESTEROL MAY THEN BE STORED OR USED FOR MEMBRANE SYNTHESIS (4). Note: ACAT should be LCAT. **PROTEASES FOR apo-B AND LCAT(lecithin:cholesterolacyltransferase)for cholesterol esters. HOW ARE TRIACYLGLYEROLS RELATED TO CHOLESTEROL LEVELS? WHAT ABOUT THE DELIVERY OF TRIACYLGLYCERIDES TO CELLS? TRIACYLGLYEROLS ARE TRANSPORTED TO ADIPOCYTES AND PERIPHERAL TISSUES (e.g. MUSCLES) VIA CHYLOMICRONS AND VLDLs/LDLs. THE MAJORITY OF TRIACYLGLYCEROLS ARE CARRIED IN CHYLOMICRONS (NORMAL DIETARY SUPPLY FOR FAT AND MUSCLE CELLS) AND VLDLS (EXTRA SUPPLY THAT COMES FROM THE LIVER). CLINICALLY, WHEN SERUM TRIACYLGLYERIDES (TAGs) ARE ELEVATED, IT USUALLY MEANS THAT THE LDLs (WITH 2.5 x MORE TAGs THAN HDLs) ARE INCREASED IN RELATION TO HDLs**. WHEN THIS OCCURS, CHOLESTEROL IN LDLs INCREASE AS WELL AND THAT INCREASES THE CHOLESTEROL THAT MIGHT BE DEPOSITED INSIDE OF CIRCULATORY BLOOD VESSELS. ** AN ADIPOCYTE (“cellulite”) HOW DOES THE COMPOSITION OF FATTY ACIDS IN TRIACYLGLYCEROLS AFFECT LIPOPROTEIN COMPOSITION? -- SATURATED vs. UNSATURATED FATTY ACIDS? -- TRANS vs. CIS FATTY ACIDS? THIS IS A QUESTION THAT HAS PERPLEXED NUTRITIONAL RESEARCHERS FOR MANY YEARS. ALL THAT IS PRESENTLY KNOWN SUGGESTS THAT: 1) SATURATED FATTY ACIDS INCREASE LDL LEVELS ONLY. 2) TRANS FATTY ACIDS INCREASE LDL LEVELS AND LOWER HDL LEVELS THE CAUSE IS UNKNOWN, BUT SOME EVIDENCE INDICATES THAT THIS IS DUE TO HORMONAL EFFECTS ON THE APOLIPOPROTEIN LEVELS THAT PRODUCE EACH LIPOPROTEIN CARRIER. THAT IS, THE AMOUNTS OF apoA-1 AND apoB-100 ARE AFFECTED. THERE IS NO DOUBT THAT INCREASED SATURATED AND TRANS-FATTY ACIDS IN THE DIET INCREASE THE LDL TO HDL RATIOS AND, ACCORDINGLY, THE AMOUNT OF CHOLESTEROL THAT CAN BE “DUMPED” INTO BLOOD VESSEL INTERIORS. WITH ALL OF THAT WE NEED SOME COMIC RELIEF! MARY HAD A LITTLE LAMB (OLD VERSION) “MARY HAD A LITTLE LAMB. ITS FLEECE WAS WHITE AS SNOW AND EVERYWHERE THAT MARY WENT, THE LAMB WAS SURE TO GO.” THE NUTRITIONAL VERSION OF THAT IS -- MARY HAD A LITTLE LAMB: “AND THAT EVENING, WITH HER BLINDS PULLED DOWN, MARY HAD 3 HELPINGS OF CORN, A BAKED POTATO, EXTRA BREAD, AND A LITTLE LAMB” -- WITH APOLOGIES TO THE LAMB NEXT: DELIVERY OF FATTY ACIDS TO ADIPOCYTES AND MUSCLE CELLS WHEN A LIPOPROTEIN CARRIER REACHES ITS TARGET AREA, TAGs ARE RELEASED BY THE COMBINED ACTION OF THE APOLIPOPROTEIN/RECEPTOR (HOLDS THE CARRIER NEXT TO THE BLOOD VESSEL ENDOTHELIAL CELL) AND