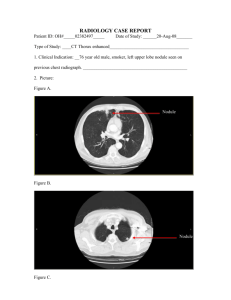
Right/Left Upper/Middle/Lower Lobe Collapse
advertisement
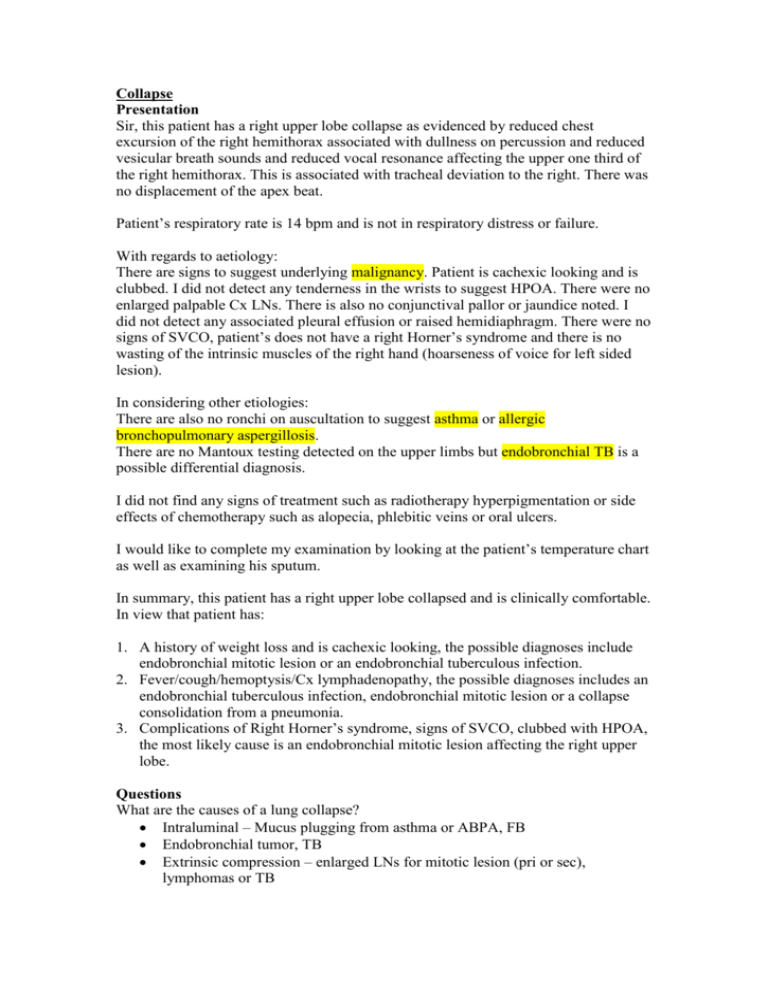
Collapse Presentation Sir, this patient has a right upper lobe collapse as evidenced by reduced chest excursion of the right hemithorax associated with dullness on percussion and reduced vesicular breath sounds and reduced vocal resonance affecting the upper one third of the right hemithorax. This is associated with tracheal deviation to the right. There was no displacement of the apex beat. Patient’s respiratory rate is 14 bpm and is not in respiratory distress or failure. With regards to aetiology: There are signs to suggest underlying malignancy. Patient is cachexic looking and is clubbed. I did not detect any tenderness in the wrists to suggest HPOA. There were no enlarged palpable Cx LNs. There is also no conjunctival pallor or jaundice noted. I did not detect any associated pleural effusion or raised hemidiaphragm. There were no signs of SVCO, patient’s does not have a right Horner’s syndrome and there is no wasting of the intrinsic muscles of the right hand (hoarseness of voice for left sided lesion). In considering other etiologies: There are also no ronchi on auscultation to suggest asthma or allergic bronchopulmonary aspergillosis. There are no Mantoux testing detected on the upper limbs but endobronchial TB is a possible differential diagnosis. I did not find any signs of treatment such as radiotherapy hyperpigmentation or side effects of chemotherapy such as alopecia, phlebitic veins or oral ulcers. I would like to complete my examination by looking at the patient’s temperature chart as well as examining his sputum. In summary, this patient has a right upper lobe collapsed and is clinically comfortable. In view that patient has: 1. A history of weight loss and is cachexic looking, the possible diagnoses include endobronchial mitotic lesion or an endobronchial tuberculous infection. 2. Fever/cough/hemoptysis/Cx lymphadenopathy, the possible diagnoses includes an endobronchial tuberculous infection, endobronchial mitotic lesion or a collapse consolidation from a pneumonia. 3. Complications of Right Horner’s syndrome, signs of SVCO, clubbed with HPOA, the most likely cause is an endobronchial mitotic lesion affecting the right upper lobe. Questions What are the causes of a lung collapse? Intraluminal – Mucus plugging from asthma or ABPA, FB Endobronchial tumor, TB Extrinsic compression – enlarged LNs for mitotic lesion (pri or sec), lymphomas or TB What is Brock’s syndrome? Collapse of the right middle lobe from enlarged LNs How would you investigate? Simple investigations o CXR o ABG, FBC and biochemical profile o Sputum AFB smear and c/s and cytology Diagnostic - Bronchoscopy and Bx Staging – CT thorax and abdomen with adrenal cuts, bone scan Physiological staging: Lung function test o FEV1 >1.5 o Transfer factor>50% How would you treat the patient? Depending on the underlying cause For mitotic lesion o Multidisciplinary approach o Education and counselling, support groups and stop smoking o Symptomatic treatment o For non-small cell Assessment for surgical resectability Staging (up to stage IIIA); ie once T4, N3 or M1 not a candidate Physiological staging Chemotherapy Neoadjuvant Adjuvant Radiotherapy Adjuvant Palliative Palliative Radiotherapy o Pain, bone mets o Dyspnea from bronchial obstruction, dysphagia o SVCO, pancoast syndrome Chemotherapy o For small cell Chemotherapy How does patient with bronchogenic carcinoma present? Primary tumor o Cough, dyspnea, hemoptysis, pneumonia Mediastinal spread o SVCO, Horner’s, pleural effusion, phrenic nerve palsy, hoarseness of voice, T1 wasting, pericardial effusion Metastasis o Liver, bone, brain, skin, adrenal glands Paraneoplastic symptoms Systemic effects o LOA, LOW, fatigue What are the paraneoplastic syndromes? Endocrine o PTH-related peptide (hypercalcemia) – SCC o SIADH – Small cell (usually asymptomatic) o ACTH – Cushing’s (usually hypokalemic metabolic alkalosis) o Gynaecomastia Neurological o Subacute cerebellar degeneration o Peripheral neuropathies o Lambert-Eaton syndrome Cardiovascular o Non-thrombotic endocarditis Renal o Nephrotic syndrome, GN (membranous) Skin o Migratory venous thrombopleblitis (Trosseau’s sign) o Acanthosis nigricans o Dermatomyositis o Zoster MSK o Clubbing, HPOA Haematological o DIC o Anaemia What is SVCO? Tumour with obstruction of the SVC Plethoric facies Facial and UL oedema Conjunctival suffusion Undersurface of the tongue with multiple venous angiomata Fixed engorgement of the neck veins Stridor Upper chest telangiectasia Radiation marks (NB think of polycythemia which also have plethoric facies) Causes o Lung carcinoma, especially small cell o Lymphoma o Others – mediastinal goitre