19429 Service Spec & Additional Forms 2012
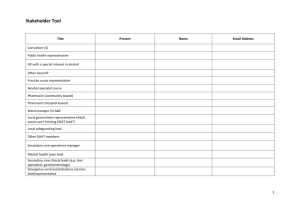
advertisement

Minor Ailments Scheme In Pharmacies Treatment of Minor Ailments by Community Pharmacists Contents Description Acknowledgements Service Specification Introduction Transfer into Minor Ailment Scheme Duties of participating Surgeries Duties of participating Community Pharmacies Referral procedure Service funding and payment mechanism Monitoring and evaluation Pharm Claim Pro-forma (Pharmacist prescription and patient exemption) Monthly Summary Sheet Minor Ailment Protocols: Page Number 3 4-6 4 4 4 5 5 6 6 7-8 9 12-33 Athlete’s Foot Cold Sores Colds / Flu / Earache Constipation Cough Diarrhoea Hay Fever / Allergy Relief Head Lice Temperature Nappy Rash Nasal Congestion Sore Throat Threadworms Vaginal Thrush Veruccas and Warts 13 14 15 17 18 20 22 24 25 27 28 29 30 31 33 Receptionists Protocol Pharmacists Protocol Pharmacist Referral Form Identification of a named professional lead Flowchart 34 36 37 38 39 d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 2 of 39 Approval Approval to undertake the pilot scheme was made at the Solis Board, Dec 2012 Monitoring and Reporting This pilot scheme is reported to and monitored by Solihull CCG Members Support team. If a recommendation to continue the pilot is made, then the responsibility for monitoring and reporting of the operation of the scheme will need to be assigned. Solihull CCG Kate Arnold, Head of Medicines Management, NHS Solihull CCG Tony Sargent, Commissioning Facilitator, NHS Solihull CCG Parveen Baden, Community Pharmacy Development Manager, Birmingham and Solihull NHS Cluster Pilot Scheme Details Commencement Date: February 2013 Review Date: August 2013 Service Specification and Clinical Protocols developed by Yvonne Murphy and Kalpesh Patel, Senior Pharmaceutical Adviser Birmingham and Black Country Commissioning Support Unit.(BBCS CCG) Pilot Practice Bosworth Medical Centre Pharmacists and staff from Community Pharmacies in Pilot Boots UK Ltd, Crabtree Drive, Chelmsley Wood Boots UK Ltd, 29-31 Greenwood Way, Chelmsley Wood Asda Stores Ltd, Bosworth Drive Lloyds Pharmacy, 3 Bell Lane, Tile Cross Dudley Taylor Pharmacies, 5 Craig Croft, Chelmsley Wood Protocol Authorised by: Dr R Clowes, Bosworth Medical Centre Kate Arnold, Head of Medicines Management, NHS Solihull CCG Professionals To Whom This Protocol May Apply Authorised professionals shall be: Pharmacists currently registered with the GPhC. Staff shall have satisfied competence criteria required by their designated responsible professional in: o Knowledge of the clinical situation the protocol applies to o Knowledge of medicines listed and their effects o Continuing Education requirements o Working under protocol for the NHS supply d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 3 of 39 Service Specification 1. Introduction 1.1 This service is available to all patients exempt from prescription charges, including those with pre payment certificates, registered with the surgeries participating in the scheme. Patients are at liberty to refuse this service. Patients who pay for their prescriptions should be referred to a pharmacy to purchase medicines in the usual way. 1.2 The service is only available for the minor ailments identified on page 10. 1.3 Only community pharmacies who are committed to making staff available to provide the service and who have successfully completed the appropriate training provided by Birmingham Black Country and Solihull Commissioning Support Unit (BBCS CSU) on behalf of the Solihull Clinical Commissioning Group (SCCG) will be included in the scheme. Additionally it is recommended that all pharmacists participating in the scheme should complete the most recent CPPE package on Minor Ailments. 1.4 In order to be eligible to participate in the scheme, the pharmacy must have a consultation room available for carrying out minor ailments consultations. 2. Transfer of Care 2.1 Patients presenting with identified symptoms at the GP surgery will be offered transfer into this service. Patients may also self refer following initial practice referral and registration at a participating pharmacy. 2.2 Patients presenting at a participating community pharmacy and registered with a participating GP will receive the service level of care as laid out in this specification. 2.3 Patients wishing to access the service must present identification and reasonable proof of registration with a participating practice. This can be a. Their NHS card or a minor ailments leaflet from their surgery bearing the surgery stamp/pharmacy stamp with the patients name, address and date added by surgery/pharmacy staff b. Be registered on the pharmacy computer system and known to the pharmacist. c. Confirmation of registration with the practice through telephone call 2.4 If registration with a participating practice is in doubt the patient will not be eligible for this scheme and they will be advised to access medical care through the usual channels. 3 Duties of Participating Surgeries 3.1 All patients requesting appointments (either immediately or on an appointment basis) for symptoms matching the criteria identified can be offered transfer into the service using the protocol on page 34. 3.2 Patients presenting in person at the surgery and accepting transfer into the scheme should be issued with a minor ailments leaflet and given a list of participating pharmacies. The leaflet should be stamped by the practice for presentation at one of d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 4 of 39 the participating pharmacies; the patient’s name and address should be written on the back of the leaflet. 3.3 Patients accepting transfer by phone will be advised to take evidence of identity and registration at the practice to one of the participating community pharmacies. In the absence of an NHS card or a practice stamped minor ailments leaflet the pharmacist may telephone the surgery to confirm registration. 3.4 All surgeries should co-operate and liase with the community pharmacists to activate the referral procedure when required (see section 5). 3.5 All participating GP surgeries should display official posters and provide leaflets promoting the service. 3.6 For patients under the age of 16 the parent or guardian can accept transfer into the scheme on behalf of the patient. 4 Duties of participating accredited Community Pharmacists 4.1 Patients should only be accepted into the service if the Pharmacist can confirm their identity and has reasonable proof of registration with a participating GP. 4.2 Community Pharmacists and any relevant members of staff should attend the training provided by the BBCS CSU before taking part in the scheme. 4.3 All participating community pharmacies will provide a professional consultation service for patients registered with participating GPs who present with one of the specified conditions. 4.4 The Pharmacist will assess the patient’s condition. The consultation will consist of: 4.4.1 Patient assessment 4.4.2 Provision of advice 4.4.3 Provision of a medication if necessary from the agreed formulary, appropriate to the patient’s condition. 4.4.4 Pharm. Claim (pharmacist’s prescription and patient exemption form) to be completed. The Pharmacist should ensure that the patient has completed and signed the declaration of exemption from prescription charges. The Pharmacist should also ensure that they sign and stamp the paperwork. 4.5 The Code of Ethics and Standards as detailed in the Royal Pharmaceutical Society of Great Britain’s Medicines, Ethics & Practice should be complied with at all times in the provision of the service. 4.6 Patient data recorded on the Pharm Claim forms should be stored securely, in accordance with the Data Protection Act, and kept for 3 years. 4.7 Where possible, record the supply on the patient’s record on the pharmacy computer system 4.8 Implementation of the rapid referral process if symptoms meet agreed criteria. 4.9 If a patient presents persistently the patient should be referred to their surgery. If the symptoms do not meet the criteria for rapid referral, patients should be advised to make an appointment in the normal manner. 4.10 If the Pharmacist suspects that the patient and/or parent is abusing the scheme they should alert the practice where the patient is registered in the first instance. d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 5 of 39 4.11 Community pharmacies will be required to complete and submit the “Monthly summary sheet along with the relevant months’ Pharm. Claim pro-formas (Pages 7-9) to the Medicines Management Team at Solihull CCG unless otherwise directed. 4.12 If there is a Serious Incident associated with the operation of this scheme, the pharmacist should follow their own process, and notify the Risk Manager at Solihull CCG. 5 Referral procedure 5.1 If the patient presents with symptoms indicating the need for an immediate consultation with the GP, the Pharmacist should advise the patient to make an appointment at the surgery immediately and preferably assist the patient in doing so. If the surgery is closed and/or the symptoms are sufficiently severe the patient should be advised to contact the “out of hours” service or attend A & E immediately. 