Part II
Hospital part II OCT 4- oct 25
*****INSERT: Health Services Restructuring
Commission.,Regional Pharmacy Models in Canada-
Overviews of Findings handout, Table II Comparative key indicators across existing regions. Facilities, People and Drugs handout. Hospital Systems – Medications Errors article
**********************Sept. 27/2002
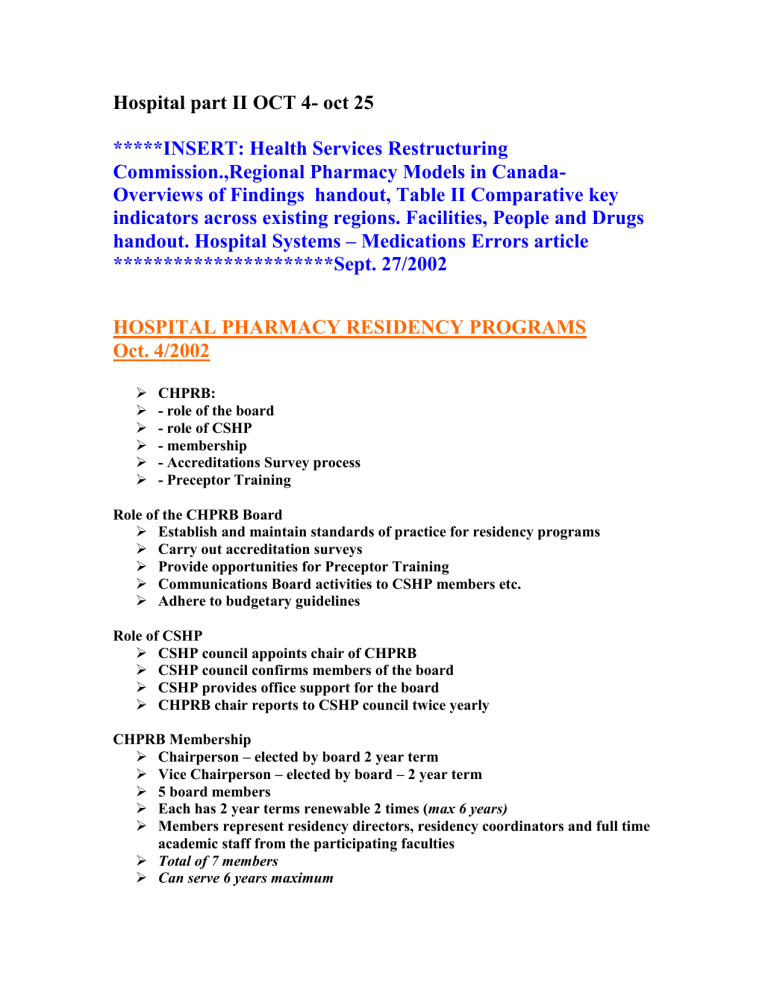
HOSPITAL PHARMACY RESIDENCY PROGRAMS
Oct. 4/2002
CHPRB:
- role of the board
- role of CSHP
- membership
- Accreditations Survey process
- Preceptor Training
Role of the CHPRB Board
Establish and maintain standards of practice for residency programs
Carry out accreditation surveys
Provide opportunities for Preceptor Training
Communications Board activities to CSHP members etc.
