Brainstem perfusion impaired in chronic fatigue syndrome
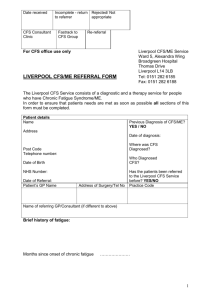
advertisement

This document has been scanned by OCR (Optical Character Recognition) and may therefore contain inaccuracies due to character recognition errors. Quarterly Journal of Medicine December 1995:88:767-773 Brainstem perfusion is impaired in chronic fatigue syndrome D.C. COSTA, C. TANNOCK1 and J. BROSTOFF2 From the Institute of Nuclear Medicine, 1 Department of Psychiatry and 2 Department of Immunology, UCL Medical School, London, UK Address: respondence to Dr D.C. Costa, Institute of Nuclear Medicine, UCL Medical School, UCL Hospitals, Mortimer Street London WTN BAA Oxford University Press 1995 Received 12 April 1995; Accepted 29 June 1995 Summary “““““““““““““ We looked for brain perfusion abnormalities in patients with myalgic, encephalomyelitis/chronic fatigue syndrome (ME/CFS). An initial pilot study revealed widespread reduction of regional brain perfusion in 24 ME/CFS patients, compared with 24 normal volunteers. Hypoperfusion of the brainstem (0.72±0.05 vs. 0.80±0.04, p<0.0001) was marked and constant. We then tested whether perfusion to the brainstem in ME/CFS patients differs from that in normals, patients with major depression, and others with epilepsy. Data from a total of 146 subjects were included in the present study: 40 normal volunteers, 67 patients with ME/CFS (24 in the pilot study, 16 with no psychiatric disorders, 13 with ME/CFS and depression, 14 with ME/CFS and other psychiatric disorders), 10 epileptics, 20 young depressed patients and 9 elderly depressed individuals. Brain perfusion ratios were calculated using 99Tcm-hexamethylpropylene amine oxime (99Tcm-HMPAO) and single-photon emission tomography (SPET) with a dedicated three-detector gamma camera computer/system (GE Neurocam). Brain-stem hypoperfusion was confirmed in all ME/CFS. Furthermore the 16 ME/CFS patients with no psychiatric disorders and the initial 24 patients in the pilot study showed significantly lower brainstem perfusion (0.71±0.03) than did depressed patients (0.77±0.03; ANOVA, p<0.0001). Patients with ME/CFS have a generalized reduction of brain perfusion, with a particular pattern of hypoperfusion of the brainstem. Introduction “““““““““““““““ There is no universally replicable identifiable organic cause to explain the symptoms and signs presented by patients with myalgic encephalomyelitis, also called chronic fatigue syndrome (ME/CFS). Indeed, amongst neurologists and psychiatrists, there is some reluctance to accept this disease as an independent syndrome. Depression is often considered the main explanation for ME/CFS patients’ symptoms. Myalgic encephalomyelitis is now a major cause of absenteeism. All patients complain of a significant lack of concentration and extreme fatigue which can be disabling to the point of reducing them to a wheelchair, career disadvantage and often job loss. The discrepancy between patients’ symptoms and objective findings on physical and neuropsychiatric examination has given rise to long debates in general1 and in the peer-reviewed literature.2-4 Another complication is the multiplicity of names given to this intriguing disorder, namely chronic fatigue syndrome (CFS), myalgic encephalomyelitis (ME), postviral fatigue syndrome (PVFS) and chronic fatigue and immune dysfunction syndrome (CFIDS). All of these seem to embody an assumption that a viral infection and possible immune dysfunction are responsible for the patients’ weakness and fatigue.2 Whilst the search for a possible causative agent (some kind of known or unknown virus) continues, the social impact of the disease has gained the attention of health carers. The Centers for Disease Control (CDC) is taking the disease seriously and has funded a nationwide (USA) prevalence survey with part of the $2.8m that Congress put in the agency’s budget for 1992.3 The resulting study by Gunn et al.5 showed that the prevalence of the disease, excluding previous psychiatric diagnosis, was 4.6-11.6 per 100.000. 