A CELL MEMBRANE BOUND LIPASE (ENZYME THAT LYSES FFAs AND MONOGLYCERIDES) FOR TRANSPORT INTO THE TARGET CELL. THIS WORKS WHEN THE LIPOPROTEIN CARRIER PARKS NEXT TO A BLOOD VESSEL WALL CELL THAT ENZYMATICALLY RELEASES FFAs AND MONOGLYCERIDES TO BE TAKEN UP BY TISSUE CELLS ON THE OTHER SIDE OF THE BLOOD VESSEL: DELIVERY OF FFAs/MONOGLYCERIDES IS SHOWN FOR CHYLOMICRONS, BUT THE MECHANISM IS SIMILAR FOR VLDLs AS WELL. NOTE THE PRESENCE OF CD36 THAT IS ASSOCIATED WITH THE RELEASED FFAs. CD36 IS A PROTEIN THAT BINDS TO THE FATTY ACID AND TRANSPORTS IT THROUGH THE ENDOTHELIAL CELL TO THE ASSOCIATED TARGET CELL. THE USES OF FATTY ACIDS – A REVIEW AND AN INTRODUCTION TO b-OXIDATION EARLIER, IT WAS SAID THAT FATTY ACIDS MAY BE USED TO STORE ENERGY AS WELL AS TO PRODUCE ENERGY. THERE ARE ALSO MINOR ROLES, FOR EXAMPLE, IN THE STORAGE FORM - FATTY ACIDS ARE GOOD INSULATORS AND THEY CAN ALSO FORM INTO HORMONE-LIKE COMPOUNDS. AS YOU HAVE SEEN, FATTY ACIDS HAVE TO BE CHEMICALLY MINIPULATED TO BE TRANSPORTED THROUGH THE BODY DUE TO THEIR SOLUBILITY “PROBLEM” IN AQUEOUS MEDIA SUCH AS BLOOD PLASMA. THIS IS ALSO TRUE INSIDE THE CELL WHEN IT BECOMES NECESSARY TO USE FATTY ACIDS FOR ENERGY. IN FACT, THERE ARE MANY CELL TYPES THAT MAKE USE OF FATTY ACIDS AS AN ENERGY SOURCE WHEN THE BODY IS STARVED FOR GLYCOGEN /GLUCOSE. NOTE THAT HEART TISSUE AND MUSCLES NORMALLLY PREFER FATTY ACIDS AS A FUEL SOURCE. BRAIN TISSUE CAN ONLY USE FATTY ACIDS AFTER THEY HAVE BEEN BROKEN DOWN TO KETONE BODIES. ACETOACETATE AND b-HYDROXYBUTYRATE ARE CONVERTED TO ACETYL-CoA FOR USE IN THE KREB’S CYCLE. THEY ALSO CONTRIBUTE TO BODY ACIDITY, A PROBLEM IN DIABETES. A NUTRITIONAL REVIEW OF FATTY ACID VS. CARBOHYDRATE ENERGY IN METABOLISM 1) TRIACYLGLYCEROLS (TAGs) ARE A MAJOR FORM OF STORED ENERGY: (70 kg = 154 lbs.) 1 kJ = 0.239 kcal (TAGs REPRESENT 84% OF ALL THE STORED BODY ENERGY) 660,360 kJ = ~157,827 kcal 2) IN NORMAL METABOLISM (NOT FASTING, STARVING OR DIABETIC): MUSCLE: FFA ARE PREFERRED, THEN GLUCOSE HEART: KETONE BODIES ARE PREFERRED, THEN GLUCOSE BRAIN & RBCs: GLUCOSE IS PREFERRED, THEN KETONE BODIES KIDNEYS: KETONE BODIES ARE PREFERRED, THEN GLUCOSE 3) FFA ACETYL CoA KETONE BODIES ACETYL CoA TCA CYCLE KETONE BODIES ARE A SOLUBLE FORM OF FFA BREAKDOWN THAT CAN BE TRANSPORTED IN THE BLOOD. SOME ARE ALWAYS PRESENT. THEREFORE: 1. TAGs (AS FATTY ACIDS) ARE AN IMPORTANT SOURCE OF SUSTAINED ENERGY IN PERIPHERAL MUSCLE, HEART AND KIDNEYS – THE LATTER AS KETONE BODIES. 