PatientHistory
advertisement
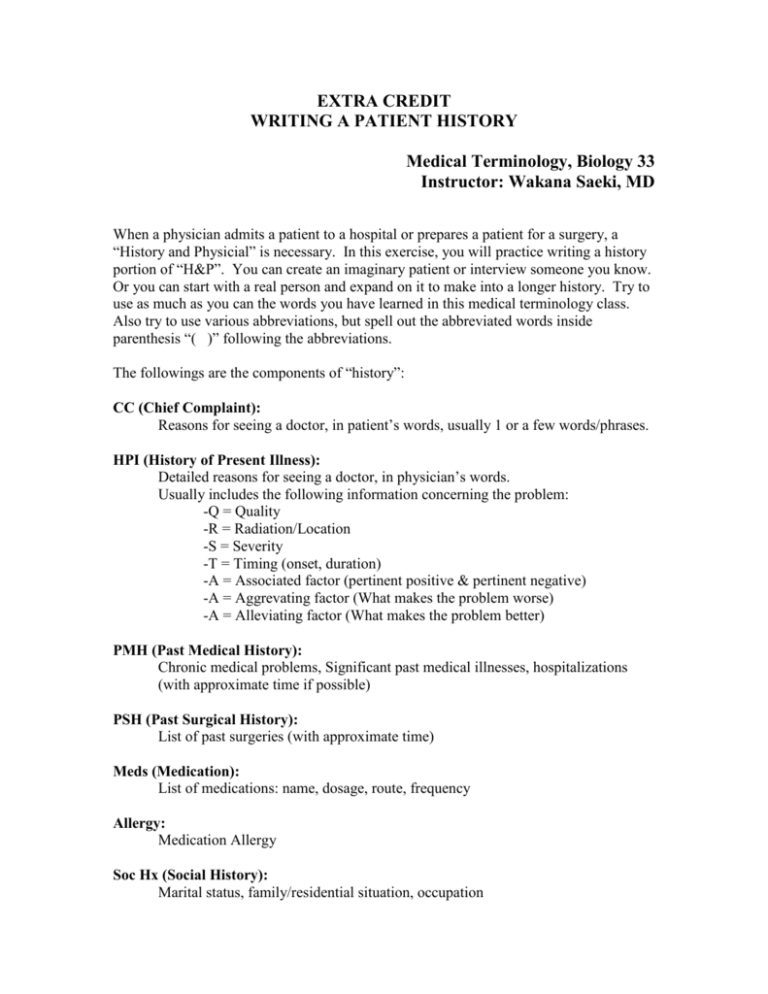
EXTRA CREDIT WRITING A PATIENT HISTORY Medical Terminology, Biology 33 Instructor: Wakana Saeki, MD When a physician admits a patient to a hospital or prepares a patient for a surgery, a “History and Physicial” is necessary. In this exercise, you will practice writing a history portion of “H&P”. You can create an imaginary patient or interview someone you know. Or you can start with a real person and expand on it to make into a longer history. Try to use as much as you can the words you have learned in this medical terminology class. Also try to use various abbreviations, but spell out the abbreviated words inside parenthesis “( )” following the abbreviations. The followings are the components of “history”: CC (Chief Complaint): Reasons for seeing a doctor, in patient’s words, usually 1 or a few words/phrases. HPI (History of Present Illness): Detailed reasons for seeing a doctor, in physician’s words. Usually includes the following information concerning the problem: -Q = Quality -R = Radiation/Location -S = Severity -T = Timing (onset, duration) -A = Associated factor (pertinent positive & pertinent negative) -A = Aggrevating factor (What makes the problem worse) -A = Alleviating factor (What makes the problem better) PMH (Past Medical History): Chronic medical problems, Significant past medical illnesses, hospitalizations (with approximate time if possible) PSH (Past Surgical History): List of past surgeries (with approximate time) Meds (Medication): List of medications: name, dosage, route, frequency Allergy: Medication Allergy Soc Hx (Social History): Marital status, family/residential situation, occupation Fam Hx (Family History): Medical problems of each family member, including but not limited to: cancer, diabetes, hypertension, heart disease, etc. ROS (Review of System): -General -HEENT (Head, ears, eyes, nose, throat) -Respiratory -Cardiovascular -Abdominal -Gynecological -Genitourianry -Musculoskeletal -Endocrinological -Hematological -Neurological SAMPLE HISTORY CC (Chief Complaint): Stomach pain HPI (History of Present Illness): Jane Smith is a 45 yo (year old) female, who presented to ER (emergency room) with 3 days hx (history) of abdominal pain. Pain is described as “crampy”. Pain is located in epigastric and RUQ (right upper quadrant), and radiates to mid back. Jane rated her pain to be 8 out of 10 on a scale of 0 (no pain) to 10 (most severe pain). Pain started 3 days ago, and gradually worsened. The pain comes intermittently about 3-4 times a day. The pain lasts 3-4 hours each time. She also becomes nauseated when she has this pain. She vomited x3 yesterday. She denies diarrhea or blood in stool. The pain is worse post-prandial, especially after eating fatty or spicy food. Pain was improved with Tylenol initially, but now nothing helps the pain. PMH (Past Medical History): Pneumonia 1990 hospitalized for 3 days Asthma since childhood PSH (Past Surgical History): 1965 Tonsillectomy and adenoidectomy 1970 Appendectomy 1987 and 1990 C-section (Cesarean section) 1997 R (right) Salpingectomy for ectopic pregnancy 2000 TAH (Total abdominal hysterectomy) for menometrorrhagia Meds (Medication): Tylenol ES (extra strength) 500mg 2 tabs (tablets) PO (per os = by mouth) q 8 hrs (every 8 hours) prn (as needed for) pain Albuterol MDI (Meter dosed inhaler) 2 puffs q 4hrs (every 4 hours) prn (as needed for) SOB (Shortness of breath) and wheezing Allergy: PCN (Penicillin) Soc Hx (Social History): Married. Lives with her husband and 2 children. She is a school teacher, teaching 5th grade Fam Hx (Family History): Mother: HTN (Hypertension) Father: Hypercholesterolemia Paternal Grandfather: Prostate CA (cancer), died of CVA (cerebral vascular accident) Maternal Grandmother: CAD (coronary artery disease), CHF (congestive heart failure), adult onset DM (diabetes mellitus) Sister: s/p (status post) cholecystectomy for cholelithiasis/cholecystitis Brother: s/p MI (Myocardial infarction = heart attack) ROS (Review of System): -General: No fever or chills, +5 lbs weight loss in the last 3 days. -HEENT (Head, ears, eyes, nose, throat): No change in vision, no ear pain, no runny nose, no sore throat -Respiratory: has asthma attack with wheezing and SOB (shortness of breath) about once every 3 months. Currently denies dyspnea or cough -Cardiovascular: Denies chest pain or palpitation -Abdominal: see HPI (history of present illness) -Gynecological: LMP (last menstrual period) 2000 due to hysterectomy. G3P2Sab1 (Gravida 3 Parity 2 Spontaneous abortion 1) -Genitourianry: No dysuria, hematuria, or increase in urinary frequency -Musculoskeletal: no myalgia or arthralgia -Endocrinological: No polyuria, polydipsia, no heat or cold intolerance -Hematological: no abnormal bleeding or easy bruising -Neurological: no LOC (loss of consciousness), no weakness, no paresthesia