5 In the UK, the ME Association claimed in 1989.6 that there were 150.000 patients with myalgic encephalomyelitis, whilst Behan et al. had suggested a prevalence of 3 cases per 100.000 of the general population who would show classic symptoms, changes in appetite, fluid retention, excessive sweating, hot flushes, sleep abnormalities, poor memory and difficulty in concentrating.8 Although all patients present with distinctive clinical features, so far no single causative agent has been identified. However, neuropsychiatric manifestations of the disease include impairment of short-term memory, loss of concentration, excessive irritability, nominal dysphasia, hypersomnia, insomnia, recurrent vertigo and/or tinnitus. Their nature and severity raises the possibility of an organic component in the evolution of ME/CFS. To investigate this organic component, we designed a comparative and quantitative study of the resting brain perfusion between patients with ME/CFS, age-matched normal volunteers and other patients with major depression. Methods “““““““““““ Study population “““““““““““““““““““““ A total of 146 individuals were included in this preliminary study. The two groups of the initial pilot study were composed of 24 ME/CFS patients (11 males, 13 females) aged 12 - 52 years (mean ± SD 36 ± 13) and 24 normal volunteers (13 males, 11 females) aged 21- 59 years (mean ± SD 31 ± 10). In addition, the brain perfusion of nine elderly depressed patients (four males, five females) aged 69 - 89 years (mean ± SD 79 ± 8) and ten young epileptics (five males, five females) aged 18-33 years (mean ± SD 31 + 5) was used for comparison. A further 43 newly recruited ME/CFS patients (14 males, 29 females) aged 19-76 years were given psychiatric tests to subdivide them into three distinct groups: 16 patients with no other psychiatric disorder in their past or present history (ME-CFS), 13 patients with a past or present history of major depression (ME + DEP), and 14 patients with other associated psychiatric disorders including dysthymia, anxiety and somatization disorders (ME + OD). In addition, a further 16 normal volunteers (11 males, 5 females; 24-52 years old) and 20 patients with major depression (8 males, 12 females; 18-52 years old) diagnosed according to DSM III-R criteria,9 using the Structured Clinical Interview for DSM III-R Patient Version (SCID-P)10 and graded for severity with the Hamilton Depression rating scale,11 to include those with moderate to severe depression, were included in this study. All ME/CFS patients were clinically assessed diagnosed according to standard criteria (Oxford.12*, CDC.13* and ME Action.14*). The following exclusion criteria were applied: (i) clinical conditions known to produce chronic fatigue, e.g. anaemia, acute or chronic infections of known aetiology, thyroid dysfunction, diabetes mellitus and chronically debilitating diseases (oncological or others); (ii) neuropsychiatric diseases, particularly schizophrenia, manic-depressive illness, drug abuse, eating disorders and proven organic CMS disease. This study was approved by the Ethical and Radiation Protection (ARSAC) committees. All the normal volunteers, epileptic and elderly depressed patients were enrolled in other studies, for which Ethical and Radiation Protection authorisation had been obtained. They were not specifically recruited for the present study. Data acquisition and processing “““““““““““““““““““““““““““““““““““““““““““ Brain perfusion studies of all subjects were done 10-30 min after injection of a mean 550 MBq, of 99Tcm-hexamethylpropyleneamine oxime (99Tcm-HMPAO), using a brain-dedicated triple-detector gamma camera (GE Neurocam). Data acquisition was according to a routine protocol previously described.15,16 High-resolution collimators were used, and total mean acquisition time was 28 min, with the subjects lying still on a comfortable couch. Data processing followed previously published protocols15,17,18 and included attenuation correction according to the Chang method, applying a coefficient of 0.12 cm-1. Data was processed by a STAR 3000 computer with software supplied by the manufacturer, General Electric. A set of horizontal (axial) slices were reconstructed using a backprojection algorithm. From these, sagittal slices were obtained and the horizontal slices were reorientated to produce a uniform display. This was attained by drawing a line parallel to the most inferior frontal and occipital cortices, approximately parallel to the anterior commissure-posterior commissure line (AC-PC line), to obtain transverse slices. Finally, coronal slices were reconstructed using planes perpendicular to the transverse slices. Data analysis ““““““““““““““““““ Data analysis was done in two steps. First, by