2. UNDER STARVATION CONDITIONS, FATTY ACIDS BECOME VERY IMPORTANT AS A MAJOR SOURCE OF ENERGY EVEN FOR BRAIN TISSUE. 3. TAGs ARE CONSUMED IN HIGHER THAN REQUIRED AMOUNTS IN THE DIETS OF MANY OF THE “DEVELOPED” NATIONS…. WITH THE RESULT THAT CHOLESTEROL MAY BE DUMPED INTO BLOOD VESSELS TO FORM PLAQUE DUE TO THEIR DELIVERY WITH LDLs CONTAINING TAGs. THE MOBILIZATION OF STORED LIPIDS WHEN THE BODY “SENSES” THAT TAGs ARE REQUIRED FROM ADIPOCYTES OR OTHER CELLS, IT CONVERTS THE TAGs TO A TRANSPORT FORM AND MOVES THEM TO A LOCATION WHERE THEY CAN BE USED – USUALLY FOR ENERGY. HOW DOES THE BODY “SENSE” SUCH A NEED? HOW DOES THE BIOCHEMICAL CONVERSION TAKE PLACE? WHAT IS INVOLVED IN TRANSPORT? “SENSATION” OR SIGNALLING OF LIPID NEED & TAG BREAKDOWN 1) MOBILIZATION IS SIGNALLED BY HORMONE BINDING TO A RECEPTOR PROTEIN. 2) THIS TRIGGERS A “CASCADE” MECHANISM OF ENZYME ACTIVATIONS. 3) THE LAST ENZYME ACTIVATED IS A TRIACYLGLYCEROL LIPASE. 4) THE REPETITIVE LIPASE CATALYSIS CAUSES THE SEQUENTIAL RELEASE OF FATTY ACIDS FROM TAGs IN THE ADIPOCYTE. 5) FREE FATTY ACIDS LEAVE THE CELL 1) 5) 2) 2) 3) (TAG) 4) NOTE: INACTIVE COMPOUNDS OR ENZYMES ARE IN RED WHILE ACTIVE COMPOUNDS OR ENZYMES ARE IN GREEN. HORMONES INVOLVED IN SIGNALLING LIPID MOBILIZATION: ALTHOUGH HORMONES AS A CLASS OF BIOCHEMICALS HAVE NOT YET BEEN ADDRESSED IN THESE LECTURES, SUFFICE IT TO SAY THAT THEY ACT AS SWITCHES TO TURN ON/ OFF AN INTRACELLULAR PROCESS. THE EXTRACELLULAR HORMONES INVOLVED IN LIPID MOBILIZATION ARE: ADRENOCORTICOTROPIC HORMONE (ACTH) EPINEPHRINE GLUCAGON THEY BIND TO A 7-HELIX RECEPTOR PROTEIN IN ORDER TO ACTIVATE THE CASCADE MECHANISM. CASCADE MECHANISMS WILL BE CONSIDERED LATER UNDER HORMONES. WHAT HAPPENS TO THE “RELEASED” FATTY ACIDS OUTSIDE THE CELLS? ONE MIGHT PREDICT THAT THE RELEASED FATTY ACIDS ARE TAKEN UP AGAIN INTO LIPOPROTEIN BODIES (SUCH AS LDLs) FOR TRANSPORT, BUT THAT IS NOT THE CASE. THESE FFAs BECOME BOUND TO THE PROTEIN: ALBUMIN FOR TRANSPORT. SHOWN AT THE RIGHT IS AN ALBUMIN MOLECULE (MW ~65,000) TO WHICH ARE BOUND 6 PALMITIC ACID (16:0) MOLECULES (SEEN IN GREY). THEN, PRIOR TO “HARVESTING” THE FATTY ACIDS FOR ENERGY, THE FFAs ARE ACTIVATED BY BEING BOUND TO CoA (CO-ENZYME A). THE THIOL ESTER THAT RESULTS IS A CARRIER FORM (A SOLUBLE FORM) FOR TRANSPORT AND THE ENZYMATIC