Microbiology Lab Manual
advertisement

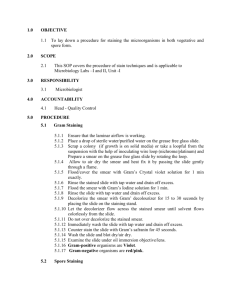
LIST OF EXPERIMENTS S. No. CONTENTS Page No MICROBIOLOGY 1. Laboratory rules and regulation 14 2. Preparation and cleaning of glass wares 15 3. Sterilization Techniques 17 4. Preparation of culture media- Nutrient agar 20 5. Preparation of culture media – Nutrient broth 21 6. Pour Plate technique 22 7. Spread Plate technique 23 8. Streak Plate technique 24 9. Smear Preparation 25 10. Simple Staining 26 11. Gram’s Staining 27 12. 13. Motility of bacterial cell Antibiotic sensitivity test 1. LABORATORY RULES AND REGULATIONS There are some rules and regulation which must be observed for the successful completion of the laboratory exercise for the safely and convenience of the others working in the laboratory. 1. Always wear a lab coat before entering a laboratory for protecting cloths from accidental discoloration by staining solutions. 2. Before and after each laboratory period clean the work bench with disinfectant like Lysol, phenol or 90% ethanol. 3. Keep laboratory bench clean off everything (like pencil, book and paper) except laboratory period. 4. Never eat or drink inside the laboratory. 5. If a live culture spilled, cover the area with a disinfectant such as mercuric chloride for 15 min and then clean it. 6. Never place pencil, label or any material in your mouth. 7. In the event of personal injury such as cuts or burns inform your instructor immediately, since bacteria enter through open injury. 8. Long hair should be tied back to minimize contamination by culture and fire hazards. 9. Be careful of laboratory burner and turn off when not in use. 10. All the microbial culture should be handled as potential pathogens. 11. The waste paper and contaminated glass wares should be kept in places provided. 12. Wash your hands with detol soap and water before leaving the lab. 13. Broth culture should never be mouth pipette. 14. Aseptic technique must be seriously observed at all the times. 15. Always keep culture tubes in an upright position in each the rack or basket. 16. Label all the plates, tubes culture properly before starting the exercise in sequence. 17. Keep the lab window and door closed when the experiment is in progress. 18. As you perform the exercise, record your data in ink and mark sketches and tables in pencil. 19. Keep your lab notebook up to date. 2. PREPARATION AND CLEANING OF GLASSWARES Glass wares used in laboratories have to be properly cleaned, washed and sterilized before and after use. Improper cleaning and sterilization may interfere with results and may cause contamination. Newly purchased glass wares also have to be cleaned and washed properly as they may be the source of chemical or microbial contamination Before sterilization and after use, glass wares like petri plates, conical flasks and test tubes have to be washed using the following procedures NEW GLASS WARES: New glass wares require special attention because of the resistant spores present in straw and other packaging materials. These materials may give out some alkali which is sufficient to interfere with the growth of certain organisms. Therefore it should be placed in 1% HCl for overnight then washed with tap water followed by distilled water and autoclaved. Screw capped tubes are subjected to a special cleaning process till the surface alkali is removed. The tubes may be used without further treatment as received from the manufactures. CLEANING OF GLASSWARE FOR LABORATORY USE: All contaminated glassware should be autoclaved before cleaning. If this is not possible, glass containers with discarded culture can be replaced in 3% Lysol or simple disinfectant after use. Glass containers contaminated with spore bearing organisms must be autoclaved. The discarded spores must be placed in a hot detergent solution. The containers placed in hot detergent solution / treated as recommended by manufacture / finally rinsed in de-ionised water. The glass ware is then dried in hot air oven at 100 ºC for 3 hrs. CLEANING OF GLASS WARE FOR BIOCHEMICAL WORKS: Remove any grease with petroleum then wash with water. Then place the glassware in chromic acid solution for 24 hrs after that wash with distilled water and then dry in hot air oven at 100 ºC for 3 hrs. CHROMIC ACID CLEANING SOLUTION: Dissolve 63gms of potassium dichromate by heating with 35ml of water, cooled and add Conc. Sulphuric acid and make upto one liter. This fluid should be handled with care. Rubber gloves and apron should be worn. CLEANING OF PIPETTES: Place the contaminated pipette in a 3% Lysol solution. The Lysol solution should be placed in a plastic container about 40cm in height and 10cm in diameter, the tips of the pipette should be broken and then it is rinsed with tap water, if necessary they can be placed in a detergent solution of chromic acid solution. Then wash with water followed by de-ionized water. To neutralize pipettes, place them in an aluminum pipette cane and keep it in a hot air oven at 160 ºC for 3 hrs. NOTE: Accurately, calibrated volumetric glass wares should never be heated in an oven, since the expansion and contraction makes the graduation inaccurate. 