File
advertisement

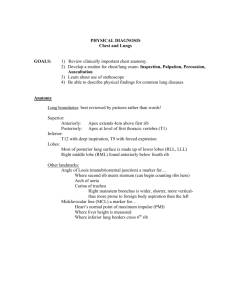
1 1/11/08 Phys Dx II – exam 1 Respiratory System Exam Respiratory System Exam -Part of a Complete Physical Exam -Symptoms/Complaints -Risk Factors Respiratory System Symptoms Cough Productive vs Non-productive (sputum production) Hemoptysis (coughing up blood) Dyspnea (SOB) Wheezing Cyanosis Chest Pain Stridor (noisy breathing) Voice changes (vocal cords) Swelling of ankles (dependent edema) Sleep Apnea Relevant History Employment (exposure to irritants) Home environment (allergens) Flame-retardants (esp. w/ infants) Tobacco (pack yrs= #yrs x #packs/day) Exposure to respiratory infections Nutritional status Obese are more prone to infections Travel Exposures Hobbies (exposure to resp. irritants) Use of alcohol Use of illegal drugs Exercise tolerance Immunizations (TB) Current chest x-rays Respiratory System Risk Factors Gender: > males (partly due to work environ.), gender difference decreases w/ aging (due to pulmonary edema) Age: increases with advancing age Family Hx: Asthma, CF, TB, other contagious ds, neurofibromatosis Smoking Sedentary life-style / immobilization (couch-potatoes have a greater risk for infection) Occupational exposure -dental problems are the most common cause of lung abscesses Extreme obesity -warm humidity helps to open airways and stop coughing, and then Difficulty swallowing cold air helps to sooth tissues Weakened chest muscles -in early stage CHF, people cough lightly when in the supine Hx. of frequent respiratory infections position Severe cardiovascular disease Coughing Onset Palliative/Provocative Quality (Nature of cough) Severity Pattern Associated Symptoms Treatment (type, effect) Descriptors of Coughing (table 13-1) Dry, hacking (virus, allergy) Chronic (bronchiectasis) productive Wheezing (asthma, allergy, CHF) Barking (croup – epiglottal dx) Stridor (tracheal obstruction) Appearance of Sputum (table 13-2) Mucoid (asthma, TB, emphysema) Mucopurulent (asthma, TB, emphysema) Yellow-green/ purulent (bronchiectasis) Rust-colored/ Purulent (pneumococcal pneumonia) Morning (smoking) Nocturnal (CHF, postnasal drip) Assoc. w/ eating or drinking (NMS dx of upper esophagus) Inadequate (debility, weakness) Red currant jelly Foul odor (lung abscesses) Pink, blood-tinged (strep or staph pneumonia) Pink, frothy (pulmonary edema) Profuse, colorless (alveolar cell carcinoma) Bloody 2 Hemoptysis (table 13-3) Onset (sudden, recurrent) Descriptor (blood tinged, clots) History of smoking, infections, meds, surgery, (females - oral contraceptives) Associated symptoms Hemoptysis vs Hematemesis Hemoptysis = coughing blood -possible history of cardiopulmonary disease -pink and frothy sputum; mixed with pus -dyspnea Hematemesis = vomiting blood -possible history of GI disease -not frothy sputum; mixed with food -dark red, brown, or “coffee grounds” -nausea -college students are most prone to mycoplasms and viral pneumonias -TB – later: night sweats, weight loss, fatigue, fever -asthma – thick mucoid sputum (hard to expectorate) 1/14/07 Dyspnea (SOB) (table 13-8) Dyspnea on Exertion (DOE) Onset (when, mode, progression) Palliative Provocative (exertional, positional) Pattern Associated symptoms Associated conditions Grading 1-5 (1st establish a baseline) 1- Excessive activity 2- Moderate activity 3- Mild activity 4- Minimal activity (ie dressing oneself) 5- Rest Common Conditions Associated with Dyspnea (table 13-8) Asthma – episodic attacks, wheezing, chest pain, productive cough (thick, mucoid, hard to expectorate the sputum) Pneumonia – insidious onset of dyspnea, cough Pulmonary edema – abrupt; tachypnea, cough, orthopnea, nocturnal dyspnea (positional dyspnea) Pulmonary fibrosis – progressive, tachypnea, dry cough Pneumothorax – moderate to severe dyspnea, sudden pleuritic chest pain -spontaneous pneumothorax occur in healthy, thin, young males (bleb that ruptures) Emphysema – insidious onset, severe dyspnea; cough Chronic bronchitis – chronic productive cough