5.2 If the patient presents with symptoms indicating the need for a GP appointment, the Pharmacist should advise the patient to make an appointment at the surgery and indicate an approximate time period, for example 2-3 days or one week. 6. Service funding and payment mechanism The Community Pharmacy will be paid according to the following schedule 6.1 Fee per consultation 6.2 Drug costs (based on Drug Tariff price) £3.00 The monthly summary sheets (page 9) with relevant Pharm. Claims Pro-formas should be returned to the Member Support Team at Solihull CCG as soon as possible after the end of the month. Payments will be made to the participating pharmacy by BACS. Pharmacists are advised to retain a copy of the summary forms. Note that claim forms submitted more than 3 months in arrears will not be paid. 7. Monitoring and Evaluation Participating community pharmacies and surgeries will be expected to participate in monitoring and evaluation using the consultation data and staff/patient questionnaires. 7.1 Attitudinal survey of o GPs o Receptionists o Community Pharmacists o Patients d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 6 of 39 TO BE COMPLETED BY THE PHARMACIST Pharm. Claim Pro-forma (Pharmacists Prescription) Only to be completed if the patient is exempt from prescription charges and has signed the declaration opposite. Patients Name: ………………………………………………………………................ Date of Birth: …………………………… Patients Address:……………………………………………………………….…………… …………………………………………. ……………………………………… Postcode: …………………………. NHS No (if known):………………………………… GPs Name: …………………………… GP Surgery:.………………………………………........................................................... Minor Ailment Consultation: Date……………………………….. Time…………………………. Presenting signs, symptoms & duration: ………..………………………………………………………… ……………………………………………………………………………………………………………………… Minor ailment condition diagnosed:………………………………………………………………………….. Self-help advice given: …………………….……………………………………………………………………. Advice Only Referral to GP- same day Referral to GP- within a fortnight Medicine supplied: I supplied the above patient with the following item(s): Product supplied Product supplied 1 Clotrimazole Cream 1% 20g 8 Bug buster kit including nit comb Miconazole Cream 30g Malathion aqueous lotion (50ml/treatment) 2 Aciclovir 5% w/w cream 2g Malathion aqueous lotion (200ml) 3 Paracetamol Tablets 500mg (32) Malathion alcoholic liquid (50ml/treatment) Paracetamol susp SF 250mg / 5ml (100ml) Malathion alcoholic liquid (200ml) Paracetamol susp SF 120mg / 5ml (200ml) Permethrin crème rinse (59ml) Ibuprofen 200mg (24) Dimethicone lotion 50mL Ibuprofen susp 100mg/5ml (100ml) Dimethicone lotion 150mL Menthol & eucalyptus inhalation (100ml) 9 Paracetamol Tablets 500mg (32) 4 Senna tabs (20) Paracetamol susp SF 250mg / 5ml (100ml) Fybogel sachets (10) Paracetamol susp SF 120mg / 5ml (200ml) Lactulose (300ml) Ibuprofen 200mg (24) 5 200ml Simple Linctus or Ibuprofen susp 100mg/5ml (100ml) 200ml Paed Simple linctus 10 Sudocrem Cream 200ml SF Pholcodine linctus Clotrimazole 1% cream 6 Oral Re-hydration sachets (pack of 6): 11 Menthol & eucalyptus inhalation (100ml) Loperamide caps (6) Sodium chloride nasal drops (10ml) 7 Cetirizine tabs 10mg (30) Xylometazoline 0.1%nasal spray Cetirizine syrup 5mg/5ml (200ml) Xylometazoline 0.05% nasal drops Loratadine tabs 10mg (30) 12 Paracetamol 500mg tabs (32) Loratadine syrup 5mg/5ml (300ml) Paracetamol susp SF 120mg / 5ml (200ml) Sodium Cromoglycate eye drops (10ml) Paracetamol susp SF 250mg / 5ml (100ml) Beclomethasone nasal spray (180 sprays) 13 Mebendazole (OVEX®) 100mg – 1 tablets Chlorphenamine 4mg – 30 tablets Mebendazole (OVEX®) 100mg – 4 tablets Chlorphenamine syrup 2mg/5ml (150ml) 14 Clotrimazole Cream 1% 20g Hydrocortisone Cream 1% (15g) Clotrimazole Pessary 500mg Clotrimazole Combi Pack (500mg pessary + 1% cream) 15 Salatac Gel 8g Was evidence of exemption seen? YES NO Referral into scheme by SELF PRACTICE d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 7 of 39 TO BE COMPLETED BY THE PATIENT Declaration of Exemption I am entitled to free prescriptions as detailed below (please tick the relevant box): A B C D E F G L H K M S is under 16 years of age is 16, 17 or 18 and in full-time education is 60 years of age or over has a maternity exemption certificate has a medical exemption certificate has a prescription prepayment certificate has a valid War Pension exemption certificate is named on a current HC2 charge certificate *gets income support (IS) *gets income-based jobseeker’s allowance (JSA (IB)) *is entitled to, or named on a valid NHS Tax Credit Exemption Certificate *has a partner who gets Pension Credit guarantee credit (PCGC) Date of birth: *Name: 5 5 5 5 5 5 5 5 5 5 5 5 NI no. *Print the name of the person (either you or your partner) who gets IS, JSA (IB), PCGC or Tax Credit □ I am the patient □ Patient’s parent/ guardian (if patient under 16) I have received …………………. (insert number) items of medicine from this pharmacy today. 4 Patient declaration and consent The information provided is true and complete to the best of my knowledge I understand that if it is not, appropriate action may be taken against me For the purposes of verifying entitlement to exemptions, I consent to the disclosure of relevant information about me, including to and by the Inland Revenue and Local Authorities I understand and agree to the Pharmacist discussing any details regarding my medicines with my GP, if considered appropriate by the Pharmacist I consent to have my personal data and details about my prescribed medicines stored by the pharmacy I consent to the use of my data anonymously for statistical purposes I declare that I have been counselled by the Pharmacist and I have understood the advice given, and where a medicine has been supplied, I understand the information given Patient’s Signature: …………………………Date: ………… Print name: …..………………………….. I declare that I have given appropriate treatment or referral for the condition presented to me based on the information given to me by the patient, which to the best of my knowledge is correct. Pharmacy stamp Pharmacists Signature: …….………………. …………………………… Pharmacists Name (print) ………………………………………………... Date: …..…………………….. TOP COPY – TO GP PRACTICE MIDDLE COPY- TO SOLIHULL CCG BOTTOM COPY - PHARMACY d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 8 of 39 Monthly Summary Sheet (Please attach this form to the Pharm claim proformas for this month and submit monthly claims to Solihull CCG Medicines Management Team) I declare that for the month of ______________________________ the following items were supplied: Product supplied 1 2 3 4 5 6 7 No. of items Clotrimazole Cream 1% 20g Miconazole Cream 30g Aciclovir 5% w/w cream 2g Paracetamol Tablets 500mg (32) Paracetamol susp SF 250mg / 5ml (100ml) Paracetamol susp SF 120mg / 5ml (200ml) Ibuprofen 200mg (24) Ibuprofen susp 100mg/5ml (100ml) Menthol & eucalyptus inhalation (100ml) Senna tabs (20) Fybogel sachets (10) Lactulose (300ml) 200ml Simple Linctus or 200ml Paed Simple linctus 200ml SF Pholcodine linctus Oral Re-hydration sachets (pack of 6): Loperamide caps (6) Cetirizine tabs 10mg (30) Cetirizine syrup 5mg/5ml (200ml) Loratadine tabs 10mg (30) Loratadine syrup 5mg/5ml (300ml) Sodium Cromoglycate eye drops (10ml) Beclomethasone nasal spray (180 sprays) Chlorphenamine 4mg – 30 tablets Chlorphenamine syrup 2mg/5ml (150ml) Hydrocortisone Cream 1% (15g) Product supplied 8 9 10 11 12 13 14 15 Numbers of : Advice Only No. of items Bug buster kit including nit comb Malathion aqueous lotion (50ml/treatment) Malathion aqueous lotion (200ml) Malathion alcoholic liquid (50ml/treatment) Malathion alcoholic liquid (200ml) Permethrin crème rinse (59ml) Dimethicone lotion 50mL Dimethicone lotion 150mL Paracetamol Tablets 500mg (32) Paracetamol susp SF 250mg / 5ml (100ml) Paracetamol susp SF 120mg / 5ml (200ml) Ibuprofen 200mg (24) Ibuprofen susp 100mg/5ml (100ml) Sudocrem Cream Clotrimazole 1% cream Menthol & eucalyptus inhalation (100ml) Sodium chloride nasal drops (10ml) Xylometazoline 0.1%nasal spray Xylometazoline 0.05% nasal drops Paracetamol 500mg tabs (32) Paracetamol susp SF 120mg / 5ml (200ml) Paracetamol susp SF 250mg / 5ml (100ml) Mebendazole (OVEX®) 100mg – 1 tablets Mebendazole (OVEX®) 100mg – 4 tablets Clotrimazole Cream 1% 20g Clotrimazole Pessary 500mg Clotrimazole Combi Pack (500mg pessary + 1% cream) Salatac Gel 8g Referral to GP-same day Pharmacy Stamp: Name of Pharmacist submitting form (PLEASE PRINT): …………………………………… Pharmacist’s signature: …………………………………… Date: …………………………….. Referral to GP-within a fortnight d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 9 of 39 For Solihull CCG use only Grand total = ……………………………………………… plus VAT (at 17.5%) = …………………………………………………………………………………………………. Number of consultations (number of Pharm claim proformas) = ………………………………… x £3.00 = …………………………..