neuroOct24-31
advertisement

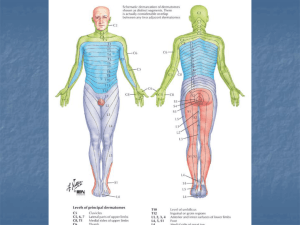
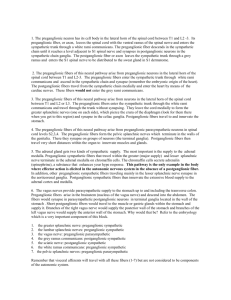
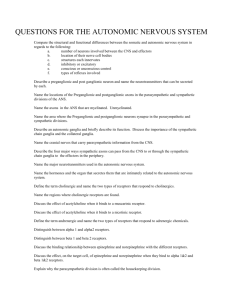
T3 - Neurology Oct. 24, 2003 Dr. Laura McNeilly Post ganglionic Neurons Cell bodies from the sympathetic ganglia Sympathetic ganglia found in 2 locations 1. Sympathetic Chain, aka trunk C1 -= coccyx 3 pairs of cervical ganglia 12 “ “ thoracic “ 5 “ “ lumbar “ 5 “ “ sacral “ 1 coccygeal ganglion 51 Total ganglia axons are unmyelinated axons have 2 options: a) exit sympathetic ganglia forming the gray ramus, and reconnects with a spinal nerve proximal to branching of anterior and posterior rami. These neurons will travel with a spinal nerve and supply sympathetic innervation to structures in skin and body wall. Both anteriorly and posteriorly. ** all spinal nerves receive gray rami. b) exit the sympathetic ganglion and travel with blood vessels to innervate other structures (organs, glands) ABOVE DIAPHRAGM. 2. Prevertebral Ganglia A group of 3 ganglia located along the abdominal aorta named for the major unpaired branches of aorta (Celiac, superior and inferior mesenteric) Cervical Sympathetic Chain 3 pairs of cervical sympathetic ganglia 1. Superior ganglion 2. Intermediate ganglion 3. Inferior ganglion 4. [ sometimes a 4th called Cervicothoracic ganglion aka: Stellate ganglion] Superior cervical ganglion Located anterior to C1, posterior to jaw Gives off gray rami to cervical nerves C1 – 4 Gives off fibers which follow Common Carotid Arteries and their branches to supply anterior brain and face. Intermediate Cervical ganglion Gives off gray rami to CN C5 and C6 Gives off fibres which follow Vertebrobasilar system to supply posterior brain Inferior Cervical ganglion Gives off gray rami to CN C7 and C8 Gives off fibers which follow Vertebrobasilar system to supply posterior brain Both intermediate and inferior ganglia give off small #’s of fibers which go to thoracic structures. Thoracic Sympathetic Chain Consists of 12 pairs of ganglia Each ganglion receives preganglionic fibers from associated nerve root via White Ramus. Each receives fibers which pass up or down the chain one or more levels. Each ganglion gives off a gray ramus which connects to its associated spinal nerve. Additionally: T1 – T4: gives off fibres which supply organs and glands of thorax (heart, lungs). These fibers follow the aorta and its branches. T5 – T9: have Preganglionic fibers which pass through w/o synapsing and collectively form the GREATER SPLANCHNIC NERVE, Which ends in a Prevertebral ganglion. (preganglionic nerve starting from ant/lat horn of SC) T10 – T11: have preganglionic fibers which pass through without synapsing forming the LESSOR SPLANCHNIC NERVE, which ends in a prevertebral ganglion. T12: has preganglionic fibers which pass through without synapsing forming the LEAST SPLANCHNIC NERVE. Which ends in a prevertebral ganglia. Splanchnic nerve and their post ganglionic fibers supply the abdominal organs. ** end of 10/24 notes, begin 10/31 notes ** Lumbar Sympathetic Ganglia 5 ganglia each ganglia gives off a gray ramus to its associated spinal nerve Additionally L1 – L2: receive preganglionic fibers from associated spinal nerve via White Rami Have preganglionic fibers which pass through without synapsing and collectively form the LUMBAR SPLANCHNIC NERVE which will end in a prevertebral ganglion. L3 – L5: receive preganglionic fibers from T11 – L2 which pass down the chain. Sacral Sympathetic Ganglia 5 ganglia receive preganglionic fivers from T11 – L2 each ganglion will give off a Gray ramus to its associated spinal nerve Coccygeal Ganglion aka: Ganglion