Slide 1 - School of Medicine
advertisement

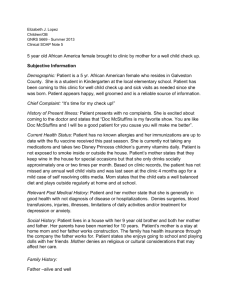
Silsbee Kemp MD Internal medicine HO III July 17, 2012 LSU INTERNAL MEDICINE CASE CONFERENCE Chief Complaint “I feel tired and my legs are swollen.” History of Present Illness 38 year-old man with no previous significant past medical history was in his usual state of health until two months ago when he began experiencing progressively worsening fatigue and decreased exercise tolerance Denies chest pain Denies SOB or DOE Denies PND HPI 1 month ago, the patient was seen at an Urgent Care clinic complaining of a sore throat Denies respiratory symptoms Admits to subjective fevers Per patient, positive “rapid Strep test” Prescribed amoxicillin Only completed 3 days HPI Soon after his Urgent Care clinic visit, the patient began experiencing progressively worsening lower extremity edema 1 week prior to admission, the patient presented to an outside facility for evaluation of this edema Diagnosed with renal failure Sent home with prescription for furosemide HPI Since that time, the patient has not received any relief of his symptoms Difficulty standing on his feet for any significant duration at work (+) nocturnal frequency, Denies dysuria, urgency, polyuria, gross hematuria, decreased urine output Denies excessive NSAID use Denies nausea, vomiting, diarrhea, decreased oral intake History continued… PMHx: Denies PSHx: Denies Home Medications: Denies Allergies: NKDA FHx: Mom with DM II Father unknown History continued… Social Hx: Lives with wife and children in Metairie, LA 2 children ages 5 and 9 Denies tobacco, ETOH, IVDA or illicit drugs Denies recent travel Health Maintenance: Up to date on Tetanus only No PCP Additional ROS: Endorses : Generalized fatigue Denies : Lightheadedness, Weight gain Dizziness Headaches Blurry vision Abdominal pain Changes in bowel habits Rashes Vital signs At initial presentation to UH: Temp 98.6° F BP 155/88 mmHg HR 61/min RR 12/min BMI 51; Ht 5’2 Weight 283lbs Physical Exam General: Alert & oriented, NAD HEENT: NC/AT, EOMI, PERRLA, Sclera nonicteric, oropharynx clear with no exudates Neck: FROM; No cervical LAD appreciated CVS: RRR, No murmurs/S3/S4, JVP 12 Chest: CTA bilaterally, No crackles /wheezes/rhonchi Physical Exam Abdomen: Nondistended, normoactive bowel sounds; soft, nontender, No organomegaly or masses appreciated Ext: Bilateral pitting edema extending to upper thigh/lower back;2+ peripheral pulses Skin: No rashes Neuro: Cranial nerves II-XII intact Motor strength 5/5 Reflexes 2+ B/L upper and lower extremities Labs: WBC 6.4 Hg/Hct 13.7/40.0 Platelets 236 MCV 83 RDW 14.6 N52 % L 27 % M16 % E6% B0% Na 142 K 4.8 Cl 108 CO2 27 BUN 53 (7-25) Cr 7.10 (0.7-1.4) Glucose 92 Ca 8.2 Phos 6.2 GFR 11 (>60) Labs continued… Total protein 6.1 UA: Protein 500 (neg), Albumin 2.4 (3.4-5.0) Bilirubin 0.5 AST 31 ALP 82 ALT 19 0-2 WBC/RBC, 2-20 squam , rare bacteria Hyaline casts BNP 221 (<100) PT 10.1 INR 0.9 PTT 28.6 CXR Renal Ultrasound Right kidney 12.8 x 6.2 6.3 Left Kidney 1 x 6.9 x 6.6 No hydronephrosis Increased echogenicity of cortex consistent with medical renal disease Hospital course cont…. Urine studies FENA 2.6% FEUrea 47.6% Spun urine: No casts or significant sediment Urine Culture: No growth Urine Eos present Total protein 25943 mg/24hr (<100) Total protein/Creatinine ratio 12910 mg/g (<200) Hospital course cont…. Other significant lab values HIV nonreactive RPR nonreactive Acute Hep panel: Hep B Surface Ag + C3 111; C4 22 ESR 55 (0-15) Rheumatoid Factor 162 (normal <20) Total cholesterol 190 Triglycerides 44 HDL 54 LDL 127 ANA negative Anti-DS DNA negative LDH 289 (<201) CK 371 (<231) SPEP: Hypoalbuminemia and increased fraction of alpha 2 consistent with Nephrotic syndrome iPTH 296 (12-65); Calcium 8.2 25-OH Vit D 5.1 (32-100) Follow-Up Patient discharged 5/15/12 with diagnosis of nephrotic syndrome and Hepatitis B infection BUN 50; Cr 6.72; GFR 11 Discharge meds: furosemide, carvedilol, amlodipine, atorvastatin, sevelamer No clear risk factors for Hepatitis B Hepatitis E Ag and Ab, HBV viral load Renal biopsy pathology pending at time of discharge After Discharge…. Renal biopsy performed 5/14/12 Diffuse foot process effacement with microvillus transformation and vacuolization. Unremarkable mesangial matrix and no deposits identified. Consistent with minimal change disease Normal glomerulus Light micrograph of an essentially normal glomerulus in minimal change disease. Follow up Patient seen in Nephrology clinic BUN 53; Cr 70.1; GFR 11 Hep B E Ag negative Hep B E Ag AB positive HBV viral load 3317 Oral prednisone 60mg daily started GI referral for hepatitis B management Follow up GI clinic 6/1/12 Chronic Hepatitis B carrier state Initiation of tenofovir renally dosed Monitoring with repeat labs at 2 and 6 months with repeat ultrasound at 6 months Currently Final Renal biopsy path report: Minimal Change Weight 250 lbs BUN 32; CR 1.45 Total protein/Creat 3148 Tapering prednisone based on renal function and proteinuria Requiring less fursoemide Tenofovir daily THANK YOU