visual inspection (qualitative analysis) of the data available from the colour video output of the computer system by DCC. Transverse, coronal and sagittal slices were used to report on areas of decreased regional brain perfusion. Black and white and colour images, always with the same 16-step scale colour scheme, were read. The colour scheme or scale represents the distribution of radioactivity counts throughout the brain, normalized to the voxel with maximum counts per pixel (100% corresponding to 16 steps). Secondly, a quantitative analysis was applied based on the ‘regions of interest’ (ROI) method following a methodology described by Costa et al.15 Regular ROls with a volume of 2.05 cm3 were used to sample different areas of the cerebral cortex, basal ganglia, thalamus, cerebellum and brainstem (mainly the pons). At least three contiguous slices were used to obtain information from each of the brain regions studied. Two or more ROIs per slice and per hemisphere were read, and the mean count rate was used to calculate radioactivity ratios normalized to the cerebellar hemisphere exhibiting highest mean counts per pixel. To estimate radioactivity from the temporal lobes, coronal rather than transverse slices were used, for improved separation between the medial and lateral components of the temporal cortex.17 Statistical analysis “““““““““““““““““““““““““““ Data obtained from the ME/CFS patients and normal volunteers in the pilot study, as well as from elderly depressives and age matched epileptic patients were submitted to Student’s t-test analysis for unpaired comparisons. Statistical analysis was done on a Macintosh computer using StatView 4.0 software. All calculated p values are presented in Results. The same software was used to assess statistical significance of the differences in the brainstem perfusion ratios between the subgroups of ME/CFS patients, normal volunteers and control depressed patients, applying ANOVA with Bonferroni corrections. Results ““““““““““““ Visual inspection (qualitative analyses) “““““““““““““““““““““““““““““““““““““““““““““““““““ In the pilot study, all 24 ME/CFS patients had generalized reduction of the brain perfusion with a distinct brainstem hypoperfusion. In eight (33%) patients, the reduction in perfusion was considered to be severe (<10 on the 16-step colour scale). Twenty-one (88%) patients also had low perfusion (<12 on the 16-step colour scale) in the right frontal cortex and twenty-two (92% in the left frontal cortex. Low perfusion to the temporal lobes was reported in 12 (50%) patients in the right hemisphere and in 14 (58%) patients in the left hemisphere. Reduced perfusion to the parietal cortex was seen in four (17%) and six (25%) patients, respectively, in the right and left hemispheres. No perfusion abnormalities were visible in the normal volunteers. Elderly depressed, epileptic, depressed and newly recruited ME/CFS patients were not qualitatively analysed for the purpose of this study. Their data were used for quantitative analysis of the brainstem radioactivity ratios. Quantitative analysis “““““““““““““““““““““““““““““ Radioactivity ratios confirmed the visual analysis, and showed further significant differences between ME/CFS patients and normal volunteers in the pilot study. The results, expressed as means ±SD for all the brain regions studied, are shown in Table 1. The p values shown are the ones calculated with the unpaired Student’s t-test. Furthermore, analysis of Table 1 shows generalized hypoperfusion in the brain of patients with ME/CFS, with the lowest values found in the frontal cortex of both hemispheres and the brainstem. We have previously reported this brainstem hypoperfusion. and hypothesized that it might be characteristic of ME/CFS patients.19 The nine elderly depressed patients showed perfusion ratios for the brainstem (0.85±0.07) significantly (p<0.001) higher than those in the ME/CFS patients (0.72 ±0.05), and the ten age- and sex-matched epileptic patients had normal perfusion ratios for the brainstem (0.82± 0.07). The brainstem perfusion ratios of the new 43 ME/CFS patients (0.74±0.05) were significantly lower than normals (p<0.0001) and patients with major depression (p= 0.005). If we consider the entire population of 67 ME/CFS patients, the significance of the results for the brainstem perfusion ratios (0.73±0.05) is still valid (p<0.0001 vs. normals and