AUTONOMIC
NERVOUS
SYSTEM
PRESENTED BY:
LAHARI PALADUGU
PHARM D (09-10)
DEFINITION
The autonomic nervous system (ANS or visceral nervous
system or involuntary nervous system) is the part of the
peripheral nervous system that acts as a control system,
functioning largely below the level of consciousness, and
controls visceral functions.
The ANS affects heart rate, digestion, respiratory rate,
salivation, perspiration, pupillary dilation, micturition, and
sexual arousal.
Most autonomous functions are involuntary but a number of
ANS actions can work alongside some degree of conscious
control.
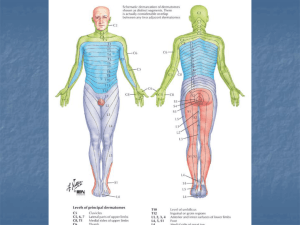
LOCATION
Within in the brain, the autonomic
nervous system is located in the
medulla oblongata in the
lower brainstem.
The hypothalamus, just
above the brain stem, acts as an
integrator for autonomic functions,
receiving ANS regulatory input
from the limbic system to do
so.
DIVISIONS
ANS
Functional
Sympathetic
Anatomical
Parasympathetic
Enteric
Chemical
Adrenergic
Non-cholinergic,
non-adrenergic
Cholinergic
Thoracolumbar
Craniosacral
SYMPATHETIC NERVOUS SYSTEM
It has:
-
A central controlling part
-
A peripheral portion which takes origin in the lateral
horn of the spinal cord from T1 to L2. The main cerebral
controlling center is the posterior hypothalamus.
-
The peripheral portions has:
-
Afferent fibers
Efferent fibers
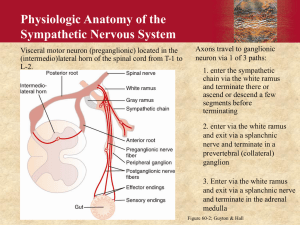
(THORACOLUMBAR) OUTFLOW
OF SYMPATHETIC FIBERS
Consists of cell bodies in the
lateral horn of the spinal
cord (intermediolateral cell columns) from T1 to L2/3.
Because its cells begin in the thoracic and
lumbar regions of the spinal cord, the SNS is
said to have a thoracolumbar outflow.
ORGANIZATION.
Take origin from the lateral horn cells of T1 to L2 and
come out of the spinal cord via the anterior root.
Axons of these nerves leave the spinal cord through
the anterior rootlet/root. They pass near the spinal
(sensory) ganglion, where they enter the anterior rami
of the spinal nerves. However, unlike somatic
innervation, they quickly separate out through white
rami connectors that connect to either the
paravertebral (which lie near the vertebral column) or
prevertebral (which lie near the aortic bifurcation)
ganglia extending alongside the spinal column.
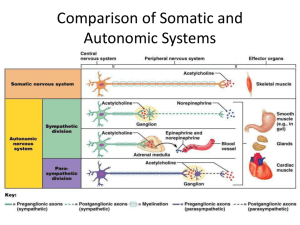
SYNAPTIC TRANSMISSION.
To reach target organs and glands, the axons must travel long
distances in the body, and, to accomplish this, many axons relay
their message to a second cell through synaptic
transmission. The ends of the axons link across a space, the
synapse, to the dendrites of the second cell. The first cell (the
presynaptic cell) sends a neurotransmitter across the synaptic
cleft where it activates the second cell (the postsynaptic cell). The
message is then carried to the final destination.
SOME TERMS…
In the SNS and other components of the peripheral nervous
system, these synapses are made at sites called ganglia.
The cell that sends its fiber is called a preganglionic cell,
while the cell whose fiber leaves the ganglion is called a
postganglionic cell. As mentioned previously, the
preganglionic cells of the SNS are located between the first
thoracic segment and third lumbar segments of the spinal
cord.
Postganglionic cells have their cell
bodies in the ganglia and send their axons
to target organs or glands.
Presynaptic nerves' axons terminate in either the
paravertebral ganglia or prevertebral ganglia. There are four
different ways an axon can take before reaching its terminal:
1
• Axon enters the paravertebral ganglion at
level of its originating spinal nerve
2
• Synapse in the ganglion, ascend to a more
superior paravertebral ganglion
3
• Descend to a more inferior paravertebral
ganglion and synapse there
4
• Or it can descent to a prevertebral ganglion
and synapse there with a postsynaptic cell
The postsynaptic cell then goes on to innervate the targeted
end effector (i.e. gland, smooth muscle, etc.). Because
paravertebral and prevertebral ganglia are relatively close to
the spinal cord, presynaptic neurons are generally much
shorter than their postsynaptic counterparts, which must
extend throughout the body to reach their destinations.
The ganglia include not just the sympathetic trunks but also
the cervical ganglia (superior, middle, and inferior), which
sends sympathetic nerve fibers to the head and thorax
organs, and the celiac and mesenteric ganglia (which send
sympathetic fibers to the gut).
AN EXCEPTION… THE
ADRENAL MEDULLA
Specialized ganglion of the SNS.
Presynaptic neurons pass through paravertebral ganglia, on
through prevertebral ganglia and then synapse directly with
suprarenal tissue. This tissue consists of cells that have pseudoneuron like qualities in that when activated by the presynaptic
neuron, they will release their neurotransmitter (epinephrine)
directly into the blood stream.
Preganglionic fibers synapse directly on chromaffin cells in the
adrenal medulla.
These chromaffin cells secrete epinephrine and norepinephrine
into the circulation.
MECHANISM OF ACTION.