3. STERILIZATION TECHNIQUES Sterilization is the process which elimination of living organisms including spores from treated substances or any objects. This can be accomplished by moist heat, dry heat and open flame sterilization. MOIST HEAT STERILIZATION Autoclave is a device used in the laboratory for moist heat sterilization. It is normally operated at 15 lbs/ square inch steam pressure for 15 min. and thus produced a temperature inside the autoclave of 121ºC (250 ºF). Sterilization in an autoclave is done with saturated steam under pressure. Saturated steam is the water vapour at the temperature at which it is produced. Autoclave is a double walled cylindrical metallic vessel, made of thick stainless steel or copper, one end of which is open to receive the material to be sterilized. Autoclave lid is provided with pressure gauge for noting the pressure, steam cock (exhaust valve) for air exhaustion of the chamber. Autoclave is provided with controls for adjusting the pressure and temperature and a safety valve to avoid explosions. The articles to be sterilization are kept loosely in a basket, provided with roles all around for the free circulation of steam. To increase the area of materials to be sterilized, metallic separators having holes can be used. USES This is the most efficient and common instrument used for sterilizing solid and liquid media for microbial cultures, heat stable liquids- usually the common media ingredients, heat resistant instruments and equipments, glass wares and rubber products. Scalpels and other sharp metal instruments are damaged by constant flaming and are usually sterilized by autoclaving. DRY HEAT STERILIZATION Hot air oven is based in the principle where sterilization is accomplished by dry heat or hot air. Sterilization is accomplished by exposure of item to 150-180 ºC for 2-4 hrs. This consists of an insulated cabinet which is held at a constant temperature by means of an electric heating mechanism and thermostat. It is fitted with a fan to keep the hot air circulating at a constant temperature and thermometer for recording the temperature. For proper circulation of the hot air, the shelves are perforated. For normal sterilization work, the oven should be operated at 160 ºC and most glass wares will require a period of two hrs for complete sterilization. The schedule of time and temperature for sterilization with dry air Temp (ºC) 120 140 150 160 170 180 Time(min) 480 180 150 120 60 20 USES Commonly used for sterilizing glass wares like petridishes, test tubes, pipettes, metal instruments that can tolerate prolonged heat exposure, oils, powder, waxes and other articles that are either spoiled or not effectively sterilized by the moist heat of the autoclave. OPEN FLAME STERILIZATION: Contaminated materials that are combustible may be disposed off by burning. The inoculation needle or loops and flaming the tips of the tubes and conical flasks are directly heated in an open flame or Bunsen burner or an alcoholic lamp. LAMINAR-FLOW HOOD: This equipment used for reducing the danger of infection while manipulating infectious microorganisms and for preventing contamination of sterile materials. In a closed room where handling of microorganisms, like transfer and inoculation are done constantly and in operation involving lyophilization and opening of lyophilized culture, large amount of floating microbial cells and aerosol may be produced. Radiation and other treatments may not be effective always in keeping such room free of particles and droplets containing microorganisms. To keep such room free of all microbes carrying particles, a new kind of technology has been developed known as laminar air-flow technique. This technique involves passing the air of a closed room of cabinet through high efficiency particulate air (HEPA) filters pack. When air thus passes through, becomes free of all particles above 0.3µm dimension. This also involves sucking of air from the room and blowing out the air through a back of filters with uniform velocity and in parallel flow line. Both horizontal and vertical laminar air –flow systems are now used in microbiological and pharmaceutical laboratories. Hospital rooms are now designed with laminar air-flow system. The advantage of the system is that in operation involving inoculation, transfer of culture and opening of lyophilized culture no closed chamber is necessary. Instead the operation can be done on platform provided with the laminar air flow unit making it easier for handling. USES: THE LAMINAR AIR FLOW (a) Separates contaminants from the interior space by creating a curtain of filtered air across the front opening. The worker has complete access to the materials inside the hood. Air is circulated through filters. (b) Before it for exhausted, laminar air-flow hoods are standard equipments in tissue culture laboratories and are required for contaminant of genetically engineered microorganisms. Room air is filtered before entering the working chamber and moves in a single direction. Contaminated air from the chamber is filtered again before being either re-circulated in the system or exhausted to the outside. 