REACTIONS THAT ARE NEEDED FOR THE FATTY ACID BREAKDOWN. GETTING TO b-OXIDATION -- BUT NOT QUITE! FATTY ACIDS OVER 10 CARBONS LONG ALSO HAVE TO BE TRANSPORTED INTO THE MITOCHONDRIAL MATRIX USING CARNITINE AND SOME “HELPER” MOLECULES BECAUSE OF THE SOLUBILITY PROBLEM. (AKA “TRANSLOCASE”) CARNITINE (CH3)3-N+-CH2-CH0H-CH2-COO- BINDS TO THE ACTIVATED FATTY ACID AS AN ESTER AND IS CARRIED ACROSS THE OUTER AND INNER MITOCONDRIAL MEMBRANES USING TWO ACYLTRANSFERASES AND A TRANSPORTER PROTEIN. A DEFICIENCY OF CARNITINE CAN LEAD TO MUSCLE WEAKNESS. NOTE THEN THAT CoA IS USED TWICE AS A CARRIER OUTSIDE OF THE MEMBRANES. b-OXIDATION (MAKING ATP FROM FATTY ACIDS) KREB’S CYCLE b-OXIDATION IS A PROCESS OF REMOVING 2-CARBON UNITS FROM FATTY ACIDS TO OBTAIN ENERGY via THE KREB’S CYCLE. THE FATTY ACIDS GAIN ENTRY INTO THE MITOCHONDRAL MATRIX BY MEANS OF A CARNITINE CARRIER AFTER “ACTIVATION” WITH CoA. THE FIGURE AT RIGHT SHOWS THE SERIES OF REACTIONS INVOLVING BOTH THE a- AND bCARBONS OF THE FATTY ACIDS. STARTING AT 1, A DOUBLE BOND IS FORMED BETWEEN THE TWO CARBONS. AT 2, H2O IS INSERTED BETWEEN THESE CARBONS. AT 3, THE REMOVAL OF TWO ELECTRONS/2 Hs FORMS A KETO GROUP ON THE b-CARBON (PREPARING FOR SPLITTING THE TWO CARBONS). AT 4, CLEAVAGE OF THE a- AND b- CARBONS FORMS ACETYL CoA (2 CARBON UNIT) AND FATTY ACYL CoA (-2 CARBONS). THE CYCLE CAN THEN BE REPEATED AT . b- AND OTHER OXIDATION NOTES: 1. THE OXIDATION OF ONE PALMITIC ACID MOLECULE (16:0) YIELDS 106 MOLECULES OF ATP vs. GLUCOSE WHICH YIELDS 36-38 ATP MOLECULES. 2. THE CONTRIBUTIONS OF TWO ADDITIONAL ENZYMES ARE NECESSARY TO CONVERT UNSATURATED FATTY ACIDS INTO 2-CARBON UNITS BY b-OXIDATION. 3. BRANCHED CHAIN FATTY ACIDS ARE DEGRADED BY a-OXIDATION. IN REFSUM’S DISEASE, A METABOLIC DISORDER, THERE IS A DEFECT IN a-OXIDATION. REFSUM’S DISEASE CAUSES NEUROLOGICAL DISORDERS AND AFFECTS NIGHT VISION. A SOURCE OF BRANCHED CHAIN FATTY ACIDS COMES FROM CATTLE THAT CONSUME PLANT CHLOROPHYLL – A SOURCE OF THE BRANCHED CHAIN FATTY ACID: PHYTANNC ACID. BRANCHES RESEARCH NOTE: BROWN VS. WHITE (YELLOW) FAT THE NEWS MEDIA HAS MADE SOME NOISE ABOUT THE POSSIBILITY ABOUT “BURNING OFF” EXCESS STORED FAT BY USING A MINOR COMPONENT IN THE BODY KNOWN AS BROWN FAT. BROWN FAT IS A TISSUE THAT HAS CELLS HIGH IN MITOCONDRIAL CONTENT. IT HAS BEEN PROPOSED THAT FAT THAT IS TRANSPORTED TO THIS TISSUE CAN BE OXIDIZED (ESSENTIALLY