……………………………………. Total payment ……………………………………………………………………………………………………………………………………………………………………………. Approved: Signature: ____________________________________ Date: ___________ ____________________________________ ____________ Member Support Team Finance Use – Passed for Payment Signature: ____________________________________________ (code:ref: Minor Ailments) Date: ______________________ Finance Manager d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 10 of 39 PROTOCOLS FOR Community Pharmacy MINOR AILMENTS SCHEME Details of contraindications, cautions, drug interactions, adverse effects and other product details are provided under the ‘Description of Treatment’ Section. This section should be referred to before supplying the medicine. This protocol has been developed using BNF 61. Any reports of unexpected severe reactions shall be recorded in the patient's computer record, the GP informed, and the MHRA informed via the yellow card system (http://yellowcard.mhra.gov.uk/) d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 11 of 39 Minor Ailment Protocols Patient with symptoms of the following conditions may be referred in to this scheme and advice and treatment will follow the regime laid out in the following pages: 1. Athlete’s Foot Page 13 2. Cold Sores Page 14 3. Colds / Flu /Earache Page 15 4. Constipation Page 17 5. Cough Page 18 6. Diarrhoea Page 20 7. Hay Fever / Allergy Relief Page 22 8. Head Lice Page 24 9. Temperature Page 25 10. Nappy Rash Page 27 11. Nasal Congestion Page 28 12. Sore Throat Page 29 13. Threadworms Page 30 14. Vaginal Thrush Page 31 15. Veruccas and Warts Page 33 . d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 12 of 39 1 ATHLETE’S FOOT Definition / Criteria Fungal skin infection affecting the foot, most commonly the area between the toes Criteria for inclusion Adults and children presenting with symptoms of: Itching, scaling and inflammation of the skin between the toes. And consent has been given Criteria for exclusion Children under 1 year Diabetics Patients whose infection has spread to toenails Previous treatment failure Patients not registered with a GP within the scheme Known hypersensitivity to the drug or any other ingredient in the product. Pregnancy Breastfeeding See individual products for additional exclusion criteria Action for excluded patients and non-complying patients Referral to GP When and how to refer to GP Rapid referral: - N/A Consider supply, but patient should be advised to make an appointment to see the GP: If toenail become black or discoloured or if infections starts to spread under nails If fungal infection spreads to other parts of body Bacterial infection suspected Patient has had the symptoms for >4weeks No improvement after using OTC preparation for 2 weeks If there is any other on-going concern Special considerations / concurrent medication Antibiotics Oral steroids / immunosuppressants Recommended treatments, route and legal status Frequency of administration and maximum dosage Clotrimazole Cream 1% 20g Miconazole Cream 30g Apply thinly 2-3 times a day. Apply twice a day. Continue using the cream for two weeks after the infection has cleared Follow-up and advice Wash & dry feet thoroughly especially between toes. Avoid warm damp conditions. Care with swimming pools, baths, shared towels or wet floors. Wearing clean wool or cotton socks may allow the skin to breath and can reduce moisture next to skin. To prevent re-infection feet should be washed daily and particular attention given to drying thoroughly – especially between the toes. Tight footwear should be avoided, socks should be changed frequently and shower shoes should be worn at swimming pool and sports hall locker rooms and showers, as these are places where the infection is often picked up. Side effects and their management Sensitivity to imidazoles Occasional local irritation and hypersensitivity reactions include mild burning sensation, erythema and itching. Treatment should be discontinued if these are severe. d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 13 of 39 2 COLD SORES Definition / Criteria Herpes simplex (Cold sores) Criteria for inclusion Adults and children with herpes simplex infection of lips and face Criteria for exclusion Patients unsure if it is Herpes simplex infection Immunocompromised patients If patient has suspected: Hand, foot and Mouth disease Herpes zoster (Shingles) infection Infectious mononucleosis Impetigo Patients not registered with an GP within the scheme Action for excluded patients and non-complying patients Referral to General Practitioner When and how to refer to GP Rapid referral: Immunocompromised patients Herpes zoster (shingles) Conditional referral: On 3rd occurrence Consider supply, but patient should be advised to make an appointment to see the GP: Regular occurrence of condition Suspected differential diagnosis If there is any other on-going concern Recommended treatments, route and legal status Frequency of administration and maximum dosage Aciclovir 5% w/w cream 2g Adults & Children over 3 months: Apply Five times a day for 5 days Follow-up and advice Cream needs to be started in early “tingling” stage of infection Many cold sores need no treatment at all and resolve in a few days Antiviral cream will reduce duration and severity of a cold sore but may have no effect Sunscreen lip balm may help to prevent cold sores if strong sunlight is a trigger Close contact, e.g. kissing, sharing cups etc, may pass on the virus Advise paracetamol or ibuprofen if required for pain relief Drinking fluid in those where infection causes excessive pain and so reduced intake Side effects and their management Transient stinging and/or burning – Advise Occasionally erythema, itching or drying of the skin - Advise d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 14 of 39 3 COLD / FLU / EARACHE Definition / Criteria Cold: widespread infectious virus disease causing inflammation of the mucous membranes of the nose, throat & bronchial tubes. Flu: highly contagious virus infection that affects the respiratory system Earache: Associated with URTI Criteria for inclusion Patients presenting with symptoms of cold / flu, e.g. fever, temperature, nasal congestion or other nasal symptoms. Criteria for exclusion Patients under one year Concomitant rash that does not fade under pressure e.g. with glass Patient is breathless Light hurts the eyes It is painful to bend the neck Systemic decongestants (pseudoephredrine) should not be supplied to patients taking MAOI inhibitors and used with caution in patients with diabetes, hypertension, hyperthyroidism and ischaemic heart disease. Patients not registered with an GP within the scheme Action for excluded patients and non-complying patients - Referral to GP When and how to refer to GP Rapid referral: Patient presenting with a rash or other symptoms suggesting a serious condition, e.g. meningitis. Symptoms may include Development of a rash that does not fade when you press a glass tumbler against the rash Development of red-flag symptoms Patient becomes breathless Painful to bend the neck or light hurts the eyes Severe pain in children Discharge or bleeding from the ear Fever, nausea and vomiting Foreign body in the ear Neck stiffness Tinnitus and vertigo * Signs and symptoms suggesting increased likelihood of serious illness include: Pallor: Not responding normally to social cues: Wakes only with prolonged stimulation: Decreased activity: No smile: Nasal flaring: Tachypnoea: Crackles: Dry mucous membrane: Poor feeding in infants: Reduced urine output: Fever for > 5 days: Swelling of a limb or joint: Non-weight bearing/ not using extremity: A new lump>2cm. See NICE clinical guideline 47 “Feverish illness in children” for details Conditional referral: Patients should consult the GP if treatment is ineffective or persists after 7 days. Patients with other chronic illness e.g. heart, kidney or lung disease, those with reduced immunity or patients living in long-stay institutions. These patients would benefit from influenza vaccination. Consider supply, but patient should be advised to make an appointment to see the GP: If more than one request per month If there is any on-going concern New symptoms develop particularly in the young children, the elderly or the infirm Symptoms worsening d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 15 of 39 Recommended treatments, route and legal status Frequency of administration and maximum dosage Paracetamol Tablets 500mg (32) Paracetamol susp SF 250mg / 5ml (100ml) Paracetamol susp SF 120mg / 5ml (100ml) po P adults, children over 16yrs 1 -2 qds Paracetamol new dosage guidance for children 12-16 years 750mg 15mls x 250mg/5ml susp 10-12 years 500mg 10ml x 250mg/5ml susp 8-10 years 375mg 7.5ml x 250mg/5ml susp 6-8 years 250mg 5ml x 250mg/5ml susp 4-6 years 240mg 10ml x 120mg/5ml susp 2-4 years 180mg 7.5ml x 120mg/5ml susp 6-24 months 120mg 5ml x 120mg/5ml susp 3-6 months 60mg 2.5ml x 120mg/5ml susp Ibuprofen 200mg (24) These doses may be repeated every 4-6 hours when necessary (maximum 4 doses in 24 hours) Ibuprofen susp 100mg/5ml (100ml) po P adults, children over 12 years 1-2 tds Adults & Children 12 years and over: 200 - 400mg Children 10-12 years 300mg (15ml of suspension) Children 7-10 years 200mg (10ml suspension) Children 4-7 years 150mg (7.5ml of suspension) Children 1-4 years 100mg (5ml of suspension) Children 6 months – 1 year 50mg (2.5ml suspension) Children 3-6 months (over 5kg body weight) 50mg (2.5ml suspension) THESE DOSES MAY BE REPEATED UP TO THREE TIMES A DAY Menthol & eucalyptus inhalation (100ml) Inhale GSL To be inhaled PRN Follow-up and advice Ibuprofen should not be used in patients suffering from asthma or gastro-intestinal problems. Caution using ibuprofen in patients with hypertension or those on ACE inhibitors (increased risk of renal impairment) Pharmacists should be aware of the NICE guidance in Feverish Children and can advice on alternating ibuprofen with paracetamol if neither work individually. Cold / Flu Patients should be advised to put 1 tsp. of menthol & eucalyptus in a pint of hot (not boiling) water and use a cloth/towel over the head to trap the steam. Maximum use of topical decongestants is seven days. Simple analgesics to bring temperature down Steam inhalation (with or without aromatic inhalant) Maintain a good fluid intake Encourage rest (if possible) Warm soothing drinks Common cold does not require antibiotics for effective treatment Remind high risk patients of influenza vaccination programmes (over 65’s, and those patients under 65 with CHD, respiratory disease or diabetes) Development of new symptoms and or symptoms have deteriorated, consult GP. Earache Enquire about concurrent analgesic usage: Paracetamol daily dose – avoiding use of other products containing paracetamol Other NSAIDs – prescribed or OTC Rest, warming, cooling or changing position, may obtain relief from pain. Patients should be advised to avoid any aggravating factors. Side effects and their management Side effects are rare with occasional use of paracetamol when taken at the recommended dose. Ibuprofen should be taken with, or after food, to avoid gastro-intestinal side effects d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 16 of 39 4 CONSTIPATION Definition / Criteria Increased difficulty and reduced frequency of bowel evacuation compared to normal Criteria for inclusion Adults and children 12 years and over presenting with: Significant variation from normal bowel evacuation which has not improved following adjustments to diet and other lifestyle activities (see below). And consent has been given Criteria for exclusion Children under 12 years. Patients not registered with an GP within the scheme Known hypersensitivity to the drug or any other ingredient in the product. Pregnancy Breastfeeding See individual products for additional exclusion criteria Patients currently receiving laxatives as part of their regular medication. Pharmacists should exercise their professional judgement to implement dosage alteration to existing laxative regime Action for excluded patients and non-complying patients - Referral to GP When and how to refer to GP Rapid referral: Blood or mucus in the stools Abdominal pain, distension or vomiting Conditional referral: If constipation persists beyond one week, consult the GP Consider supply, but patient should be advised to make an appointment to see the GP: If more than one request per month Change in bowel habit / repeated bouts of constipation If there is any other on-going concern Special considerations / concurrent medication Patients taking medication with recognised constipating effects Pregnant or breast-feeding women Recommended treatments, route and legal status Frequency of administration and maximum dosage Adults only: Senna tabs (20) Fybogel sachets (10) Lactulose solution (300ml) po po po P P P 2 on prn 1 bd 15mls BD (Adult) 10mls BD (5-10 years) 5mls BD (1-5 years) Follow-up and advice Regular doses of laxatives are rarely required and can cause a “lazy” bowel. Advice re considering alteration to diet to prevent the occurrence of further events e.g. increased fibre and fluid intake and increased physical activity if appropriate. Senna should not be used in pregnancy – advise Fybogel instead Side effects and their management If dosage is too large, griping and diarrhoea may result Senna may colour the urine yellow or red Laxative abuse ( associated with eating disorder) can lead to hypokalaemia Lactose intolerance d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 17 of 39 5. COUGH Definition / Criteria Coughing arising as a defensive reflex mechanism Persistent cough of less than 3 weeks duration Criteria for inclusion Adults and children aged 2 years and over presenting with: A dry unproductive cough requiring a degree of suppression Troublesome cough requiring soothing, with or without attendant mucous production And consent has been given Criteria for exclusion Children under 2 years old (See MHRA guidance below) Patients with a history of chronic bronchitis Cough productive of green / blood stained sputum Asthmatics presenting with wheeze or reduced peak-flow Patients experiencing sudden weight loss Patients not registered with a GP within the scheme Known hypersensitivity to the drug or any other ingredient in the product. Pregnancy Breastfeeding COPD and bronchiectasis Significant co-morbidities (heart, lung, renal, liver or neuromuscular disease, immunosuppression, CF) See individual products for additional exclusion Action for excluded patients and non-complying patients Referral to GP When and how to refer to GP Rapid referral: Constant chest pain or chest pain on normal inspiration Difficulty breathing (e.g. shortness of breath at rest) Cough productive of green/yellow/blood stained sputum If pain related to exertion If cough and other symptoms persist beyond one week the patient should consult the GP Asthmatics presenting with wheeze or reduced peak-flow Difficulty breathing Weight loss Night sweats COPD and bronchiectasis or significant co-morbidities as above Elevated Respiratory rate or large respiratory effort High temperature Tachycardia Reduced PEFR esp if <50% predicted Older than 65 years plus two or older than 80 years plus one of the following: o Hospitalisation in previous year o Type 1 or 2 diabetes o Congestive heart failure o Current use of oral steroids (based on NICE CG 69) o Consider supply, but patient should be advised to make an appointment to see the GP: If cough and other symptoms persist beyond one week A persistent, dry, night time cough particularly in children A dry cough in a patient prescribed an ACE inhibitor Patients diagnosed with asthma, GORD or post nasal drip. If there is any other on-going concern d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 18 of 39 Recommended treatments, route and legal status Frequency of administration and maximum dosage Simple Linctus x200ml Adults (12yrs & over) Paediatric Simple Linctus X200ml Children (212yrs) Sugar free Pholcodine Linctus 5mg/5ml x200ml Adults (12yrs and over) Children (6-12yrs) generally not recommended po po GSL GSL 5-10ml up to qds 5-10ml up to qds po GSL 5-10ml up to qds po 2.5ml up to 3-4 times a day MHRA: Children 6-12 years: Should only be considered after basic principles of best care have been tried and treatment restricted to five days only. Patient should be advised not to smoke and to try to avoid smoky or dusty atmospheres. Making sure the air is humid enough may be beneficial, e.g. placing a damp towel over a radiator. Patients can manage their cough by: o Using a steam inhalation o Sucking lozenges, preferably sugar free and keeping to the recommended dose o Taking warm drinks, such as a teaspoon each of honey and lemon dissolved in warm water The MHRA has stated that non-prescription cough and cold medicines containing the following active ingredients should not be used in children under 6 years old and may have limited efficacy in children under 12 years old: Antihistamines – brompheniramine, chlorphenamine and diphenhydramine Cough expectorants – guaifenesin and ipecacuanha Cough suppressants – dextromethorphan and pholcodine Decongestants – phenylephrine, pseudoephedrine, ephedrine, oxymetazoline and xylometazoline Follow-up and advice Check smoking status , where appropriate offer smoking cessation/referral information Maintain fluid intake with chesty cough Side effects and their management Constipation Respiratory depression NICE CG 69 http://www.nice.org.uk/nicemedia/live/12015/41322/41322.pdf Prodigy http://prodigy.clarity.co.uk/cough/management/scenario_diagnosis_cough_less_than_3_weeks#451191006 d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 19 of 39 6 DIARRHOEA Definition / Criteria Increased frequency and fluidity of defecation. Criteria for inclusion Adults and children > 1 presenting with the above symptoms, and consent has been given Criteria for exclusion* Patients not registered with a GP within the scheme Patients with chronic diarrhoea problems Children under 1 year Where clinical shock is suspected or confirmed Known hypersensitivity to the drug or any other ingredient in the product. Pregnancy Suspicion of abuse See individual products for additional exclusion criteria Action for excluded patients and non-complying patients Referral to General Practitioner - offer dietary advice When and how to refer to GP Rapid referral: Adults where symptoms have lasted more than 5 days Children where symptoms have lasted more than 48 hours or who look ill or dehydrated Rectal bleeding or blood or mucus in the stool Severe symptoms, including abdominal pain Children who are immunocompromised Elderly >70 years Weight loss Recent travel abroad Food handlers Red flag Signs of clinical dehydration or shock** If a child persistently vomits the ORS solution. Consider supply but patient should be advised to make an appointment with the GP: If symptoms persist beyond 48 hours If septicaemia is suspected Patients taking medications with recognised diarrhoea effect If there is any other on-going concern Recommended treatments, route and legal status Frequency of administration and maximum dosage First line Oral Re-hydration sachets (pack of 6): Child: (1-12 years) 200ml after every loose motion. Adult: According to fluid loss, usually 200 - 400ml solution after every loose motion. Oral re-hydration sachets(6) po GSL Reconstitute one sachet with 200ml of water (freshly boiled & cooled for infants) Any unused reconstituted solution should be discarded 1 hour after preparation. If stored in a fridge the solution can be kept for up to 24 hours Second line if required for circumstances (adults only and children>12) Loperamide caps (6) GSL 2 capsules stat then 1 after every loose motion (max 8 in 24 hours) Note: Should not be provided if patient has recently taken anti-biotics d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 20 of 39 Follow-up and advice Explain that diarrhoea usually lasts for 5-7 days and stops within 2 weeks, and vomiting usually lasts for 1-2 days and stops within 3 days. Explain treatment and course of action Explain that after reconstitution any unused solution should be discarded no later than 1 hour after preparation unless stored in a refrigerator when it may be kept for 24 hours. Monitor condition and seek medical advice if symptoms of dehydration develop, or