Adhere to budgetary guidelines
Role of CSHP
CSHP council appoints chair of CHPRB
CSHP council confirms members of the board
CSHP provides office support for the board
CHPRB chair reports to CSHP council twice yearly
CHPRB Membership
Chairperson – elected by board 2 year term
Vice Chairperson – elected by board – 2 year term
5 board members
Each has 2 year terms renewable 2 times (max 6 years)
Members represent residency directors, residency coordinators and full time academic staff from the participating faculties
Total of 7 members
Can serve 6 years maximum
Pharmacy Residency Forum of Ontario
Coordinates program s in Ontario
Membership includes residency directors, residency coordinators, representative from OPRA, faculty liaison and Residency selection coordinator
Activities include coordination of residency activities including selection process
Ontario Pharmacy Residents Association
Represents the residents enrolled in programs
Includes hospital, community and industrial
Communicate with members
Organize educational events
Attempt at national membership bid failed because difficulty to organize
CHPRB Standards
Residency program requirements o General education approach o Assessment of residents learning o Pharmacy practice rotations o Communication and research skills o Program completion
Purpose of residency programs o To provide an experiential learning environment using pharmacy practitioner role models so the necessary skills, knowledge and values can be acquired and applied by the resident in the provision of exemplary patient care o To develop competent and progressive pharmacy practitioners in health care organizations and encourage future leaders for the profession
Qualifications o Health care organization o Program direction o Preceptors o Residents o Also used as a recruitment tool o Most residents are offered jobs at least 6 months into the program
Pharmacy practice rotations
Direct patient care (focus of all rotations)
Drug distribution and intravenous admixtures
Drug information and literature evaluation
Practice management and drug use control
Research project
Aka administrative rotations
Accreditation Survey Process
Each program is survey every 4 years or sooner if deemed necessary
Two members of board conduct an on-site visit to evaluate the program against the standard
A verbal report is provided at the time of the visit but no recommendations are given
A written report is provided ot the program within 30 days which will contain any recommendations
The program is given 60 days to respond to any recommendations
Report and response are discussed at next CHPRB meeting and an accreditation award is given
Recommendations o Recommendations based on standards
Accreditation award is directly related to the number and seriousness of the concerns o Consultative recommendations
Recommendations about some factors that may help to improve the delivery of the program but are not directly related to the standards
Do not affect the accreditation status
Ie. Phmt shortage (no DI phmt)
Too many recommendations and the hospital won’t get accredited
Accreditation Awards o Accreditation o Accreditation with progress report at 2 years o Accreditation with progress report at 1 year o Not a good report
at risk of getting pulled o Accreditation is time to fix mistakes o Status is based upon how the program meets the standards o Not dependant on whether meet recommendations o Standards
not consultative recommendations
Structure of Residency Programs
Program Director – usually the director of pharmacy
Program coordinator
Individual resident coordinator (optional)
Preceptors
Residency advisory committee
Residency Advisory Committee
Oversees the program to ensure effective operation
Provides guidance to the program and to the residents
Act as as a source for quality improvement ideas
Support for project
Membership (variable) o Program director and coordinator o Hospital administrator o Nurse o Physician o Faculty liaison o Preceptors
Preceptor Training
CHPRB seminars q2yr
On the job by residency coordinators
Preceptor guide
Qualifications and requirements of a preceptor
Assessment, feedback and evaluation
Mentoring and motivating residents
Challenges to preceptor
Dealing with residents in difficulty
Qualifications
Broad knowledge base
Desire to learn and teach
Challenge resident to think logically and critically
Assessment Feedback and Evaluation
Learning portfolio
Self-assessment
Providing feedback
Evaluating the resident
Mentoring and Motivating
Mentor is a person who unselfishly serves as a wise and trusted counselor
Motivating the resident o Motivation comes from within o Preceptor can maximize motivation by guiding and challenging resident but not by overloading and overwhelming them
Leaders are learners who are willing to take risks and learn from their mistakes
Challenges to Precepting
Interpersonal conflicts between the preceptor and the residents
Attitude
Behavior
Competency
Dealing with Residents in Difficulty
When preceptor recognizes the problem they should deal with the problem quickly with the help of the coordinator
Timing of the evaluation is crucial
Develop a plan of action
Follow up
************INSERT: Oct 04.02 accreditation standards Introduction handout ,
Assessment, feedback and evaluation handout too***************************
HOSPITAL ACCREDIATION OCT 11, 2002
Overview
Why have accreditation
Voluntary (unlike OCP regulation)
Does pharmacy have anything comparable
CCHSA as a process model o Theory and process o Elements for evaluation o Self assessment tool o Standard 15 (medication) o Strengths/weaknesses
What evaluation tools are available to the profession of pharmacy?
