Presenting Problem and Client Strengths
advertisement

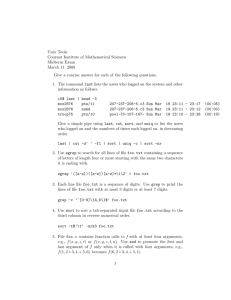
CLINICAL PRACTICUM CLASS, ANTIOCH UNIVERSITY LA CLINICAL ASSESSMENT Page 1 of 6 Revised 01/2012 Client Name: ___________________________________________ Date: _________________________ Presenting Problem and Client Strengths Presenting Problem Why is client coming to treatment? Precipitating Event? Current Complaints, Symptoms/Behaviors: onset, duration, and frequency? What changes in functioning (e.g., at home, school, work, socially) has client experienced? Presenting crises, if any, and how client is managing them? Client Strengths What are client’s strengths? What are client’s current coping mechanisms? Psychiatric/Counseling/Mental Health Treatment History What is client’s previous experience with therapy? Client’s perceived benefits or lack thereof re: previous therapy? Any history of suicidal and/or homicidal ideation/attempts? Does client currently take or have past history of taking psychotropic medication? If yes, name of prescribing physician and the medication(s), dosage and client’s perceived benefits? This confidential information is provided to you in accord with applicable Welfare and Institutions Code Section. Duplication of this information for further disclosure is prohibited without the prior written consent of the patient/ authorized representative to who it pertains unless otherwise permitted by law. Destruction of this information is required after the stated purpose of the original request is fulfilled. Client Name: Agency: ID#: CLINICAL PRACTICUM CLASS, ANTIOCH UNIVERSITY LA CLINICAL ASSESSMENT Page 2 of 6 Revised 01/2012 Family Developmental History and Current Living Situation Family of Origin (FOO) Composition of FOO? Client’s relationship with FOO? Significant events (deaths, divorce, physical/sexual/verbal abuse, serious illnesses, family milestones, etc.) Spoken/unspoken messages client received from FOO and culture/community? FOO attitude towards significant events Client attitude towards FOO Family History Psychiatric/Mental Illness Substance Abuse/Dependence Legal Issues Current Living Situation What is client’s current living arrangement? Client’s feelings about current living situation? Any custody of children or dependents? Does client have financial, legal, or immigration issues? Relationship Status/History and Current Support System Relationship Status/History If coupled, how long and what is quality of the relationship? If single, is client dating or interested in a relationship? What is client’s relationship history and what are client’s interpersonal relationship patterns (e.g., abuse, codependence, etc.)? Current Support System Composition Who is available to client for emotional support? Is support system aware of client’s presenting problems? What are the deficits in client’s support system? This confidential information is provided to you in accord with applicable Welfare and Institutions Code Section. Duplication of this information for further disclosure is prohibited without the prior written consent of the patient/ authorized representative to who it pertains unless otherwise permitted by law. Destruction of this information is required after the stated purpose of the original request is fulfilled. Name: Agency: ID#: CLINICAL PRACTICUM CLASS, ANTIOCH UNIVERSITY LA CLINICAL ASSESSMENT Page 3 of 6 Revised 01/2012 Client Educational, Vocational, & Social History Educational and Vocational History Client’s education history, highest grade completed, and attitude toward school? Does client have educational aspirations and/or goals? If so, what? Does client currently have employment? Employment satisfaction? If client is unemployed, is client satisfied with unemployment? Goals for employment? Significant events in clients’ educational/vocational history? Social History Client’s significant cultural, ethnic, racial, class, religious, and/or spiritual influences? How have those influences viewed client’s sexual and/or gender identity? What are the client’s hobbies/social activities? Drug/Alcohol/Addictive Behavior History Past history of drug/alcohol use/abuse (including onset, frequency, quantity)? Treatment? Current use/abuse of drugs/alcohol (including onset, frequency, quantity)? Impact on client’s life and