The SNS is designed for a quick immediate and massive action
and in conjunction with adrenal medulla initiate reactions in
conditions of stress… Fight or flight reaction.
MECHANISM…
Its effect is mediated by catecholamines through three
types of receptors:
• epinephrine and norepinephrine are mediated by αreceptors and β-receptors
•
•
•
•
α1-receptors
α2-receptors
β1-receptors
β2-receptors
• dopamine action is mediated through D receptors
PARASYMPATHETIC NERVOUS
SYSTEM (CRANIOSACRAL SYSTEM)
The parasympathetic system is responsible for stimulation of
"rest-and-digest" or “feed and breed” activities
that occur when the body is at rest, especially after eating,
including sexual arousal, salivation, lacrimation, urination,
digestion, and defecation
Its action is described as being complementary
the sympathetic nervous system.
to
LOCATION.
Parasympathetic nerve fibers arise from the
central nervous system with the S2, S3, and S4
spinal nerves and from third, seventh, ninth, and
tenth cranial nerves. Because of its location, the
parasympathetic system is commonly referred to
as having "craniosacral outflow", which stands in
contrast to the sympathetic nervous system, which
is said to have "thoracolumbar outflow".
The parasympathetic nerves that arise from the S2,
S3, and S4 spinal nerves are commonly referred to
as the pelvic splanchnic nerves or the "nervi
erigentes".
PATHWAYS.
The main controlling center is present in the anterior
hypothalamus. The parasympathetic nervous system
also has:
1) Afferent fibers
2) Efferent fibers
The afferent fibers are concerned with the detection of
volume and pressure changes in the viscera.
The efferent fibers are concerned with secretomotor
activity of the viscera.
OUTFLOW.
The outflow has two divisions:
1) Cranial division
2) Sacral division
CRANIAL DIVISION.
EdingerWestphal
nucleus
Superior
salivary
nucleus
Preganglionic
neurons
Dorsal
nucleus and
nucleus
ambiguous of
the vagus
Inferior
salivary
nucleus
The preganglionic nerve fibers of these neurons
synapse in the appropriate ganglia. These ganglia are
present near the target organ.
Postganglionic nerve fibers starts from these ganglia
and supply to the organ.
Preganglionic fibers are longer and the
postganglionic fibers are shorter.
CRANIAL DIVISION.
The cranial outflow is through III, VII, IX, and X.
Occulomotor – III
Constrictor pupillae
Ciliaris
Facial – VII
Lacrimal gland
Submaxillary gland and sublingual gland
Glossopharyngeal – IX
Parotid gland
Vagus – X
CVS, RS, GIT, up to transverse colon.
SACRAL DIVISION
The preganglionic neurons are present in the lateral horns of
sacral segments (S2, S3, and S4).
Preganglionic fibers come out through the anterior root and
form nervi erigentis or pelvic nerve.
The postganglionic neurons are present in the target organ
itself.
Nervi erigentis supplies the descending colon, sigmoid
colon, and rectum. It also supplies the urinary bladder,
erectile tissue of the penis and the uterus.
RECEPTORS
The parasympathetic nervous system uses chiefly acetylcholine
(ACh) as its neurotransmitter, although peptides (such as
cholecystokinin) may act on the PSNS as a neurotransmitter.
The ACh acts on two types of receptors, the muscarnic and nicotinic
cholinergic receptors.
Most transmissions occur in two stages: When stimulated, the
preganglionic nerve releases ACh at the ganglion, which acts on
nicotinic receptors of postganglionic neurons. The postganglionic
nerve then releases ACh to stimulate the muscarinic receptors of
the target organ.
NICOTINIC RECEPTORS.
MUSCARNIC RECEPTORS.
INTERACTION OF THE TWO
DIVISIONS… SNS & PSNS.
Most of the organs receive dual nerve supply. Though the
actions of these two systems appear to be opposed, they are
in-fact complementary. Depending on the situation at one
moment, the sympathetic dominates and the PSNS is
inhibited and in the next moment, the PSNS dominates and
the SNS is inhibited.
ENTERIC NERVOUS SYSTEM.
Consists of intramural nerve plexesus:
(a) myenteric plexus
(b) Meissner’s plexus
These are present in the GIT and contain the sensory, motor, and
interneurons.
Their activity is modulated by the sympathetic and
parasympathetic nerve fibers. Several neurotransmitters are
associated with this system. They influence
- Smooth muscle: peristalsis and villi movements
- Gland secretion: of enzymes, electrolytes, and the
mucous
- Blood vessels: alter blood flow
- APUD cells: release of various GIT hormones
CENTRAL CONTROL OF THE
AUTONOMIC NERVOUS SYSTEM.
DISORDERS OF THE ANS.
-
Autoimmune autonomic gangliopathy
-
Congenital central hypoventilation syndrome
-
Familial dysautonomia
-
Holmes-Adie syndrome
-
Horner syndrome
-
Multiple system atrophy
-
Neurally mediated syncope
-
Orthostatic hypotension
-
Postural tachycardia syndrome
-
Striatonigral degeneration
-
Vasovagal syncope
-
Erectile dysfunction
-
Etc……
DRUGS AFFECTING
AUTONOMIC ACTIVITY.
REFERENCES.
1) https://en.wikipedia.org/wiki/Sympathetic_nervous_syste
m
2) https://en.wikipedia.org/wiki/Parasympathetic_nervous_s
ystem
3) http://www.nlm.nih.gov/medlineplus/autonomicnervoussy
stemdisorders.html
4) http://www.dana.org/news/brainhealth/detail.aspx?id=978
0
5) Fundamentals of Medical Physiology 4th Edition – LPR
6) BRS Physiology 5th edition - Costanzo