4. PREPARATION OF CULTURE MEDIA – NUTRIENT AGAR AIM: To prepare the nutrient agar medium for bacterial growth. REQUIREMENTS: i. 250ml conical flask ii. Distilled water iii. pH meter iv. Electronic balance v. Non- absorbent cotton. MEDIUM COMPOSITION (G/100ML): a. Yeast extract (1g) b. Peptone (1g) c. NaCl (0.5g) d. Agar (2g) e. Distilled Water(100ml) PROCEDURE: 1. A clean glass conical flask was taken with 100ml distilled water. 2. The medium components were weighed accurately and dissolved one by one in distilled water. (Care was taken to see that the chemical was added to distilled water only if the pervious chemical was dissolved completely). 3. The pH was adjusted to 7.2 using 1N NaOH solution. 4. The mouth of the flask was then plugged with non-absorbent cotton, and then it was covered with brown paper then tied with a thread tightly. 5. The flask was then autoclaved at 121ºC for 15 min. RESULT: Nutrient agar plate was prepared for the cultivation of bacteria. 5. PREPARATION OF CULTURE MEDIA – NUTRIENT BROTH AIM: To prepare the nutrient broth medium for bacterial growth. REQUIREMENTS: i. 250ml conical flask ii. Distilled water iii. pH meter iv. Electronic balance v. Non- absorbent cotton. MEDIUM COMPOSITION (G/100ML): a. Yeast extract (1g) b. Peptone (1g) c. NaCl (0.5g) d. Distilled Water(100ml) PROCEDURE: 1. A clean glass conical flask was taken with 100ml distilled water. 2. The medium components were weighed accurately and dissolved one by one in distilled water. (Care must be taken to see that to see that the next chemical was added to distilled water only if the previous chemical added was dissolved completely). 3. The pH was adjusted to 7.2 using 1N NaOH solution. 4. The mouth of the flask was then plugged with non-absorbent cotton, and then it was covered with brown paper then tied with a thread tightly. 5. The flask was then autoclaved at 121ºC for 15 min. RESULT: Nutrient broth culture media was prepared for the cultivation of bacteria. 6. POUR PLATE TECNIQUE By pour plate technique, individual colonies can be observed throughout the nutrient agar medium. The colonies will be of different size, shape and color. From the individual colony, pure colonies can be isolated. MATERIAL REQUIRED: Test tubes, pipettes, sterile distilled water, Bunsen burner, test sample etc. MEDIA USED: Nutrient agar medium PROCEDURE: 1. 1ml of the liquid sample was transferred into the test tube which contains 9ml of distilled water blank. Here the dilution is 10-1 and this has to be mixed properly. 2. Using a sterile pipette, 1ml from 10-1 dilution was transferred to the next test tube which contains 9 ml distilled water (10-2) 3. Subsequent dilutions were made up to 10-5 4. Then 1ml of each dilution was transferred to each sterile Petri plates. 5. Then the molten nutrient agar was poured into the plates and was rotated gently to ensure a uniform distribution of cells in the medium. 6. The step 5 was repeated for each dilution. 7. Then the media was allowed to solidify. 8. After solidification, the plates were incubated for 18 - 24 hrs at optimum temperature in an inverted position. CALCULATION: CFU = RESULT: Total Number of organism present is a given sample = _________________ cfu/ml 7. SPREAD PLATE TECHNIQUE This is another method, which is also used for the isolation of individual colonies. In this technique, microorganisms are spreaded over the solidified agar medium with a sterile L-shaped glass rod while the pertidrsh is spun on a turn table. The principle is, as the petridish spuns, at some stage single cells will be deposited with the bent glass rod on the agar surface. Some of these cells will be separated from each other by a distance sufficient to allow the colonies that develop to be free from each other. MATERIAL REQUIRED: Nutrient agar medium L rod, tubes, petriplates, distilled water etc. PROCEDURE: 1. 9ml of distilled water was taken in different test tubes and was sterilized. 2. After sterilization, 1ml of the sample was added to the first tube(101 ) 3. From the above, 1ml of diluent was taken and added to the second test tube (10-2). In this method all the test tubes were serially diluted. 