impar both (R + L) sympathetic chains unite at this point anterior to coccyx receives preganglionics from T11 – L2, and gives off a gray ramus to its associated spinal nerve. Clinical Note: due to the location of the ganglion, injury to the coccyx can lead to: o pushing of filum terminale leading to laxing of spinal cord and potential for nerve root damage. o Irritation of the ganglion leading to aberrant sympathetic output. Some correlation between coccygeal injuries and PMS, endometriosis, constipation, etc. PREVERTEBRAL GANGLIA aka Collateral Ganglia, aka Paravertebral Ganglia 3 ganglia located on anterior surface of abdominal aorta, in association with the 3 major unpaired trunks of aorta. mesentery – conn. tiss. That hold the organs to the body wall. 1. Celiac Ganglion Receives preganglionic fibers from T5 – T10 via Greater and Lesser Splanchnic nerve. Post ganglionic fibers follow the celiac artery and its branches to supply the liver, gallbladder, stomach, pancreas, spleen, kidneys, adrenal glands. Plexus that follows the artery is called CELIAC PLEXUS, aka SOLAR PLEXUS. Some preganglionic fibers which passed through the sympathetic chain also passed through the Celiac ganglion w/o synapsing, these fibers travel to the adrenal medulla and synapse there. 2. Superior Mesenteric Ganglion receives preganglionic fibers fromT10- T11 via the LESSOR SPANCHNIC NERVE post ganglionic fibers follow the superior mesenteric artery to supply the small intestine, proximal large intestine up to splenic flecture. 3. Inferior Mesenteric Ganglion Receives its preganglionic fibers from T12 – L2 via the Least and Lumbar Splanchnic nerves Post ganglionic fibers follow the inferior Mesenteric artery to supply distal colon, bladder, genitalia. ARDRENAL MEDULLA Cells are embryologically nervous tissue. These cells are the “POST GANGLIONIC NEURONS” BUT they release their NT’s into the bloodstream vs. a synaptic cleft, cells are considered glandular and NT is called a HORMONE. A NT that is secreted into the tissues via a synapse remains active for only a few seconds before it is: a). broken down b) recycled c) diffused away Hormones are released directly into the blood stream, these remain active much longer (10s – several minutes) and are broken down in the liver (usu.) Hormones released from AM = NOREPINEPHRINE AND EPINEPHRINE Clinical Note: 1. stimulation of AM causes release of hormones which have sympathetic effect in the body (like sympathetic nervous innervation) but effect is greatly prolonged. (lasts longer) organs/glands redeive dual sympathetic stimulation reflecting importance of sympathetics for survival. 2. having the AM involved in sympathetic allows for sympathetic access to every cell in the body. Substances which stimulate adrenals: a) caffeine (and related xanthines) b) perceived stress NEUROTRANSMITTERS IN ANS this applies to para/sympathetic NS in the ANS A) all parts of the peripheral NS (somatic and autonomic) include: Preganglionic sympathetics, Pre/Post ganglionics Parasympathetics Somatics They all release: ACETYLCHOLINE there are 2 kinds of cholinergic receptors (receives Ach) 1. muscarinic: btwn post ganglionics and effector cells 2. nicotinic: btwn pre/post ganglionic and at neuromuscular junctions (NMJ) B) Postganglionic sympathetic neurons release: NOREPINEPHRINE EXCEPT: 1. sympathetics to sweat glands release Ach 2. norepinephrine is converted to EPI in the Adrenal medulla adrenergic receptors are further divided into ALPHA AND BETA Clinical Note: “beta blockers” – drugs that block beta receptors of the heart which blocks sympathetic innervation of the heart. ** end of 10/31 notes **