OCP
Regulatory, mandatory
Standards of practice
Community pharmacy accreditation
Backed up by inspection and enforcement
QA program for pharmacists
CSHP
Voluntary standards
No enforcement
Other
Faculty and residency accreditation
Specialty organizations
Consultants
Networks
MOTIVATION = Desire to know we are doing the right thing PLUS Desire to keep improving
Accountability through
Self examination and reflection
Peer review
External expert review
Benchmarking against standards
Use of CQI strategies
CCHSA process provides a model for this
CCHSA Mission
The mission of CCHSA is to promote excellence in the provision of health care and
The efficient use of resources
In health organizations throughout Canada
For the benefit of Canadians
CCHSA AIM: “ACHIEVING IPORVED MEASUREMENT”
Quality Dimensions and Descriptors
1.Client and community
Responsiveness
Confidentiality
Participation and partnership
Respect and caring
Involvement in the community
2.Work Life
Open communication
Role clarity
Participation in decision-making
Learning environment
Well being
3.Responsiveness
Availability
Accessibility
Timeliness
Continuity
Equity
4.System competency
Appropriatness
Competence
Effectiveness
Safety
Efficiency
Alignment between organization and programs
Elements of a CCHSA survey
Pre-survey documents
On-site documents
Quality indicator data
Self-assessment
Team interviews
Client interviews
Focus groups
Tours
Teams
Leadership and partnership
Environment
Human resources
Information management
Patient care
Patient Care Standards
Individual and population
Assessment
Diagnostic servies
Providing information
Consent
Ethics
Rights and responsibilities
Cycle of planning and providing
Standard 15: Medication
The use of medication is safe, efficient, effective and promotes the best possible QOL
Review Rxs to make sure they are accurate
Fill Rxs and dispense medications in a timely, accurate way
Store medications in a way that is safe and secure
Prevent, monitor and promptly respond to any adverse effects resulting from their use
15.2 Clients receive written and verbal feedback about the…
Medications and other therapeutic technologies that are available
Potential benefits and adverse effects
The risks of not complying with instructions
15.3 The team has access to current information, advice and support about using medication and other therapeutic technologies
15.4 The use of medication and other technologies
Meets legal requirements and standards of practice
Is monitored and reported through an ongoing utilization review
15.5 The organization monitors the quality of its pharmacy services by
Carrying out an internal quality control program
Participating in external quality control or accreditation
Continually reviewing and improving performance as part of a QI process
Accreditation process: Strengths and Weaknesses
Accreditation process Strengths
Comprehensive
Consistent
Objective
Shared expertise
Educational process
Structure, process and outcome based
Team building opportunity
public seal of approval
second d set of eyes (outsider) to critique
QI emphasis- ids areas for improvement
Ids areas of excellence
Validated through multiple strategies
Holds hospitals accountable
Source of pride and celebration
Process Challenges
Expensive
Labor intensive
Self-assessment- how honest?
Standards vague and repetitious
Agreement on standards?
Stressful
Surveyor variability – bias, expertise
Worth the effort?
****INSERT: “value of pharmacists’ services handout Oct 11, “ The value of Your services” article Oct 11.02, **********************************************
OCT 18 TH
FRAN PARADISO – HARDY
OPPORTUNITIES FOR PHARMACISTS IN THE CARE OF THE CV PATIENT
(CLASS NOTES)
Cv disease complex, costly, prevalent
Clinics ambulatory o Cardiac rehab o Chf
Inpatient: warfarin dosing
Cath lab
Administrative
o Involvement in CV drug use/outcomes programs or QC activities
(standard orders, hospital guidelines, heparin nomograms) o Written DI monographs
*** INSERT: “seamless Care workshop” article Oct 18, 02 Jim
Mann*************