4. About 0.1ml of sample was taken from each dilution and applied to the surface of nutrient agar plate and spreaded uniformly by using sterile ‘L’ rod. 5. After inoculation, the petriplates were incubated at optimum temperature for 24hrs in an inverted position. CALCULATION: CFU = RESULT: Total Number of organism present is a given sample = _________________ cfu/ml 8. STREAK PLATE TECHNIQUE The streak plate method is a qualitative isolation method. If a microbial culture is applied to the surface of agar in a petriplate and spreaded with a loop or a bent needle it is called streaking and the plate thus prepared is called as streak plate. Ther streaking ‘thins out’ the bacteria on the agar surface so that the individual bacteria are separated from each other. The streak plate technique can be done by the following methods. i. ii. Phase Streaking Continuous streak MATERIALS REQUIRED: Plates with sterile agar medium, inoculation needle, etc. PREPARATION OF AGAR PLATES FOR STREAKING: About 15-20ml of melted sterile nutrient agar medium was allowed to solidify. A. PHASE STREAKING: 1. A loop full of organisms was taken in the inoculation needle and spreaded evenly on a small area of the agar plate. 2. Then three or four parallel streaks were made. 3. The inoculation needle was then sterilized and 3 or 4 streaks were again made at right angles from that of the first streak. 4. The loop was flamed again and the step 3 was again repeated. 5. Then the streaked plates were incubated in an inverted position at optimum temperature for 24 hrs. B. CONTINUOUS STREAKING: A part of the inoculums was taken in the inoculation loop and spreaded well on the agar plate and the streak was done in one continuous motion. The plates were then incubated at optimum temperature for 18-24 hrs in an inverted position. RESULT: Isolated observed on final Isolated colonies maintain as a colonies were streak path area. were selected and pure culture. 9. SMEAR PREPARATION The preparation of a smear is required for many laboratory procedures, including the Gram-stain. The purpose of making a smear is to fix the bacteria onto the slide and to prevent the sample from being lost during a staining procedure. A smear can be prepared from a solid or broth medium. Below are some guidelines for preparing a smear for a Gram-stain. 1. Place one needle of solid bacterial growth or two loops of bacterial growth in the center of a clean slide. 2. If working from a solid medium, add one drop (and only one drop) of water to your specimen with a water bottle. If using a broth medium, do not add the water. 3. Now, with your inoculating loop, mix the specimen with the water completely and spread the mixture out to cover about half of the total slide area. 4. Place the slide on a slide warmer and wait for it to dry. The smear is now ready for the staining procedure. RESULT: Thin bacterial smear was prepared for staining. SIMPLE STAINING AIM: To elucidate morphological shapes and arrangements of bacterial cells by using simple stain technique. PRINCIPLE: In simple staining, the bacterial smear is stained with a single reagent. Basic stains with a positively charged are used because the bacterial nucleic acids and certain cell wall components carry negative charge that strongly attracts and bind to the cationic chromogen. The commonly used basic stains are methylene blue, crystal violet and carbol fuchsin. MATERIALS REQUIRED: Bacterial sample, Methylene blue stain, Microscope slides, inoculation loop, Bunsen burner etc. PROCEDURE: 1. By means of a sterile inoculation loop, a drop of the bacterial suspension was transferred to the center of the slide. 2. The drop over the slide was spreaded to about 1sq.inch as a thin film and allowed to air dry. 3. Then the smear was fixed by passing the slides rapidly over the flame. 4. The smear was then flooded with several drops of methylene blue and allowed to remain for 1-2 min. 5. The slide was washed after 2 min in a gentle stream of water to remove the excess of stain and the slide was air dried. 