Obesity – exertional dyspnea Dyspnea of Rapid Onset (within 24-hour period) Pneumonia Pneumothorax Pulmonary Constriction Peanut (or inhaled foreign object) Pulmonary Embolus Pericardial Tamponade Pump Failure (CHF) Peak seekers (high altitudes) Psychogenic (anxiety) Poisons Wheezing & Noisy Breathing Wheezing: Abnormally high-pitched suggest bronchiospasm or compression Rhonchi: Harsher sounds suggesting secretions in larger airways. Stridor: Harsh wheeze entirely or predominately in inspiration which suggest partial obstruction of larynx or trachea Causes of Wheezing or Noisy Breathing Infections (can lead to edema &/or mucus production) Irritants & Allergens Compression of the Airway (ie tumors, aneurysm) Congenital Malformations/Abnormality (ie atresia) Acquired Abnormalities at any level of airway (tumors, stenosis) Neurogenic Disorders (something that can affect the diaphragm, ie phrenic nerve pblm) 3 **Positional Dyspnea (page 369) – table 13-4 Paroxysmal nocturnal dyspnea (PND) Sudden onset occurring while sleeping, relieved by assuming upright position (CHF) Orthopnea – lying flat requires multiple pillows (CHF, mitral valvular disease) Trepopnea – more comfortable on side (in later stage CHF) Platypnea – problems sitting up, patient breaths easier in recumbent position (neuro ds., hypovolemia, cirrhosis) Cyanosis (Bluish Discoloration) Central – cardiorespiratory pblm Dec. O2 in lungs Severe C/R ds. Lips, oral mucosa, nail beds Gets worse with warming of body Peripheral – venous stasis Venous Stasis Exposure to cold Nail beds, nose, lips Cyanosis decreases with warming Chest Pain OPPQRST & Assoc Sx, Treatments Differential: Cardiovascular Respiratory (Pleural involvement) Gastrointestional (esophageal pblms) Chest Wall Syndrome Psychogenic -likely not a heart attack, unless pt. is diaphoretic Chest pain – Tracheobronchitis -Inflammation of trachea & large bronchi associated with upper sternal and/or parasternal pain Quality: burning Associated symptom: coughing Provocative: unfortunately coughing Palliative: lying on the involved side may provide relief Chest Pain – Pleural -Inflammation of the parietal pleura (pleurisy, pneumonia, neoplasm, or pulmonary infarction) -Constant pain of the chest wall overlying area of involvement Quality: sharp and stabbing, often severe Provocative: breathing, coughing, movements of the trunk Apnea - The absence of spontaneous breathing Deglutition – apnea during swallowing is a normal response Primary – if a person has fallen or got hit in the chest (wind knocked out of you) – not an abnormality Reflex – not an abnormality (ie strong odors, like sulfur) Secondary – IS an abnormality (damage to respiratory centers, MI, stroke, etc) – pt. needs resuscitation Selective – when person selectively decides to hold breath (ie diving into water) Sleep – biggest concern with patients (even 10 seconds can have deleterious effects) Multiple causes: often cardiovascular pblm, obesity (fat in airways), or incr intracranial pressure (but mostly idiopathic) If obese, losing weight or exercise often will get rid of sleep apnea 1/15/07 Examination Sequence Peripheral Assessment Inspection of Chest & Thorax Palpation Percussion Auscultation Peripheral Signs Posture Facial Expression Use of Accessory Respiration Muscles Clubbing of Nails (pg 376) Cyanosis (central) 4 *Sweet, fruity – diabetic ketoacidosis; starvation ketosis *Ammonia-like – uremia *Foul, feculent – intestinal diverticulum *Cinnamon – pulmonary TB Clover – hepatic failure Clubbing of Nails – chronic hypoxia -Intrathoracic tumors -congenital heart malformations -mixed venous-to-arterial shunts -Acquired cardiopulmonary disease -chronic pulmonary disease -chronic hepatic fibrosis Inspection of the Chest/Thorax Note Shape & Movement of Chest Observe Effort of Breathing Rate, Rhythm, Depth, Audible sounds Note Any Skin Lesions Slope of Ribs and Motion Symmetrical with no retraction or lag (retraction=sucking in; lag=decr motion) Accessory resp muscles - contraction of scalenes and SCM - after scalenes and SCM tires, patient sits with hands on thighs and pushes off a little as breath in - flaring of nostrils, pursing of lips - pushing against chest wall to aid in exhaling More than 5mm of movement of clavicles during resting respiration indicates a problem *anatomy of respiratory system* -sternomanubrial angle (2nd rib) -angulation of ribcage of anterior vs. posterior -ribs become more horizontal as chest expands -lungs rise 1-1.5” above inner 1/3 of clavicle -6th rib on anterior aspect, 10th SP on posterior -rt/left midclavicular lines (at nipples) & midsternal line -ant/post axillary lines & midaxillary line -midspinal line & midscapular lines -major (oblique fissure) at SP of T3 -descends obliquely down to the 6th rib midclavicular line -horizontal fissure – from 5th rib to sternum *-rt middle lobe – from 5th rib (midaxillary) to 4th rib at sternum to 6th rib (midclavicular line) **know anatomical landmarks of lung lobes Ds. of Chest Expansion/Lag Chronic fibrotic disease (lung or pleura) Pleural effusion Pneumothorax Lobar pneumonia Pleural Pain (splinting) Unilateral bronchial obstruction Palpation of the Chest/Thorax Tender areas Evaluate skin lesions, abnormal bulges or depressions Determine tracheal position Assess chest expansion (rib excursion) Tactile (vocal) fremitus Estimate level of the diaphragm 5 -barrel-shaped chest is normal in infants -Pectus Excavatum (funnel-shaped chest) – depression of lower portion of sternum -poor posture & pot belly -may lead to compression of great vessels & heart murmurs -Marfan’s is classically associated with pectus excavatum (& Rickets in third-world countries) -Pectus Carinatum (pigeon chest) – sternum is displaced anteriorly -costocartilage adjacent to the sternum are depressed -severe scoliosis can lead to this -used to be a classic distortion in children with asthma Multiple displaced rib fractures (traumatic flail chest) -patient should sleep with pillow b/n arm and chest wall (patient should sleep on back, not on side) Ds. Of Chest expansion/Lab (B/L) -chronic fibrotic disease (lung/pleura) – B/L -obesity -COPD -Ascites – organomegaly -Diaphragmatic disease Respiration - rate, rhythm, depth Ds. of Chest Expansion/Lag (U/L) Chronic fibrotic disease (lung or pleura) – U/L Pleural effusion (fluid accumulates in lowest portion of pleural space) Pneumothorax – air in pleural space Lobar pneumonia – fluid accumulation Pleural Pain (splinting) Unilateral bronchial obstruction Normal adult resting respiration: 10-20 breaths/min, regular rhythm, relaxed with no use of accessory muscles 4:1 ratio with heart rate Respiration Terms Bradypnea: <10 bpm (well-conditioned athlete) -incr intracranial pressure (headache), neoplasia, aneurysm, head trauma (subdural hematoma) Tachypnea: >20 bpm & shallow (rib fracture) -pleural involvement (pleurisy) Hyperpnea: deeper & more rapid -stress, exercise, anxiety -Kussmaul (rapid, deep, labored) -metabolic acidosis (diabetes, kidney failure) Apnea: temporary halt in breathing Chest Expansion Posterior: 3-4 cm on inspiration @ T10 Anterior: Apex - symm. slight motion, Upper lobe ribs 2&3 -- 1-2 cm Lower lobe ribs 5&6 -- 2-3 cm Lateral: Depends on levels -sighing respiration – anxiety, boredom -air trapping – classic for COPD -Cheyne-Stokes – classic for CHF (or drug-induced respiratory depression) Influences Rate & Depth of Breathing Increases with: Acidosis, CNS lesions-Pons, anxiety, pain, hypoxemia, aspirin poisoning Decreases with: Alkalosis, CNS-cerebrum, severe obesity, myasthenia gravis, narcotic overdose 6 Palpation of Chest/Thorax -tender areas -evaluate skin lesions, abnormal bulges or depressions -determine tracheal position (place fingers on either side of tracheal, but medial to the SCM) -it is not uncommon for there to be slightly less left spacing than right (mediastinum) -also, it should move freely -assess chest expansion (rib excursion) -tactile (vocal) fremitus -estimate level of the diaphragm