DESTROYED) BY THIS TISSUE. AT PRESENT THERE IS NO PRACTICAL WAY FOR THIS TO BE REALIZED SINCE: 1) THE AMOUNT OF BROWN FAT IS TOO LOW 2) NO ONE KNOWS HOW TO INDUCE THE TRANSPORT OF THE LIPID CONTENT OF WHITE FAT INTO BROWN FAT TISSUES. SUMMARY OF LIPID CATABOLISM AND NOTEWORTHY POINTS: ●LIPID TRANSPORT IS COMPLICATED BY THE NON-POLAR NATURE OF LIPIDS AND THE NEED TO FORM SPECIAL TRANSPORT FORMS SUCH AS CHYLOMICRA, LIPOPROTEINS & THE USE OF ALBUMIN TRANSPORTERS. KNOW THIS. ●THE PRINIPAL LIPIDS TAKEN INTO THE GI TRACT ARE FATTY ACIDS AND CHOLESTEROL (AS TRIACYLGEROLS AND CHOLESTERYL ESTERS (~9:1). THIS TOO. ●THE PRIMARY USES OF INGESTED LIPIDS ARE: ENERGY, MEMBRANE SYNTHESIS AND HORMONE FORMATION. AND THIS. ●THE DUODENUM EMUSIFIES AND HYDROLYZES LIPIDS WHILE THE SMALL INTESTINE RESYNTHESIZES LIPIDS INTO ESTERS AND FORMS CHYLOMICRA (CHYLOMICRONS). KNOW DETAILS. ●CHYLOMICRA AND LIPOPROTEINS ARE COMPOSED OF LIPIDS AND APOLIPOPROTEINS. THESE ARE BODIES THAT TRANSPORT LIPIDS IN THE LYMPH AND BLOOD VESSELS. KNOW THE DETAILS OF EACH TYPE IN DELIVERING LIPIDS TO EACH CELL TYPE. ●LDLs AND HDLs ARE INVOLVED IN THE POSSIBLE FORMATION OF BLOOD VESSEL PLAQUE AND CARRY WITH THEM THE MISNOMERS OF “BAD” AND “GOOD” CHOLESTEROL . WHY IS THAT? WHAT IS THE REALATIONSHIP OF AN ABSENCE OF RECEPTORS FOR B100 AND FAMILIAL HYPERCHOLESTEROLEMIA? ●CHOLESTEROL IS TAKEN UP INTO CELLS BY ONE MECHANISM WHILE TRIACYLGLYCEROLS BY ANOTHER. KNOW THE DIFFERENCE AND THE DETAILS. ●CLINICALLY AN ELEVATED LDL VS. HDL MIGHT BE A SIGN OF THE POSSIBILITY OF ARTERIAL CLOGING. WHY IS THAT? WHAT MIGHT AN INCREASED INTAKE OF SATURATED VS. UNSATURATED FATTY ACIDS OR TRANS VS. CIS FATTY ACIDS CAUSE? ●b-OXIDATION BREAKS DOWN FATTY ACIDS INTO TWO CARBON UNITS. HOW IS THIS DONE AND WHY IS IT DONE? DETAILS! WHAT IS THE CHEMICAL MECHANISM? ●SOME CELLS PREFER GLUCOSE, SOME FATTY ACIDS AND SOME KETONE BODIES AS SOURCES OF ATP. DOES THIS CHANGE YOUR OUTLOOK ON NUTRITION AND, PERHAPS, YOUR RELATIVE EVALUATION OF GLUCOSE VS. FAT METABOLISM? WHAT ENERGY SOURCE BECOMES QUITE IMPORTANT UNDER STARVATION CONDITIONS? ●WHAT IS MEANT BY THE “MOBILIZATION” OF LIPIDS? HERE AN UNDERSTANDING OF THE ROLE OF HORMONES BECOMES IMPORTANT AS WELL AS THE CARRIER PROTEIN: ALBUMIN. THIS IS ALSO IMPORTANT. ●WHAT IS REFSUM’S DISEASE AND WHAT OXIDATION PROCESS IS IT RELATED TO? THIS SUMMARY – YOU MUST REALIZE – IS ALSO A STUDY GUIDE! ☺