symptoms do not resolve as expected During rehydration therapy do not give solid foods to children For children without red flag signs, do not routinely give oral fluids other than ORS solution; however consider supplementing with usual fluids (including milk feeds or water, but not fruit juices or carbonated drinks) if they consistently refuse ORS solution In infants, breast feeding or normal formula feeds should be offered between oral rehydration drinks. After rehydration, give full-strength milk straight away, reintroduce child’s usual solid food, avoid giving fruit juices or carbonated drinks until the diarrhoea has stopped. Adult patients should take clear fluids for 24-48 hours until symptoms resolve. If condition worsens or symptoms persist then seek further medical advice Advise parents, carers and children that: − washing hands with soap (liquid if possible) in warm running water and careful drying are the most important factors in preventing the spread of gastroenteritis − hands should be washed after going to the toilet (children) or changing nappies (parents/carers) and before preparing, serving or eating food − towels used by infected children should not be shared − children should not attend any school or other childcare facility while they have diarrhoea or vomiting caused by gastroenteritis − children should not go back to their school or other childcare facility until at least 48 hours after the last episode of diarrhoea or vomiting − children should not swim in swimming pools for 2 weeks after the last episode of diarrhoea. All severe adverse reactions, including anaphylaxis, should be reported to the MHRA via the yellow card system and recorded in the medical records. Verbal information should be provided to patients / carers and, if requested, written information in the form of a patient information leaflet should be given. Reconstitute 1 sachet with 200mL of water (freshly boiled & cooled for infants) Patients should eat as soon as they are able - foods rich in carbohydrates eg rice, pasta, bread, potatoes recommended Avoid dehydration by drinking plenty of fluids Babies, small children and the elderly are more susceptible to dehydration Avoid all dairy products Side effects and their management Loperamide can cause abdominal pain and bloating and should not be provided if the patient has recently taken anti-biotics *NICE Clinical Guideline 84 Diarrhoea and vomiting in children ** Red Flag signs of clinical dehydration include : Appears to be unwell or deteriorating, Altered responsiveness, sunken eyes, tachycardia, tachypnoea, reduced skin turgor. Symptoms of clinical shock include: decreased level of consciousness, pale or mottled skin, cold extremities, weak peripheral pulses. See NICE Clinical Guideline 84 for further details. d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 21 of 39 7 HAY FEVER /ALLERGY RELIEF Definition / Criteria Treatment of allergic reactions e.g. hayfever and urticaria, bites and stings Criteria for inclusion Adults and children over 6 years presenting with: Allergic rhinitis (hayfever) Allergic reactions resulting in a rash or inflammation and itchiness And consent has been given Children over 6 years (N.B. Follow specific age restrictions for individual product - some are not licensed for children under 12 years) Adults and children over the age of 10 years presenting who: Have been bitten or stung by small insects, Have localised minor irritation to the skin Criteria for exclusion Patients not registered with a GP within the scheme Known hypersensitivity to the drug or any other ingredient in the product. Pregnancy Breastfeeding Epilepsy See individual products for additional exclusion criteria Specific to Hydrocortisone Children under the age of 10 years Bites or stings to the face or anogenital region Where skin is broken or infected In acne rosacea Action for excluded patients and non-complying patients - Referral to GP When and how to refer to GP Rapid referral: Shortness of breath Pain in eyes Nasal ulceration/ crusting Conditional referral: Patient should consult the GP if treatment is ineffective or persists after the end of September If there is any other on-going concern Special considerations / concurrent medication Glaucoma (antihistamines contra-indicated) Patients on anti-arrhythmic drugs (antihistamines contra-indicated) Recommended treatments, route and legal status Frequency of administration and maximum dosage Cetirizine tabs 10mg (30) Cetirizine syrup 5mg/5ml (200ml) po po P P Loratadine tabs 10mg (30) po P 10mg daily Adult 10mg daily 2-6 years 2.5mg BD 6-12 years 5mg BD 10mg daily d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 22 of 39 Loratadine syrup 5mg/5ml (300ml) po P Sodium Cromoglycate eye drops (10ml) Beclomethasone nasal spray (180 sprays) Adults over 18 years only Chlorphenamine 4mg – 30 tablets (over 6 years – check dose) Chlorphenamine syrup 2mg/5mL – 150mL (over 1 year) Hydrocortisone Cream 1% 1x15g . topical P topical P po P po P topical P Adult 10mg daily Body weight under 30kg 5mg daily (not recommended under 2 years) Body weight over 30kg 10mg daily 1 drop QDS 2 sprays each nostril BD Dose (including maximum dose): Adults & Children 10 years and over: Apply sparingly over the affected area 1-2 times daily for a maximum of 7 days Follow-up and advice Explain treatment and course of action Advise patient not to exceed the stated dose If condition worsens or symptoms persist then seek further medical advice All severe adverse reactions, including anaphylaxis, should be reported to the MHRA via the yellow card system and recorded in the medical records. Verbal information should be provided to patients / carers and, if requested, written information in the form of a patient information leaflet should be given. If there is transient drowsiness, do not drive or operate machinery Advise patient to take pollen avoidance measures and to check daily pollen count Advise re smoking cessation where appropriate. Side effects and their management There are unlikely to be any side effects if treatments used at recommended doses. Fatigue, headache and nausea have been reported rarely Potentially may cause drowsiness Refer to current BNF and individual product information for full detail Beclometasone spray Dryness and irritation of the nose and throat Epistaxis Headache Smell and taste disturbances Hypersensitivity reactions including bronchospasm Specific to Hydrocortisone Potential Adverse Effects Rare with mild corticosteroids used for short periods Sensitivity reactions – discontinue treatment Refer to current BNF and individual product information for full details d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 23 of 39 8 HEAD LICE Definition / Criteria Infection with live moving head lice Criteria for inclusion Patients who are proven to be infected with live moving head lice. Criteria for exclusion Family/siblings of patient, who are not proven to be infected (note: infection is not indicated by the presence of nits (hatched & empty egg shells) Children under the age of 6 months Patients not registered with an GP within the scheme A second request within one week Action for excluded patients and non-complying patients Referral to GP When and how to refer to GP Rapid referral: - N/A Conditional referral: Pregnant or breastfeeding – wet combing method only or refer to GP If head lice persist after two lots of treatment within one month Consider supply, but patient should be advised to make an appointment to see the GP: If requesting repeat treatment more than twice in a month If there is any other on-going concern Special considerations / concurrent medication Alcoholic lotions not recommended for head lice in severe eczema / asthma. Pregnant or breast feeding Recommended treatments, route and legal status Frequency of administration and maximum dosage * First line treatment Wet combing method (Bug Busting) Bug Buster Kit * Second line treatment Insecticide Malathion aqueous lotion (50ml/treatment) topically P Malathion aqueous lotion (200ml) topically P Malathion alcoholic liquid (50ml/treatment) topically P Malathion alcoholic liquid (200ml) topically P Permethrin crème rinse (59ml) topically P Dimethicone lotion 50mL topically P Dimethicone lotion 150mL topically P The 200ml sizes are for use when two or more family members are affected. Follow-up and advice Wet comb well conditioned hair using a detection or nit comb to remove dead lice / eggs Regular weekly detection combing is recommended. Where Permethrin crème rinse is used, the patient should be advised to wash hair as normal prior to application, using shampoo ONLY, not 2 in 1 products or conditioner. Apply the Permethrin crème rinse to the clean damp hair & rinse after 10 minutes. With Malathion alcoholic liquid rub preparation into dry hair & scalp, allow hair to dry naturally, wash off after 12 hours. Two treatments are now recommended 7 days apart (this is different advice from package insert) Alcoholic solutions are suitable for people with normal healthy skin. These may be slightly more effective. Aqueous lotions are suitable for asthmatics or eczema/skin disorders Treatment to be repeated in seven days. The BNF recommends after 7 days to prevent lice emerging from eggs that survive the first time. The same chemical should not be used for the next re-infestation i.e. alternate treatments Side effects and their management - Side effects are rarely experienced Guidance reference: PRODIGY: http://www.prodigy.nhs.uk/guidance.asp?gt=Head%20lice d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 24 of 39 9 TEMPERATURE Definition / Criteria