Tender regions -palpate for tender areas on the chest wall or thorax using ulnar surface of hand, MCP joints or distal pad of your fingers. -skin changes or lesions should be further delineated and defined Tracheal Deviation *Pulled: Open pneumothorax, Fibrosis, Atelectasis (upper lobe), infiltrative tumor, pneumothorax *Pushed: Tension pneumothorax, Tumor, Thyroid or lymph node enlargement (Hodgkin’s), Pleural Effusion Pushed posterior: Mediastinal tumors, goiter Pushed anterior: Mediastinitis 1/18/07 Tactile (Vocal) Fremitus Palpable or auditory vibration of the chest wall resulting from speech or other verbalizations. “99”, “1,1,1” Ulnar surface of the hand, MCP, Pads Simultaneous or Alternating side to side, down and across -most cancers are small masses and will not alter our exam findings 7 *Table 13-5. Changes in Tactile Fremitus (sound transmission) -anything that causes the parenchyma to become more solid, transmits more sound (ie lobar pneumonia) Increased tactile fremitus: pneumonia, atelectasis that is close to the main stem bronchus (rare) Decreased tactile fremitus: U/L: pneumothorax, pleural effusion, bronchial obstruction, atelectasis (incomplete expansion of lung tissue) B/L: chronic obstructive lung disease, chest wall thickening (muscle, fat) Estimate Level of Diaphragm Approximation through Tactile Fremitus Abnormally high diaphragm: Pleural Effusion Paralysis of Diaphragm Organomegaly Atelectasis (Lower lobe) – absorbs the sound rather than transmit it Pregnancy -start at inferior level of scapula and have patient say “99” – diaphragm should be around the T10 level Percussion Creates sound waves that travel inward 5-7 cm (assesses a superficial or peripheral lesion) Percussion note (intensity, pitch, duration) Diaphragmatic excursion: change between inspiration and expiration Percussion Note (page 379) *Flat percussion note: classic for pleural effusion (or “flat to dull”) *Resonant: normal or ?tumor? *Hyperresonant: pneumonia *Dull: classic for lobar pneumonia (with consolidation) *Tympany: pneumothorax Diaphragmatic Excursion Level between the Resonance/Dullness on full inspiration vs expiration. 3-6 cm (4-5 cm according to Swartz) Depends on size and level of activity of patient (can be up to 8cm in athletes) – not concerned with incr Decrease B/L: *Emphysema, Thickened chest wall, Elevated diaphragm, Ascites, B/L Organomegaly, B/L Collapse Decrease U/L: Same conditions as Lag – U/L pleural effusion, pneumothorax, bronchial obstruction, organomegaly, consolidation (lower lobe) Absent: Inflammation of diaphragm or visceral below, Phrenic nerve palsy -sucking in stomach, sticking out chest, and throwing back your shoulders all lead to an inefficient way of breathing (using more of the accessory muscles) Auscultation Breath Sounds (type, intensity) Adventitious Sounds Vocal Resonance Bronchophony Egophony Whispered Pectoriloquy Breath Sounds Auscultation is performed in the across-down-across method 4 Breath Sounds (Note location) Tracheal (harshest – outside chest) Bronchial (over manubrium) Vesicular (periphery) Bronchovesicular (1st and 2nd intercostal spaces) 8 Tracheal – very loud harsh sound (consistent with the extrathoracic trachea); high pitch, Inspiration:Expiration ratio = 1:1 Bronchial – loud, and high pitch; I:E = 1:3 Bronchovesicular – moderate intensity & pitch; I:E = 1:1; sounds like rustling Vesicular – quiet, soft intensity, low pitch; vast majority of lung field; I:E = 3:1; gentle rustling -quieter sounds = more tissue that the sound must travel through -the same conditions that alter tactile fremitus can also alter the breath sounds -ie pneumonia (consolidation) increases the harshness Breath Sound Intensity Increase: Pneumonia w/ Consolidation (classic) Atelectasis in the Upper Lobe or adjacent to the main stem Bronchi ?Diffuse Fibrosis (depends on extent of fibrosis) Adventitious Sounds (Added) Decrease: COPD Chest wall weak Pleural effusion Pneumothorax Bronchial Obstruction Thickened Wall