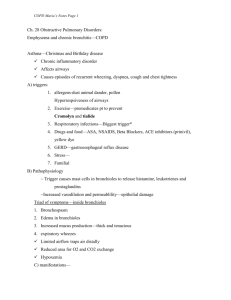
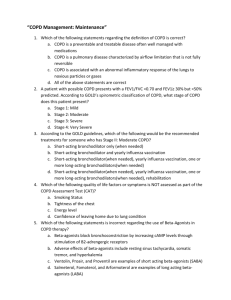
Quiz
advertisement
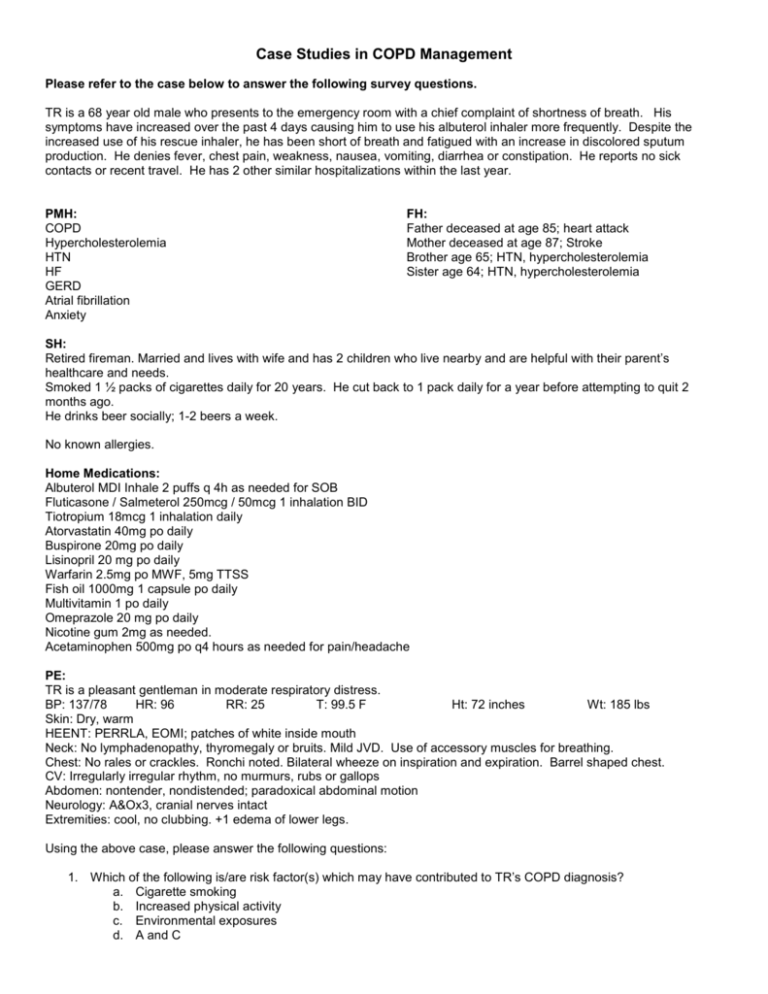
Case Studies in COPD Management Please refer to the case below to answer the following survey questions. TR is a 68 year old male who presents to the emergency room with a chief complaint of shortness of breath. His symptoms have increased over the past 4 days causing him to use his albuterol inhaler more frequently. Despite the increased use of his rescue inhaler, he has been short of breath and fatigued with an increase in discolored sputum production. He denies fever, chest pain, weakness, nausea, vomiting, diarrhea or constipation. He reports no sick contacts or recent travel. He has 2 other similar hospitalizations within the last year. PMH: COPD Hypercholesterolemia HTN HF GERD Atrial fibrillation Anxiety FH: Father deceased at age 85; heart attack Mother deceased at age 87; Stroke Brother age 65; HTN, hypercholesterolemia Sister age 64; HTN, hypercholesterolemia SH: Retired fireman. Married and lives with wife and has 2 children who live nearby and are helpful with their parent’s healthcare and needs. Smoked 1 ½ packs of cigarettes daily for 20 years. He cut back to 1 pack daily for a year before attempting to quit 2 months ago. He drinks beer socially; 1-2 beers a week. No known allergies. Home Medications: Albuterol MDI Inhale 2 puffs q 4h as needed for SOB Fluticasone / Salmeterol 250mcg / 50mcg 1 inhalation BID Tiotropium 18mcg 1 inhalation daily Atorvastatin 40mg po daily Buspirone 20mg po daily Lisinopril 20 mg po daily Warfarin 2.5mg po MWF, 5mg TTSS Fish oil 1000mg 1 capsule po daily Multivitamin 1 po daily Omeprazole 20 mg po daily Nicotine gum 2mg as needed. Acetaminophen 500mg po q4 hours as needed for pain/headache PE: TR is a pleasant gentleman in moderate respiratory distress. BP: 137/78 HR: 96 RR: 25 T: 99.5 F Ht: 72 inches Wt: 185 lbs Skin: Dry, warm HEENT: PERRLA, EOMI; patches of white inside mouth Neck: No lymphadenopathy, thyromegaly or bruits. Mild JVD. Use of accessory muscles for breathing. Chest: No rales or crackles. Ronchi noted. Bilateral wheeze on inspiration and expiration. Barrel shaped chest. CV: Irregularly irregular rhythm, no murmurs, rubs or gallops Abdomen: nontender, nondistended; paradoxical abdominal motion Neurology: A&Ox3, cranial nerves intact Extremities: cool, no clubbing. +1 edema of lower legs. Using the above case, please answer the following questions: 1. Which of the following is/are risk factor(s) which may have contributed to TR’s COPD diagnosis? a. Cigarette smoking b. Increased physical activity c. Environmental exposures d. A and C 2. Fluticasone/Salmeterol Diskus is a: a. Dry powder inhaler b. Metered dose inhaler c. Nebulized solution d. HFA inhaler 3. Patients with an infectious exacerbation of severe COPD are at risk for which pathogens: a. Pseudomonas b. H. influenzae c. S. pneumoniae d. M. catarrhalis e. All of the above 4. The most effective thing TR could do at this point to slow his COPD progression is: a. Better compliance with medications b. Treat his anxiety c. Stop smoking d. Loose weight 5. A Pulmonary rehab program is only indicated in severe COPD a. True b. False 6. Based on TR’s complaints and only having a mild fever: a. Antibiotics are not indicated b. Antibiotics are indicated c. His exacerbation is most likely viral d. A chest X-ray will better clarify the need for antibiotics 7. TR’s current medication treatment for anxiety: a. Should be discontinued because of the side effect of decreasing respiratory drive b. Is a reasonable choice in COPD patients c. Is generally more effective/preferred over the SNRI’s class of medications d. He is not on any anti-anxiety medications 8. TR’s reported level of alcohol intake: a. Is a significant risk factor in further exacerbations b. Will complicate pulmonary rehab efforts c. Is contraindicated in patients receiving warfarin d. Has little to no impact on his COPD 9. Patients at high risk for future exacerbations have: a. A history of 2 or more exacerbations within the previous year b. A GOLD level of 2 or greater for COPD severity of disease c. A GOLD level of 4 for COPD severity of disease d. A and B 10. Patients may respond to the “Righting Reflex” with defensiveness and resistance to change a. True b. False