relationships of drug/alcohol use/abuse? Client’s attitude toward drug/alcohol use/abuse? Is client attempting to stop/reduce use or seek treatment? Does client have other addictive behaviors (e.g., food, gambling, sex, video games, etc.) This confidential information is provided to you in accord with applicable Welfare and Institutions Code Section. Duplication of this information for further disclosure is prohibited without the prior written consent of the patient/ authorized representative to who it pertains unless otherwise permitted by law. Destruction of this information is required after the stated purpose of the original request is fulfilled. Name: Agency: CLINICAL ASSESSMENT ID#: CLINICAL PRACTICUM CLASS, ANTIOCH UNIVERSITY LA CLINICAL ASSESSMENT Page 4 of 6 Revised 01/2012 General Medical History History of significant illnesses/injuries/allergies? History of hospitalizations and/or surgeries? Does client have any permanent disabilities? Does client have a primary care physician? If so, name and phone? Intimate Partner/FOO Domestic Violence Assessment Frequency of conflicts & the manner in which they are/were resolved w/partner/FOO? Interrogation about or restriction of outside activities, associations, and/or friends by client, partner, or within FOO? If yes, describe Name-calling, insults, threats by client, partner, or within FOO when angry? If yes, describe Does client, partner, or those in FOO have an explosive temper or difficulty controlling anger? If yes, describe Hitting, shoving, kicking, or throwing of objects by client, partner, or FOO when angry? If yes, describe: Has client, partner, or FOO ever required medical treatment as a result of abuse? If yes, describe Have law enforcement personnel ever been involved because of fighting or abuse? If yes, describe Does client, partner, or FOO own a weapon? If yes, describe weapon, location, whether it is locked, and the frequency & purpose of use What does client hope to accomplish from counseling/therapy at Agency (e.g., increase self esteem, support during coming out process, working to build LGBTQ support system, etc.)? Client’s Expectations Of Therapy What is client’s understanding of and commitment to the therapeutic process? Is client in need of any referrals at this time? Any suggestions for reading for client at this time? This confidential information is provided to you in accord with applicable Welfare and Institutions Code Section. Duplication of this information for further disclosure is prohibited without the prior written consent of the patient/ authorized representative to who it pertains unless otherwise permitted by law. Destruction of this information is required after the stated purpose of the original request is fulfilled. Referrals/Bibliotherapy Name: Agency: CLINICAL ASSESSMENT ID#: CLINICAL PRACTICUM CLASS, ANTIOCH UNIVERSITY LA CLINICAL ASSESSMENT Page 5 of 6 Revised 01/2012 Mental Status Provide a word picture of the client based on your observations. Be sure to address relevant features from each bolded category in the left column by editing/changing the words under each heading. Appearance Dress, grooming, unusual physical characteristics. Behavior Activity level, mannerisms, eye contact, manner of relating to parent/therapist, motor behavior, aggression, impulsivity. Appearance: Client is a -year-old African American/Caucasian/Hispanic male/female who presented as his/her stated age. He/She appeared clean/unkempt and was dressed casually/formally in a clean/rumpled/dirty pullover/longsleeve/short-sleeve shirt/blouse, clean/rumpled/dirty pants/jeans/dress, and shoes/sneakers. His/Her grooming appeared poor/fair/age-appropriate. He/She appeared to have no unusual physical characteristics. Behavior: Client presented with low/moderate/high activity level, expressive hand and arm gestures to accentuate his/her verbal content, and with poor/fair/good eye contact. He/She seemed to relate to this therapist/writer with some degree of suspicion/guardedness/openness. Client appeared to have age-appropriate fine and gross motor movement. He/She exhibited no overt aggression or impulsivity throughout the interview. Expressive Speech Fluency, pressure, impediment, volume Expressive Speech: Client's speech exhibited fluency, articulation, and appropriate volume, with no sign