Superimposed on the Breath Sounds (extra sounds) Crackles (Rales) Wheezes & Rhonchi (rhonchi are harsher sounds assoc with more fluid) Pleural Friction Rub (when pleural involvement; ie pleural effusion and pneumothorax) Stridor (inspiratory harsh sound assoc with partial tracheal or laryngeal obstruction) Table 13-7. Adventitious Sounds Crackle – excess airway secretions (ie Bronchitis, infections, pulmonary edema, atelectasis, fibrosis, CHF) Wheeze – rapid airflow through obstructed airway (ie Asthma, pulmonary edema, bronchitis, CHF) Rhonchus – transient airway plugging (ie Bronchitis) Pleural Rub – Inflammation of the pleura (ie pneumonia, pulmonary infarction, pleurisy, small pneumothorax, or small pleural effusion) 1/22/08 -pleural effusion is the only condition with a transition area b/n decreased and increased tactile fremitus (?) -pneumothorax shifts the trachea to the opposite side Vocal Resonance Transmitted voice sounds “99”, “1,1,1” When abnormal breath sound is heard may help to further delineate the area. Enhance: consolidation (lobar pneumonia), airless lung Decrease: blockage of respiratory tree, or over-inflated lungs, thickened chest wall When an area of abnormality is noted during auscultation, especially bronchial breath sounds any of these tests can be used to localize the area of involvement Bronchophony – spoken words are louder, clearer, more audible Egophony – “ee” is heard as “ay” Whispered Pectoriloquy – whispered words are louder, clearer -in your office, bronchophony is the only one that needs to be tested for Table 13-9. Differentiation of Common Pulmonary Conditions Asthma – tachypnea, tachycardia, dyspnea, use of accessory muscles, often normal palpation & percussion Emphysema – stable vital signs, wasting, decr tactile fremitus, incr resonance, decr lung sounds Chronic bronchitis – tachycardia, often normal palpation & percussion, rhonchi & early crackles Pneumonia – tachycardia/pnea, incr tactile fremitus, dull percussion, late crackles Pulmonary Embolism – tachycardia/pnea, usually normal exam Pulmonary edema – tachycardia/pnea, wheezes Pneumothorax – tachycardia/pnea, inspection may be normal, absent fremitus, hyperresonant percussion -a small pneumothorax (contained) will self-resolve, even though there is a little pain Pleural effusion – tachycardia/pnea, decr fremitus, dull percussion, absent breath sounds Atelectasis – tachypnea, decr fremitus, dull percussion, absent breath sounds Acute resp distress syndrome – tachycardia/pnea, use of accessory muscles, cyanosis 9 10 *know conditions that can have BLOOD (table 7-3) – bacterial pneumonia, chronic bronchitis, bronchiectasis, TB, lung abscess, cancer, pulmonary emboli TB – cough dry or sputum that is mucoid or purulent; may be bloody Lung abscess – bloody, foul-smelling sputum GI reflux – cough Pulmonary emboli – after surgery or person with problem with venous stasis and sits a lot; may cough up blood ----------- 11 Breast Exam 1/25/08 Breast Exam -Part of a complete physical exam -Risk Factors -Symptoms/Complaints -1 in 8 women develop breast cancer *******know risk factors******** -caffeine, soft drinks, chocolate, and cheese incr breast swelling & tenderness -fibrocystic change = benign breast cancer -radiation to breast tissue leads to increased incidence of mutations occurring -diagnostic ultrasound is preferred b/c it is better at distinguishing b/n a solid and cystic mass -if hard, immobile mass or if there are lymph nodes associated with General Questions Do you perform monthly SBE Last mammogram, results History of cancer (patient or family) Breast implants, augmentation Use of birth control pills Use of estrogen replacement therapy Breast Mass(es) Location Onset (When, How, Change) Does it change with menses? Pain (tenderness) Pattern Skin Lesions, Color variations Nipple Change Symptoms/Complaints Mass or Swelling Pain Nipple Discharge/Deviation Change in Skin over Breast Breast Pain Location: Unilateral/Bilateral Any Trauma OPPQRST