p=0.0004 vs. major depression). The 16 ME/CFS patients, who showed no psychiatric disorder, had perfusion ratios of the brainstem (0.71 ±0.03) which were statistically different from those in the group of 40 normal volunteers (0.80 ± 0.03) and the group of 20 patients with major depression (0.77±0.03) who scored >20 on a 17-item Hamilton Depressive Rating Scale. However, they were similar to the earlier ME/CFS pilot group (not formally screened psychiatrically), as can be seen in Table 2. Brainstem perfusion ratios of patients in groups ME+DEP and ME+OD were significantly lower than those of normal volunteers but not those of depressed patients. Figure 1 shows profiles of radioactivity ratios obtained from a patient with ME/CFS (a) and a patient with depression (b), with reference to the 95% CIs (±2SD) of the normal population. Figure 2 shows brainstem perfusion in a typical normal volunteer, a typical patient with depression, and a typical patient with ME-CFS. Discussion “““““““““““““““ This study demonstrates generalized reduction in the brain perfusion ratios in patients with ME/CFS, as measured with single-photon emission tomography (SPET) and HMPAO. These patients differ from patients with major depression and some other neuropsychiatric diseases in that their brainstem is significantly hypoperfused We do not know whether these findings are the cause of these patients’ symptoms or a consequence of the disease process. Some studies which indicate that ME is a unique clinical entity20-23 are based on clinical and subjective data and on objective measurements of immune and serological markers. Other studies of cerebral perfusion in patients with ME/CFS also report extensive abnormalities in cerebral cortical perfusion in patients with this disease.24-28 Reduced perfusion ratios have been observed in the cortex of the posterior parietal,24 frontal and temporal lobes.28 None of these studies reported hypoperfusion in the brainstem. Our finding of significantly decreased brainstem perfusion may advance knowledge on the development of ME/CES. In addition to diagnostic difficulties, some ME/CFS patients have a psychiatric history of depression as well as personality abnormalities. Nonetheless, it is important to discover whether these patients’ symptoms are compatible with a diagnosis of major depression. To date, few controlled studies have used SPET or positron emission tomography (PET) to examine cerebral perfusion/ metabolism in patients with ME/CFS and those with major depression. However, glucose hypometabolism measured with PET and 18-F-fluorodeoxyglucose has been reported in ME/CFS patients compared to normals and other patients with depression.1 In a recent report, Schwartz et al.28 compared the midcerebral uptake index (MCUI) of 45 patients with CFS, 14 patients with unipolar depression and 24 patients with HIV encephalopathy of the AIDS dementia complex type. They defined MCUI as the radioactivity ratio between the average counts in a 1.5-cm slab at the thalamus and a 5-mm midcerebellar slice. The MCUI of their CFS patients was lower than that of depressed patients and healthy controls. This accords with our pilot study, but no specific investigation of brainstem perfusion was made. Brainstem hypoperfusion appears to be the differentiating factor between our MECFS patients and those with major depression. Other recent findings seem to corroborate our results. The hypothalamus of ME/CFS patients shows functional abnormalities different from those in depressed patients with upregulation of hypothalamic 5-hydroxytryptamine (5-HT) receptors, mediating the increased prolactin response to buspirone challenge, compared to healthy normal volunteers and patients with primary depression.29 Sleep disorders may occur in patients with MF/CFS,30 which may be related to abnormal physiology of the reticular formation. This contains systems concerned with activation and inhibition of sleep, consciousness and arousal, with activation and inhibition of movement, and with control of behaviour and memory via connections with the cerebral limbic system. It also includes groups of neurones which constitute repiratory and cardiovascular centres, as well as another less defined centre controlling peristaltic and other motor and secretory activities in the gastrointestinal tract. The reticular formation is an important component of the brain-stem structure, composed