of pressuring or impediment. Thought Content Fears, worries, preoccupations, obsessions, delusions, hallucinations Thought Content: Client's thought content exhibited no overt or excessive fears, worries, preoccupations, or obsessions. Client denied any current or past delusions or hallucinations. Thought Process Attention, concentration, distractibility, magical thinking, coherency of associations, flight of ideas, rumination, defenses (e.g. planning) Cognition Orientation, vocabulary, abstraction, intelligence Mood/Affect Depression, agitation, anxiety, hostility absent or unvarying, irritability Thought Process: Client's thought process exhibited coherency of associations and no difficulty with attention, concentration, distractibility, magical thinking, flight of ideas, or rumination. Client's main defense appears to be denial/planning/withholding/withdrawing/intellectualization/repression. Cognition: Client was oriented x4 (person, place, time, and situation). He/She appears to have an average/aboveaverage/below-average vocabulary and an average/above-average/below-average level of intelligence, with a poor/fair/good degree of abstraction. Mood/Affect: Client presented with a relaxed/restricted/blunted/sad/angry affect and acknowledged/denied feelings of depression and/or anxiety, with no/occasional/frequent feelings of agitation and/or irritability. He/She exhibited no hostility throughout the interview. Suicidality/Homicidality Thoughts, behavior, stated intent, risks to self or others Suicidality/Homicidality: Client denied any current or past history of suicidal ideation or attempts or of homicidal ideation or attempts. Attitude/Insight/Strengths Adaptive capacity, strengths & assets, cooperation, insight, judgment, motivation for treatment. Attitude/Insight/Strengths: Client presented with a low/moderate/high level of adaptive capacity. Client reported his/her strengths as follows: (from p.1). Client was cooperative throughout the interview and exhibited poor/fair/good judgment, little/moderate/good insight, and a low/moderate/high level of motivation for treatment. This confidential information is provided to you in accord with applicable Welfare and Institutions Code Section. Duplication of this information for further disclosure is prohibited without the prior written consent of the patient/ authorized representative to who it pertains unless otherwise permitted by law. Destruction of this information is required after the stated purpose of the original request is fulfilled. Name: Agency: CLINICAL ASSESSMENT ID#: CLINICAL PRACTICUM CLASS, ANTIOCH UNIVERSITY LA CLINICAL ASSESSMENT Page 6 of 6 Revised 01/2012 Diagnosis I. Summary & Formulation: (Be sure to write from your theoretical orientation [e.g. Psychodynamic, Family Systems, CBT, Cultural Diversity, and Feminist] and include an Affirmative Conceptualization of Client, Strengths, Coping Mechanisms, Levels of Internalized Homophobia/Heterosexism, Potential for Therapeutic Work, Observations/Descriptions, Current Symptoms/Behaviors, and Impairments in Life Functioning, i.e. Work, School, Home, Community, Living Arrangements, etc.) II. Admission Diagnostic Impression: Axis I: Axis II: Axis III: Axis IV: Axis V: Principle Secondary Code: Code: Code: Code: Code: Code: Code: Nomenclature: Nomenclature: Nomenclature: Nomenclature: Nomenclature: Nomenclature: Nomenclature: Psychosocial and environmental problems that may affect diagnosis, treatment, or prognosis: 1. Primary Support Group; 2. Social Environment; 3. Educational; 4. Occupational; 5. Housing; 6. Economic; 7. Access to Health Care; 8. Interaction with Legal System; 9. Other Psychosocial/Environmental; 10. Inadequate Information. Current GAF Score: Signatures Assessor’s Signature & Discipline* Date Co-Signature & Discipline * Licensed MHP or unlicensed MHP with co-signature This confidential information is provided to you in accord with applicable Welfare and Institutions Code Section. Duplication of this information for further disclosure is prohibited without the prior written consent of the patient/ authorized representative to who it pertains unless otherwise permitted by law. Destruction of this information is required after the stated purpose of the original request is fulfilled. Name: Agency: CLINICAL ASSESSMENT ID#: Date