Ch 28 COPD
advertisement
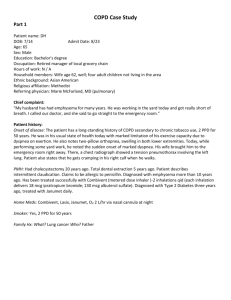
COPD Maria’s Notes Page 1 Ch. 28 Obstructive Pulmonary Disorders: Emphysema and chronic bronchitis—COPD Asthma—Christmas and Birthday disease Chronic inflammatory disorder Affects airways Causes episodes of recurrent wheezing, dyspnea, cough and chest tightness A) triggers: 1. allergens-dust animal dander, pollen Hyperrespsiveness of airways 2. Exercise—premedicates pt to prevent Cromolyn and tialide 3. Respiroratory infections—Biggest trigger* 4. Drugs and food—ASA, NSAIDS, Beta Blockers, ACE inhibitors (prinivil), yellow dye 5. GERD—gastroesophageal reflux disease 6. Stress— 7. Familial B) Pathophysiology ~ Trigger causes mast cells in bronchioles to release histamine, leukotrienes and prostaglandins ~Increased vasodilation and permeablility—epithelial damage Triad of symptoms—inside bronchioles 1. Bronchospasm 2. Edema in bronchioles 3. Increased mucus production—thick and tenacious 4. expiratory wheezes Limited airflow traps air distally Reduced area for O2 and CO2 exchange Hypoxemia C) manifestations— COPD Maria’s Notes Page 2 chest tightness, dyspneic reddened nose cough wheezing—decreases breath sounds may be bad sign, prolonged expiration, Increased HR, Increased RR—tachypnea Severe attack Use of accessory muscles Intercostals retractions Fatigue Anxiety Failure—decreased to inaudibles Breath sounds. Ineffective cough D) Status asthmaticus—severe prolonged attack that doesn’t respond to tx. ABG’s pH—7.32 Slightly lower PCO2—60 goes up PO—65 II. Diagnositics: H and P—frequency identify trigger Pulmonary function tests—tells us the severity of the disease, response to treatment. Look at forced expiratory volume. Pulse O2 ABG’s—very best indicator or oxygenation Allergy testing Peak expiratory flow rate—at home daily Chest x-ray III. Prevention: COPD Maria’s Notes Page 3 Avoid triggers No pets No smoking Mask/scarf in cold weather IV. Collaborative Care Attacks A) mild to moderate premedicate prior to exercise bronchodilators--proventil/albutero, Maxair, Increases HR, helps to expectorate mucous. B) Moderate attack treatments—regular maintenance Corticosteroids—vanceril and pulmacort—reduce edema and reduce mucus. Cromolyn—hyperresponsiveness of airway Anticholinergic bronchodilators—atrovent/combivent SE: dry mouth C) Severe, frequent attacks ~ Steroids—prednisonePO, Solumedrol IV Decrease in inflammatory process Don’t stop abruptly—can go into adrenal failure Steroids causes an increase in Blood Sugar. ~ Methylxanthines—theophylin—eminophylinne Bronchodilators PO, or IV WATCH HR can go up a lot— Therapeutic levels of Rx—10-20. Give O2—O2 therapy Place pt in Fowler’s position Status asthmaticus—In addition to other tx swteroids q 4-6 IV and continious monitoring/assessment. IV Mg+ can be given as a bronchodilator Teaching Pg 652-658 teach pts at home. Teach first administer bronchodilator THEN steroids COPD Maria’s Notes Page 4 Leukostrine inhibitors—Mast cell—Accolate and zyflo—preventative medicines COPD: Chronic Bronchitis—excessive mucous production Productive cough for 3 or more months for two consecutive years. Mucous (thick and tenacious) results in narrowed airways Results in impaired ciliary fct., can’t sweep things up and out Recurrant infections COR pulmonae—Right sided heart failure Biggest causative factor—SMOKING Called blue bloaters—tendency to get cyanotic and acidotic Emphysema—destruction of alveolar walls— Enlargement of air spaces (Panlobaular (distant) and centrilobular (Closer)) Decreased area for gas exchange Loss of elasticity Loss of tissue that supports the alveoli Causes airways to collapse with expiration Leads to trapped air—some air cannot get out of the lungs Causes: Primary cause: SMOKING Can be hereditary in less than 1%. Caused from Alpha antitrpsin deficiency 1. Signs and Symptoms/manifestations Insidious—1st SOB with exertion Progresses to dyspnea at rest Barreled chest—increased anterior posterior distance in the chest Tachypneic—sleeps sitting up Pink Puffers—initially after more destruction become blue 2. Diagnostics: H and P—PFT’s check serum antialpha tripsin deficiency (blood test for genetics) COPD Maria’s Notes Page 5 Ventilation perfusion scan—looks for clots—V/Q scan Oximetry ABG’s CBC—hgb Hct—chronic bronchitis increased amount of RBC—body is trying to increase amount of hgb and increase amount of O2 carrying capabilities. Chest x-ray Treatment— Stay away from pollution—smoke Flu shot every year . Maybe pneumia vaccine? Increase fluids, (thins out mucous) teach effective cough and deep breathing to clear mucous out. Postural drainage—positioning a pt to drain an area of the lungs Purcussion—clapping and vibrating of chest wall To improve breathing: teach to prolong expiration—pursed lip breathing, strengthen abd. Muscles, helps to force diaphrahm up and better expiration Aggressive tx: O2 therapy CAUTION: drive to breathe is dependant on low O2 levels—don’t administer high levels of O2 (only 2-3 L) Medications: Antibiotics for infections, bronchodilators, (will improve airflow) Steroids—same as for asthma Guiafensin—mucolytic COPD Maria’s Notes Page 6 Test review: 1. Blood gases 2. Medications Cromalin and proventil 3. Ominious sound decreased chest sounds 4. RN Nx chronic bronchitis: ineffective airway clearance 5. Venturei mask—high flow system delivers a fixed concentration of O2. 6. If some one has COPD and they have jugular vien distention and they have edema and no hx of previous heart disease—cor pulmonai—right sided heart failure? 7. Some one has RN Dx impaired gas exchange what is cause? O2 sat of 84 low O2. 8.