6. Then the slide was examined under oil immersion microscope. Simple Staining RESULT: The bacterial cells stains blue and the cells were in ______________ Shape and are referred as ____________________ 10. GRAM’S STAINING AIM: To differentiate the two principal groups of bacteria ie. Gram positive and gram negative on the basis of the gram stain. PRINCIPLE: Most bacteria can be differentiated by the gram reactions due to difference in their cell wall structure. GRAM POSITIVE BACTERIA Cell wall has a large amount of peptidoglycan. GRAM NEGATIVE BACTERIA They have less amount of peptidoglycan in their cell wall. They have lipopolysaccharide containing a compound known as lipid A or endotoxin.The organisms that retain purple color with crystal violet and are not decolorized by acetone iodine are called gram positive bacteria.The organisms that loose their color of crystal violet after being treated with acetone iodine are called gram negative bacteria. Differential staining requires the use of atleast three chemical agents that are applied sequentially to the heat fixed smear. The first reagent used is called the primary stain. Its function is to impart its color to all the cells. When iodine solution is applied, it replaces the chloride in the crystal violet molecule and a complex is formed which becomes insoluble in water. This complex is formed in both the gram negative cells. This is due to the difference in the composition of the cell wall. The gram positive cell wall having a lower lipid content becomes dehydrate, making the pore size small and thus not allowing the get dehydrated and thus the pore size remaining the same allows the complex to leak out on applying the counter stain, the cells that have last the primary stain appearing pink. The gram positive cells that retain the primary stain colour appears violet. MATERIALS REQUIRED: Bacterial Sample, Microscopic slide, Microscope, inoculation loop, blotting paper, spirit lamp etc. REAGENTS: a. Crystal violet b. Grams iodine c. 95% ethyl alcohol d. Safranin PROCEDURE: 1. The smear of the organisms was made in a clean glass slide, an dried and then it was heat fixed. 2. The fixed smear was covered with crystal violet stain for 30-60 seconds. 3. Then the stain was rapidly washed off with distilled water 4. Again the smear was covered with gram’s iodine solution for 30-60 seconds. 5. Using the distilled water, the iodine was washed off. 6. The smear was then decolorized rapidly with 95% alcohol and washed immediately with distilled water. 7. The smear was again covered with safranin for 1 min. 8. The above stain was washed off with distilled water. 9. The slide was then allowed to air dry. OBSERVATION: The smear was examined microscopically with 40x and 100x objective for morphology and arrangement of cells and microphotograph was made. RESULT: The bacteria appeared _________________ color, ________________ shape and are referred as________________________. 12.MOTILITY TEST- HANGING DROP SLIDE AIM: To gain expertise in determining the motility of living bacteria. PRINCIPLE: Most motile bacteria move by use of flagella, thread like locomotor appendages extending outward from the plasma membrane and cell wall. Motile cells may have one flagellum, but most have several. Each flagellum has a very rigid, helical structure and actual motility results from the rotation of the flagellum in a manner similar to that of a boat propeller. Motility by means of flagella is particularly important for the identification of microorganisms, for instance Bacilli are motile except for the anthrax, which is instead capsular, therefore flagella could be produced to enable the organisms to run away from danger and to move from less favorable to more favorable environment. Materials Required : Clean depression slides and coverslips Petroleum jelly / Vaseline Inoculating loop Toothpicks Cultures:- 24- to 48-hour Nutrient broth cultures of Pseudomonas aeruginosa Procedure: 1. With a toothpick, spread Vaseline or Petroleum jelly on the four corner of a clean coverslip. 2. After thoroughly mixing one of the cultures, use the inoculating loop to aseptically place a small drop of the bacterial suspension in the center of a coverslip 3. Lower the depression slide, with the concavity facing down, onto the coverslip so that the drop protrudes into the center of the concavity of the slide .Press gently to form a seal. 4. Turn the hanging drop slide over and place on the stage of the microscope so that the drop is over the light hole. Examine the drop by first locating its edge under low power and focusing on the drop. Switch to the high-dry objective (40 x). To increase the contrast and to see the bacteria clearly, close the diaphragm as much as possible. 5. Distinguish between actual motility and Brownian movement 6. Discard the coverslips and any contaminated slides in a container with disinfectant solution. Hints: 1. Always examine a hanging drop preparation immediately, because the organisms become less motile with time. 2. Particular care must be taken to avoid breaking the coverslip since it is more vulnerable when supported only around its edges 3. Always make sure the specimen is on the top side of the slide. Expected Results: Actively motile organisms (Pseudomonas aeruginosa) were observed OBSERVATION: The smear was examined microscopically with 40x and 100x objective for morphology and arrangement of cells and microphotograph was made. RESULT: Actively motile organisms organism name were observed