of midbrain, pons and medulla oblongata, and is sampled within ‘brainstem’ in brain perfusion SPET studies. Neuropathological work on animal models has shown a predilection of the herpes simplex virus for the brainstem and diencephalon,31 in particular the dorsal raphe nuclei, containing 5-HT-producing cells, and the locus ceruleus, intimately connected to the ascending reticular activating system and the regulation of sleep and levels of consciousness. Several herpes group viruses, e.g. Epstein-Barr virus and herpes virus Type 6, have been implicated in the pathogenesis of CFS.32,33 There could be a relationship between hypoperfusion of the brain, particularly the brainstem and direct neurons damage by a viral agent. This could explain some of the neurological and cognitive changes in ME/CFS. Our data indicate that ME CFS and major depression may be two distinct clinical entities with different perfusion of the brainstem. While the relationship between psychiatric disease and brainstem abnormalities is obscure, our data suggest that brainstem hypoperfusion could be due to an organic abnormality. This test of brain perfusion with SPET in patients with ME/CFS could be useful in the diagnosis of the disease and investigation of its evolution over time, especially its response to therapy. Acknowledgements “““““““““““““““““““““““““ We thank Dr Vana Douli, Dr George P. Gerasimou and Dr Svetislav Gacinovic, who helped with quantitative analysis of SPET data. This work has been partially funded by a research grant from Action for ME and Chronic Fatigue. References “““““““““““““““ 1. The CFIDS Chronicle, Spring 1991:101-110. 2. Kendell RE. Chronic fatigue, viruses, and depression. Lancet 991; 337:160-2. 3. Palca J. On the track of an elusive disease. Science 1991;. 254:1726-8. 4. Ray C. Chronic fatigue syndrome and depression: conceptual and methodological ambiguities. Psychological Medicine 1991; 21:1-9. 5. Cunn WJ, Connel DB, Randall B. Epidemiology of CFS: the CDC study. In: Kleinman A, Strauss SE, eds. Chronic Fatigue Syndrome. Chichester, Wiley, 1993; Ciba Foundation Symposium no. 173:83-101. 6. Annual Report. Myalgic Encephalomyelitis Association. Stanford le Hope Essex, ME Association, 1989. 7. Behan PO, Behan WMH, Bell EJ. The postviral fatigue syndrome- an analysis of the findings in 50 cases.J Infect 1985; 10:211-22. 8. Behan PO, Bakheit AMO. Clinical spectrum of postviral fatigue syndrome. Br Med Bull 1991; 47:793-808. 9. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (3rd edition Revised). Washington DC, 1987. 10. Spitzer RL, Williams JBW. Structured Clinical interview for DSM III-R Patient Version (SCID-P7/1/85). New York, Biometrics Research Department, Psychiatric institute; 1985. 11. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiat 1960; 23:56-62. *12. Sharpe MC, Archard LC, Banatvala JE, et al. A report chronic fatigue syndrome: guidelines for research. J Roy Soc Med 1991;84:118-21. *13. Holmes GP, Kaplan JE, Grantz NM, et al. Chronic fatigue syndrome: a working case definition. Ann Intern Med 1988; 108:378-9. *14. Criteria for a diagnosis of ME for use in the ME Action funded research. Based on the criteria suggested by W.R.C. Weir in Post Viral Fatigue Syndromes by Jenkins & Mowbray, pp 248-9. ““““““““““““““““““““““““““““““““““““““““““““““ Note: Doris M Jones MSc wrote in her message: ....Dr Weir in his chapter in the 1991 Jenkins/ Mowbray book refers to the 1988 Holmes et al criteria.... ---While Margaret Williams said in a former message: *....The Jenkins & Mowbray textbook at pp 248-249 sets out Dr Weir’s own modification of the Holmes et al 1988 criteria and makes no mention of any “London” criteria, nor of the authors of the criteria being Miss Goudsmit, Dr Macintyre and Dr Shepherd. From this, it is apparent that the “ME Action” criteria used by Costa, Tannock and Brostoff were based on criteria suggested by Dr Weir.....* ““““““““““““““““““““““““““““““““““““““““““““““““ 15. Costa DC, Eli PJ, Burns A, Philpot M, Levy R. CBF Tomograms with [99mTc]-HM-PAO In Patients with Dementia (Alzheimer type and HIV) and Parkinson’s Disease—Initial Results. J Cerebral Blood Flow Metab 1988; 8:5109- 15. 16. Kouris K, Jarritt PH, Costa DC, Eli PJ. Physical assessment of the GE/CGR Neurocam and comparison with a single rotating gamma-camera. EurJ Nucl Med 1992; 19:236-42. 