Raised body temperature Criteria for inclusion Adults and children presenting who: Need relief from symptoms e.g. feeling hot or cold or shivery, and are generally unwell Patients requiring relief of pain / fever associated with upper respiratory tract infections And consent has been given Criteria for exclusion * Children under 3 months Patients not registered with an GP within the scheme Known hypersensitivity to the drug or any other ingredient in the product. Pregnancy Breastfeeding Recurrent or severe pain See individual products for additional exclusion criteria Action for excluded patients and non-complying patients Referral to GP When and how to refer to GP Emergency referral: Suspected meningitis (vomiting, fever, stiff neck, light aversion, drowsiness, joint pain, fitting, cold extremities, nonblanching rash) – 999 call to avoid unnecessary delay Rapid Referral * Signs and symptoms suggesting increased likelihood of serious illness include: Pallor: Not responding normally to social cues: Wakes only with prolonged stimulation: Decreased activity: No smile: Nasal flaring: Tachypnoea: Crackles: Dry mucous membrane: Poor feeding in infants: Reduced urine output: Fever for > 5 days: Swelling of a limb or joint: Non-weight bearing/ not using extremity: A new lump>2cm. See NICE clinical guideline 47 “Feverish illness in children” for details. Consider supply but patient should be advised to make an appointment to see the GP: If symptoms have been present for longer than a week For children under 5 years where signs or symptoms suggest increased likelihood of serious illness* Patients recently returned from foreign travel (particularly in malarial regions) Patients that appear very unwell or have symptoms that suggest an infection that may need other GP input. If more than one request per month If there is any other on-going concern Recommended treatments, route and legal status Frequency of administration and maximum dosage Paracetamol Tablets 500mg (32) Dose (including maximum dose): Adult and children over 16 years 500 – 1000mg (1-2 x 500mg) tablets Paracetamol susp SF 250mg / 5ml (100ml) Paracetamol susp SF 120mg / 5ml (200ml) Paracetamol new dosage guidance for children 12-16 years 750mg 15mls x 250mg/5ml susp 10-12 years 500mg 10ml x 250mg/5ml susp 8-10 years 375mg 7.5ml x 250mg/5ml susp 6-8 years 250mg 5ml x 250mg/5ml susp 4-6 years 240mg 10ml x 120mg/5ml susp 2-4 years 180mg 7.5ml x 120mg/5ml susp 6-24 months 120mg 5ml x 120mg/5ml susp 3-6 months 60mg 2.5ml x 120mg/5ml susp d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 25 of 39 These doses may be repeated every 4-6 hours when necessary (maximum 4 doses in 24 hours) Dose (including maximum dose): Ibuprofen 200mg (24) Ibuprofen susp 100mg/5ml (100ml) po P adults, children over 12 years 1-2 tds Adults & Children 12 years and over: 200 - 400mg Children 10-12 years 300mg (15ml of suspension) Children 7-10 years 200mg (10ml suspension) Children 4-7 years 150mg (7.5ml of suspension) Children 1-4 years 100mg (5ml of suspension) Children 6 months – 1 year 50mg (2.5ml suspension) Children 3-6 months (over 5kg body weight) 50mg (2.5ml suspension) THESE DOSES MAY BE REPEATED UP TO THREE TIMES A DAY Ibuprofen should not be used in patients suffering from asthma or gastro-intestinal problems. Caution using ibuprofen in patients with hypertension or those on ACE inhibitors (increased risk of renal impairment) Pharmacists should be aware of the NICE guidance in Feverish Children and can advice on alternating ibuprofen with paracetamol if neither work individually. Follow-up and advice Enquire about concurrent analgesic usage: Paracetamol daily dose – avoiding use of other products containing paracetamol Other NSAIDs – prescribed or OTC Rest, warming, cooling or changing position, may obtain relief from pain. Patients should be advised to avoid any aggravating factors. NB overuse of analgesics can cause headaches Side effects and their management Side effects are rare with occasional use of paracetamol when taken at the recommended dose. Ibuprofen should be taken with, or after food, to avoid gastro-intestinal side effects d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 26 of 39 10 NAPPY RASH Definition / Criteria Rash often caused by local dermatitis Criteria for inclusion Child with identified rash in nappy contact area Criteria for exclusion If nappy rash diagnosis is uncertain Patients not registered with an GP within the scheme Action for excluded patients and non-complying patients Referral to General Practitioner When and how to refer to GP Rapid referral: Suspected systemic candidiasis Conditional referral: on 3rd occurrence Consider supply, but patient should be advised to make an appointment to see the GP: Patient not responding to initial treatment Widespread severe infection If there is any other on-going conncern Recommended treatments, route and legal status Frequency of administration and maximum dosage 1st Line: Sudocrem Cream Apply GSL Apply at each nappy change nd 2 Line: Clotrimazole 1% cream Apply P Apply thinly to the affected area twice daily Follow-up and advice Advise if symptoms do not resolve within 7 days to make an appointment to see a GP Advise guardian to ensure nappy change frequently and to avoid tightly fitting water-proof pants Advise on application of 2nd line therapy thinly Side effects and their management Sensitivity to Imidazoles, occasional local irritation. Discontinue if severe d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 27 of 39 11 NASAL CONGESTION Definition / Criteria Blocked nose associated with colds and upper respiratory tract Criteria for inclusion Adults and children presenting with: Congestion where seasonal allergy has been excluded and consent has been given Criteria for exclusion Known hypersensitivity to the drug or any other ingredient in the product. Pregnancy Diabetes or hyperthyroidism Recurrent nose bleeds Patients not registered with an GP within the scheme See individual products for additional exclusion criteria Action for excluded patients and non-complying patients - Referral to GP When and how to refer to GP Rapid referral: If suspected foreign body within nostril Swelling of the eyes, temples, nose or cheek Consider supply, but patient should be advised to make an appointment to see the GP: If symptoms persist for more than 2 weeks If more than one request per month If there is any other on-going concern Special considerations / concurrent medication Caution in hypertensive patients and patients with ischaemic heart disease Topical decongestants are contra-indicated in patients taking MAOIs Recommended treatments, route and legal status Frequency of administration and maximum dosage Menthol & eucalyptus inhalation (100ml) Sodium chloride nasal drops (10ml) inhalation nasal GSL GSL Xylometazoline 0.1%nasal spray (adults & children over 12yrs) Xylometazoline 0.05% nasal drops (6-12yrs) nasal GSL nasal GSL To be inhaled prn 1-2 drops into each nostril 3-4 x per day (before feeds for babies) 1 spray in each nostril 2-3 x per day (Max 7 days) 1-2 drops each nostril 1-2 x a day prn MHRA: Children 6-12 years should only be treated after basic principles of best care have been tried. Up to 5 days treatment only. Follow-up and advice N.B. Systemic products should only be supplied when topical products have been tried without success Patients should be advised to put 1 teaspoon of menthol & eucalyptus in a pint of hot (not boiling) water and use a cloth / towel over the head to trap and inhale the steam Maximum use of topical decongestants is seven days The MHRA has stated that non-prescription cough and cold medicines containing the following active ingredients should not be used in children under 6 years old and may have limited efficacy in children under 12 years old: Antihistamines – brompheniramine, chlorphenamine and diphenhydramine Cough expectorants – guaifenesin and ipecacuanha Cough suppressants – dextromethorphan and pholcodine Decongestants – phenylephrine, pseudoephedrine, ephedrine, oxymetazoline and xylometazoline Side effects and their management Local Irritation Nausea, headache After excessive use tolerance with diminished effect, rebound congestion Cardiovascular effects also reported Refer to current BNF and individual product information for full details d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 28 of 39 12 SORE THROAT Definition / Criteria A painful throat, often accompanied by viral symptoms (e.g. temperature and/or fever) Criteria for inclusion Adults and children presenting with: Sore throat that requires soothing And consent has been given Criteria for exclusion Patients under 2 years Patients taking DMARDS carbimazole Patients not registered with an GP within the scheme Known hypersensitivity to the drug or any other ingredient in the product. Pregnancy Breastfeeding Significant co-morbidities (heart, lung, renal, liver or neuromuscular disease, immunosuppression, CF) See individual products for additional exclusion criteria Action for excluded patients and non-complying patients Referral to GP When and how to refer to GP Rapid referral: Patients on immunosuppressants / oral steroids / drugs causing bone marrow suppression or accompanied by other clinical symptoms of blood disorders) Quinsy, large lesions, blisters in throat, possible strep throat Non blanching rash Patients taking methotrexate or carbimazole Assessment of Centor criteria (3 of Tonsillar exudates, Tender anterior cervical nodes, history of fever, absence of cough) Consider supply but patient should be advised to make an appointment with the GP: Symptoms suggesting oral candidiasis / tonsillitis/ strep throat The condition has persisted more than 10 days A second request within 1 month If there is any other on-going concern Assessment of Centor criteria (2 of Tonsillar exudates, Tender anterior cervical nodes, history of fever, absence of cough) Recommended treatments, route and legal status Frequency of administration and maximum dosage Paracetamol 500mg tabs (32) Paracetamol susp SF 120mg / 5ml (200ml) Paracetamol susp SF 250mg / 5ml (100ml) Dose (including maximum dose): Adult 500 – 1000mg 1-2 x 500mg tablets Paracetamol new dosage guidance 12-16 years 750mg 15mls x 250mg/5ml susp 10-12 years 500mg 10ml x 250mg/5ml susp 8-10 years 375mg 7.5ml x 250mg/5ml susp 6-8 years 250mg 5ml x 250mg/5ml susp 4-6 years 240mg 10ml x 120mg/5ml susp 2-4 years 180mg 7.5ml x 120mg/5ml susp 6-24 months 120mg 5ml x 120mg/5ml susp 3-6 months 60mg 2.5ml x 120mg/5ml susp 1-2 qds These doses may be repeated every 4-6 hours when necessary (maximum 4 doses in 24 hours) Follow-up and advice Patients should be advised to gargle with salty water Patients should avoid smoky or dusty atmospheres and reduce or stop smoking. Patients who find swallowing painful should take a light fluid diet. Maximum daily doses of paracetamol should be reinforced, along with avoiding use of other products containing paracetamol. Side effects and their management There are unlikely to be any side effects with Paracetamol taken at the recommended dose. Ref: Prodigy http://prodigy.clarity.co.uk/sore_throat_acute/management/scenario_management/management_admission_not_required/prescribin g_an_antibiotic/additional_information#-328994 d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 29 of 39 13 THREADWORMS Definition / Criteria Enterobius vermicularis (threadworm) infection Criteria for inclusion Adults and children (over 2 years) with identified threadworm infection Patients not registered with an GP within the scheme Criteria for exclusion Patients under 2 years Pregnant and/or breastfeeding women Patients unsure if it is threadworm infestation Those taking cimetidine Action for excluded patients and non-complying patients Referral to General Practitioner When and how to refer to GP Rapid referral: Heavy cases or persistent cases Conditional referral: On 3rd occurrence Consider supply, but patient should be advised to make an appointment to see the GP: Other type of worm infection Perianal itching in adults (possible differential diagnosis) If there is any other on-going concern Recommended treatments, route and legal status Frequency of administration and maximum dosage Mebendazole (OVEX®) 100mg PO P One tabled chewed or swallowed whole [1 or 4 tablet pack as necessary] Follow-up and advice Advise if symptoms do not resolve within 7 days to make an appointment to see a GP Pregnant and /or breastfeeding women to follow hygiene advice for 6 weeks Repeat after two weeks if necessary All family members should be treated Importance of personal hygiene should be stressed (Issue PIL) Side effects and their management Rarely abdominal pain, diarrhoea, hypersensitivity reactions. Reassure patient d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 30 of 39 14 VAGINAL THRUSH Definition / Criteria Vaginal Candidiasis (Thrush) Criteria for inclusion Adult females presenting with: Symptoms of vaginal thrush Who have had a previous diagnosis of thrush Who are confident this is a recurrence of the same condition And consent has been given Criteria for exclusion Patients under 16 years or over 60 Patients unsure if this is thrush Patients not registered with an GP within the scheme Known hypersensitivity to the drug or any other ingredient in the product. Pregnancy No previous diagnosis by GP Recurrent (more than 2 episodes in 6 months) See individual products for additional exclusion criteria Action for excluded patients and non-complying patients Referral to GP When and how to refer to GP Rapid referral: Presence of loin pain, abdominal pain or fever Blood present in discharge Offensive smelling or coloured (other than colourless or white) discharge Irregular vaginal bleeding Severe infection Regular attack more frequently than twice in the previous six months Diarrhoea, nausea or vomiting Ulcers or blisters on the vagina or vulva Treatment failure (7 – 14 days following treatment for same symptoms) Conditional referral: Refer on 3rd recurrence within six months Consider supply, but advise patient to make an appointment to see the GP: Post menopausal women Consider undiagnosed diabetes in at risk patients Patients with diabetes – could be a sign of poor diabetes control If there any other ongoing concern Special considerations / concurrent medication Diabetic patients Patient taking antibiotics Patient taking immunosuppressants or oral steroids Recommended treatments, route and legal status Frequency of administration and maximum dosage Clotrimazole Cream 1% 20g Route pv Clotrimazole Pessary 500mg pv Legal Status Dosage GSL Apply thinly to the area 2-3 times a day and rub in gently GSL Insert pessary into the vagina at night using d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 31 of 39 Clotrimazole Combi Pack (500mg pessary + 1% cream) Fluconazole capsule 150mg (not for use in nursing mothers) pv GSL oral P the applicator provided Instructions as per above for cream & pessary One dose Follow-up and advice Explain treatment and course of action Advise patient that any sexual partners should be treated concurrently if symptomatic Advise patient not to exceed the stated dose Advise patient to avoid use of vaginal deodorants and scented soap etc If condition worsens or symptoms persist beyond 7 days then seek further medical advice All severe adverse reactions, including anaphylaxis, should be reported to the MHRA via the yellow card system and recorded in the medical records. Verbal information should be provided to patients / carers and, if requested, written information in the form of a patient information leaflet should be given. Avoid highly perfumed soaps, bubble baths & vaginal deodorants. Wear loose fitting cotton underwear. Keep genital area cool. Remind your doctor that you are prone to thrush if they are prescribed antibiotics or other medication. Advise to discuss with sexual partners and consider treating concurrently The treatment may damage latex condoms and diaphragms Side effects and their management Sensitivity to imidazoles Occasional local irritation Drug interactions – pharmacist should consider interactions, for example with anticoagulants, some antihistamines, tranquilizers, statins etc d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 32 of 39 15 VERUCCAS AND WARTS Definition / Criteria Warts on the foot caused by human papilloma virus (Verruca) Criteria for inclusion Adults and children Criteria for exclusion Uncertain diagnosis of verruca / Wart Sensitivity to salicylic acid preparations Patients not registered with an GP within the scheme Action for excluded patients and non-complying patients Referral to General Practitioner When and how to refer to GP Rapid referral: Multiple, debilitating verrucas / warts Conditional referral: On 3rd occurrence Consider supply, but patient should be advised to make an appointment to see the GP: Verrucas / warts are very painful Severe inflammation of surrounding skin Suspected alternative diagnosis If there is any other on-going concern Recommended treatments, route and legal status Frequency of administration and maximum dosage Salatac Gel 8g Apply P Apply daily Follow-up and advice Remove film from previous application before applying Verrucas / warts may regress on their own Care should be taken to avoid treating normal skin Side effects and their management Irritation to normal skin d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 33 of 39 Minor Ailment and Community Pharmacy Scheme Reception Protocol For patients making an appointment by telephone or in person at the surgery 1. If the patient is telephoning a request and practice policy allows you to enquire about the nature of the requested appointment then use this opportunity to tell the patient that if their appointment is for one of the minor ailments they can use the new scheme in operation. If practice policy does not allow you to question the nature of the appointment then you may read out the list rather than asking directly what their appointment is for. 2. If the patient is presenting in person show them the list of minor ailments, asking if their request for an appointment is for one of the listed ailments. Inform them that there is a new scheme in operation “Minor Ailments in Pharmacies” where patients can be referred to a local Community Pharmacy for advice and treatment rather than waiting for an appointment. If the patient is exempt from prescription charges then the medicines will be free. If the patient pays for prescriptions the patient can go to the pharmacy and purchase a medicine in the normal way. (This will usually be less than a prescription charge). 3. If the patient is present at the surgery and accepts transfer into the scheme they should be given a minor ailments patient information leaflet and asked to present this at a participating pharmacy. The leaflet should be stamped with the practice stamp on the back and the patients’ details filled in by the surgery staff before issuing to the patient. For patients who decide to go to the pharmacy following a telephone request for an appointment: if they are not known to the pharmacy they will need to prove that they are registered with a participating GP practice by taking some form of identification and proof of GP registration (eg NHS card) with them. The pharmacy may contact the practice to confirm registration. 