Change In Bra Size Pattern Associated Symptoms 12 Nipple Change Discharge Depression or inversion -Could be a tumor pulling nipple in -not problematic if nipples have always been inverted Deviation Discoloration Dermatologic changes Nipple Discharge Location: Unilateral/Bilateral Onset Describe Change/Discharge Related to Menses Medications/Oral Contraceptives Associated Symptoms Serous: thin & watery, may appear as stain: intraductal papilloma, carcinoma, b/l-oral contraceptives Bloody: Malignant intra ductal papillary carcinoma, benign IDP during pregnancy Milky: Late pregnancy, persistent lactation, pituitary tumor, certain tranquilizers (anti-psychotics) Change in Skin Over Breast Change in Color or Texture Edema Dimpling, puckering, retraction Discoloration Rash Breast Exam Procedures -Inspection -Palpation -Axillary lymph node evaluation Inspection: Breast Tissue Sitting & supine Number, size, shape, symmetry, edema, dimpling, redness, thickening of skin, prominent vessels, rashes Slight asymmetry in size is normal How to Accentuate Changes through Inspection Raise arms over head (stretches pects) Press hands against hips or pressing hands together (contracting the pectoralis muscles) Lean forward with arms outstretched from waist (looks at how breasts hang) Palpation of Breast Tissue Seated – Bimanual (looking for gross change in tissue density, retraction signs, etc) Supine - Pillow under ipsilateral shoulder (the more comprehensive exam is performed supine) Systematic palpatory approach to assess all breast tissue Optimal exam timeframe: 2-7 days after the onset of menses/month -follicular phase of menstruation (after 7 days) leads to swelling of the breasts Note consistency of tissue - Normal varies widely with physiologic nodularity noted in most women. Tenderness, masses, skin temperature If mass is noted document accordingly as follows: Documentation of Breast Mass Location: Clock (preferred method) or Quadrant method w/ distance from nipple (R or L breast) Size: Length, width, thickness Shape: Round, discoid (multiple nodules connected), lobular (fibroadenoma), stellate (irregular – not good) -Round or discoid could be gross cysts and not problematic Tenderness: Severity (unless significant lymphatic blockage, most cancers are painless) Consistency: Firm, soft (cystic – not as worried), hard (ie pebble – not good) -Could have calcified lymph nodes Borders: Discrete (good sign) or poorly defined (bad) Mobility: Movable (in what direction) or fixed to overlying skin or underlying fascia or tissue -Bad sign if fixed Retraction: Presence or absence of dimpling or altered contour If a mass is immobile with the patient relaxed, it is attached to the ribs & intercostal muscles. If a mass becomes fixed when the pt. presses her hands against her hips, the mass is attached to the pectoral fascia. -Must remove the outer portion of the pec 13 Nipple & Areola Examination Inspection: 5 D’s Palpation: note thickening, pain Gently compress or strip nipple Note any discharge Evaluate Axillary Nodes Inspection Lesions: rashes, masses Discoloration (unusual pigmentation) Palpation Location Number Discrete/Matted Size Tenderness Mobility Inspection: Nipples Size, shape, symmetry Discharge Depression or inversion Deviation Discoloration Dermatologic changes Table 16.2 -most malignancies occur in the upper outer quadrant Lymph Node Assessment Enlarged axillary nodes from infection, recent immunization, neoplasia, or generalized – check epitrochlear … Screening Guidelines (NCI) BSE should be started in early 20’s Clinical breast exam about every 3 yrs for women in 20’s & 30’s then yearly for women 40 and older. Screening mammograms every 1-2 yrs starting at age 40 every yr over 50 High risks pts personal schedule Breast Cancer in Males ~1000 men/yr in the US >300 deaths/yr due to metastatic CA Ave age of 59 y.o. 75% painless mass or nodule subareolar or upper outer quadrant M/C site of metastasizes: bone, lung, liver, pleura, lymph node, skin, brain