17. Costa Dc, Jerritt PH. Eli PJ. The effect of ROl size and plane of reconstruction on HMPAO/SPET rCBF studies. Nuc Med Carmen 1989; 10(4):253. 18. Costa DC, Brostoff J, Douli V, Eli PJ. Postviral fatigue syndrome. Br Med J 1992; 304:1567. 19. Costa DC, Brostoff J, Douli V, Eli PJ. Brainstem hypoperfusion in patients with Myalgic Encephalomyelitis -Chronic Fatigue Syndrome. Eur J Nucl Med 1992 19:733. 20. Yuosef G, Bell E, Manu G. et aI. Chronic enterovirus infection in patients with Post-viral Fatigue Syndrome. Lancet 1988;I:146-50. 21. Straus SE, Tosato G, Armstrong G, et al. Persisting illness and fatigue in adults with evidence of Epstein Barr Virus Infection. Ann Intern Med 1985;102:716. 22. Wakefield D, Lloyd A. Pathophysiology of Myalgic Encephalomyelitis. Lancet 1987;11:918-19. 23. Klimas NG, Salvato FR, Morgan R. Fletcher MA. Immunologic abnormality in Chronic Fatigue Syndrome.J Clin Microbiol 1990;1403-10 24. Troughton AH, Blacker R, Vivian G. 99mTc-HMPAO SPET in Chronic Fatigue Syndrome- Clin Radiol 1992; 45:59. 25. Schwartz RB, Garada BM, Vasile R Komaroff A, Holman BL. Tc-99m HMPAO SPECT in the diagnosis of CFS. J Nucl Med 1993; 34:47P. 26. Mena I, Goldstein J, Jouanne E, Lesser I. Cerebral hypoperfusion in late life chronic fatigue syndrome (CFS) and late life depression (D). J Nucl Med 1993; 34:210P. 27. Ichise M, Salit I, Abbey S, et al Assessment of regional cerebral perfusion by 99Tcm-HMPAO/SPECT in Chronic Fatigue Syndrome. Nucl Med Common 1992;.13:767-72. 28. Schwartz RB, Komaroff AL, Garada BM, at al. SPECT imaging of the Brain: Comparison of Findings in Patients with Chronic Fatigue Syndrome, AIDS Dementia Complex, and Major Unipolar Depression. Am J Radiol 1994; 162:94351. 29. Bakheit AMO, Bahan PO, Dinan TG, Gray CE, O’Keane V. Possible upregulation of hypothalamic 5-hydroxytryptamine receptors in patients with postviral fatigue syndrome. Br Med J 1992; 304:1010-12. 30. Morriss R, Sharpe M, Sharpley AL et al. Abnormalities of sleep in patients with chronic fatigue syndrome. Br Med J 1992; 306;1161-4: 31. Neeley SP. Cross AJ, Crown TJ, et al, Herpes Simplex Virus Encephalitis, Neuroanatomical and Neurochemical Selectivity. J Neurological Sci 1985; 71;325-37. 32. Strauss SE, Tosato G, Armstrong G. Persistent illness and Fatigue in Adults with Evidence of Epstein-Barr Virus Infection. Anna Intern Med 1985;102:7-16. 33. Buchwald D, Cheney PR, Peterson DL, et al. A Chronic illness Characterised by Fatigue, Neurologic, and Immunologic Disorders, and Active Human herpes virus Type 6 Infection. Ann intern Med 1992;116;10313. “““““““““““““““““““““““““““““““““““““““““““““““““““““““““““““““““ Table 1 Brain perfusion ratios (mean ±SD) in 24 patients with ME/CFS and 24 normal volunteers included in the initialpilot study. p values are for unpaired Student’s t-test Table 2 Reduced brainstem perfusion in patients with ME/CFS Both the ME-CFS and the pilot group showed lower brainstem perfusion CBS) than that in depressed patients, who were not significantly different from normals. p values have been obtained via ANOVA with Bonferroni corrections. NS, non-significant at the 5% level. Table 1 and 2 not reproducible “““““““““““““““““““““““““““““““““““““““““““““““““““““““““ Figure 1. Radioactivity ratios (on the y-axis) for various regions of the brain. R/L cer, right over left cerebellar hemispheres. Radioactivity ratios for the following regions have as a common denominator the cerebellar hemisphere with higher count- . rate: RF and LF, right and left frontal cortex; RP and LP, right and left parietal cortex; RMT and RLT, right menial and lateral temporal cortex LMT and LLT, left mesial and lateral temporal cortex; RCN and LCN, right and left visual cortex; RCN and LCN, right and left caudate nucleus; RT and LT, right and left thalamus; BS, brainstem. a.) Marked hypoperfusion in the brainstem of a patient with ME/CFS. b.) Frontal, parietal and temporal hypoperfusion with normal brainstem perfusion in a patient with major depression. “““““““““““““““““““““““““““““““““““““““““““““““““““““““““““““““““““““ Figure 2. Brainstem perfusion in a typical patient with ME-CFS is lower than that in a typical normal volunteer, and in a typical patient with depression. The colour bar on the left hand side represents the distribution of relative perfusion. See text for further explanation. Figures 1 a & b and Figure 2 not reproducible “““““““““““““““““““““““““““““““““““““““““““““““““““““““““