4. If a patient is referred to the pharmacy for treatment through the scheme, it is good practice to record this in the patients’ notes or computer record and read codes for the service are available on most clinical systems. Alternatively, this can be done upon receipt of a Pharm. form, which will be sent to the practice by the pharmacy when a registered patient uses the scheme to obtain treatment for a minor ailment covered by the scheme. For good practice the form should be scanned into the patients’ record. 5. If a patient refuses transfer into the scheme then an appointment should be made for them in the surgery in the usual manner. For patients self-referring at the Pharmacy The pharmacist is required to confirm the patient’s identification and registration with your surgery. If the pharmacist does not know the patient or does not have a previous d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 34 of 39 prescription record for them, then they may ring the surgery to check they are registered. Please co-operate with these requests. Referral On some occasions the Pharmacist may consider that the patient needs to be seen by a doctor. The urgency will depend upon the symptoms. In these circumstances the Pharmacist will advise the patient to make an appointment and indicate an appropriate time period for the patient to be seen by their Doctor, for example the same day for more serious conditions, within 2-3 days for less serious conditions or within the next 2 weeks if symptoms persist. Sometimes if the surgery is closed the Pharmacist may advise the patient to call the emergency number or go straight to A&E. The pharmacist will complete a referral form and give this to the patient to bring to the surgery. If an urgent appointment is required, the pharmacist will phone the surgery to arrange this. d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 35 of 39 Minor Ailment Scheme in Pharmacies Pharmacy Protocol Role of the Pharmacist and supporting staff Each patient should receive the Minor Ailments Pharmacy Patient information leaflet. If they have not already got one please give them a leaflet at this stage to allow them to understand the scheme 1. The client presenting for a Minor Ailment Pharmacist Advice Request must be seen by the Pharmacist. 2. Ensure that some evidence of registration with the named GP practice is shown. This can be a medical card, a tear-off slip from a previous prescription or if referred from the practice a stamped Minor ailments leaflet. Confirmation of patient registration may be obtained directly from the practice if required. 3. Ascertain whether the referral is from the practice (they may or may not have a stamped Minor Ailments Leaflet) or Self-referral. 4. For patients who go to the pharmacy following a telephone request, if they are not known to the pharmacy they will need to prove that they are eligible for the scheme by taking some form of identification, proof of GP registration with them and proof of exemption from prescription charges. Confirmation of patient registration may be obtained directly from the practice if required 5. During the consultation with the client complete the Pharm Claims Pro-forma 6. If a medicine is to be supplied, complete the section of the form detailing the name and the quantity supplied (Refer to formulary if in doubt as these are the only medicines that will be reimbursed) 7. Following transfer into the scheme it is good practice to record this in the Patient Medication Records For patients self-referring at the Pharmacy The pharmacist is required to confirm their identification and registration with your surgery. If the pharmacist does not know the patient or does not have a previous prescription record for them, then they may ring the surgery to check their registration. Please cooperate with these requests. Referral On some occasions the Pharmacist may consider that the patient needs to be seen by a doctor. The urgency will depend upon the symptoms. In these circumstances the Pharmacist will advise the patient to make an appointment and indicate an appropriate time, for example the same day for more serious conditions, within 2-3 days for less serious conditions or within the next 2 weeks if symptoms persist. The pharmacist will complete a referral form and give this to the patient. If urgent the pharmacist may phone the surgery to arrange referral. Sometimes if the surgery is closed the Pharmacist may advise the patient to call the emergency number or go straight to A & E. d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 36 of 39 Minor Ailments and Community Pharmacy Scheme Pharmacist Referral Form Dear Patient, Your pharmacist has reviewed your symptoms and feels that you should see your doctor for further advice or treatment. Please take this form and show it to your doctor. Your pharmacist will advise you how quickly you should see your doctor and help you make arrangements if you need to be seen quickly. Patients Name: ………………………………………………………………................ Date of Birth: …………………………… Patients Address:……………………………………………………………….…………… …………………………………………. ………………………………………………………………………………………………… Postcode: …………………………. GPs Name: ……………………………………….… GP surgery: ……………………................................................................ Symptoms reported: ..................................................................................................................... ……………………………………………………………………………………………………………….. Reason for referral…………………………………………………………………………………………………. …………………………………………………………………………………………………………………………… Has any medicine been supplied: Yes No How soon does the patient require to be seen □ Immediately (pharmacist to phone the surgery to arrange) Appointment date:…………………………. Appointment time:…………………… □ Next routine appointment Pharmacy stamp Name of pharmacist referring: ……………………………………………..…………. Contact telephone number: ……………………………………………………………. Date of referral: ……………………………………………………………………………. d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 37 of 39 Identification of a Named Professional Lead in the Minor Ailments Scheme Name of professional lead Profession .............................................................................................................. ............................................................................................................................................... I agree with the terms laid out in the service specification and I am happy to take the professional lead on the Minor Ailments Scheme for this practice/pharmacy. I will keep all staff (including any locum staff) informed of the protocol and all relevant documentation and I will provide updates following any amendments. Where necessary I will either provide training or highlight any training requirements to the Member Support Team at Solihull CCG. Pharmacists must ensure that they are competent to undertake the professional elements of the scheme. Refresher training is available as a CPPE package entitled “Minor Ailments”. It is essential that the pharmacists participating in the scheme are covered by professional indemnity insurance before they begin to participate. The pharmacist must ensure that the patient declaration is completed correctly. Reimbursement of the pharmacist for the cost of the product will be dependent on the submission of a fully completed declaration. Incident Reporting Forms should be used to inform Solihull CCG Member Support Team immediately of any incidents regarding the scheme. All complaints should be directed to the relevant Practice Manager in the first instance, who will then liaise with the Member Support Team at Solihull CCG. Signature .............................................................................. Date ………………………………………. Practice/Pharmacy stamp: d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 38 of 39 Minor Ailments Scheme Patient contacts surgery for appointment or enquires about the service Telephone Call Patient calls into surgery Patient self-referral to participating pharmacy If the patient says they have at least one of the minor ailments and is registered at the practice, they will be given an information leaflet and/or an explanation of the service and informed of the nearest participating pharmacy. They are given the option to take part Patient not happy to take part Appointment arranged with GP as usual Patient happy to take part The receptionist will provide a stamped “Minor Ailments” leaflet to the patient Patient visits participating pharmacy where they are asked for proof of registration at surgery. (see scheme details) The service is then explained to them and they will be asked to register with the pharmacy to use the scheme. A stamped “Minor ailments” leaflet will be provided if they do not already have one. Pharmacist carries out consultation and patient describes symptoms Pharmacist gives advice only Pharmacist gives advice and treatment Pharmacist refers back to GP Pharmacist and Patient complete Pharmacy proforma and exemption declaration where appropriate. Pharmacist completes PMR and labels item(s) supplied where appropriate. Pharmacist should ensure that top copy of proforma is sent to the GP as soon as possible At the end of the month, pharmacist completes monthly summary sheet and returns it, along with copies of Pharmacy proforma to Medicines Management Team at CCG. GP is also sent list of their patients registered with the pharmacy. d:\106766851.doc Solihull CCG: Treatment of Minor Ailments in Community Pharmacies (Dec 2012) Page 39 of 39