Lecture 8
advertisement

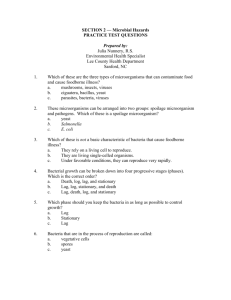
Lecture 7 Dr. Ismail I. Daood Medical Microbiology Clostridium tetani : Clostridium tetani which causes tetanus, is worldwide in distribution in the soil and in the feces of animals and human. It has specific flageller antigens, all type produce same neurotoxin, tetanospasmin. Small amounts of toxin can be lethal for humans. The vegetative cells of C tetani produce the toxin tetanospasmin which binds to motor neurons that effect to the spinal cord and brain . Pathogenesis : C tetani not invasive organism . The infection remains localized in the area of tissue ( wound, burn, injury, surgical suture )in which the spores have been introduced , and the disease is entirely a toxemia. Germination of the spore and development of vegetative that produce toxin are aided by necrotic tissue, calcium salts, and pyogenic infections ,then the toxin released reaches the central nervous system (CNS) and rabidly become fixed to receptors in the spinal cord and brain. Treatment : Intramuscular administration of 250-500 units of human antitoxin ( tetanus immune globulin ) to neutralizes the toxin that has not been fixed to nervous tissues . Patients who develop symptoms of tetanus should receive muscle relaxants , sedation, and assisted ventilation. Sometimes surgical to removes the necrotic tissue . Penicillin inhibits the growth of C tetani and stops toxin production . 54 Prevention of tetanus depend on : 1. active immunization with Toxoids. 2. care of wounds contaminated with soil, etc. 3. prophylactic use of antitoxin 4. administration of penicillin. Enterobacteriaceae \ Enteric Gram-Negative Rods : Enterobacteriaceae are a large, heterogeneous group of gram- negative rods ( bacilli ) whose natural habitat is the intestinal tract of human and animals . The family includes many genus ( Escherichia, Shigella , Salmonella, Enterobacter , Klebsiella, Proteus and others ). referred to as "enteropathogenic bacteria" or enteric bacilli or simply enteric these involved in extra intestinal infections. Some enteric organisms e.g. Escherichia coli , are part of the normal flora and incidentally cause disease . Most of them are opportunistic pathogens infected human, general characteristics of it : Gram-negative rods, nonspore-forming facultative anaerobic, grow in simple media ferment glucose and produce acid, motile, have peritrichous flagella capsulated. Major enteropathogenic bacteria : Enterobacteriaceae (these bacteria may also be called coliforms). a. Opportunistic bacteria Escherichia coli (most strains), Citrobacter spp., Shigella spp. , Salmonella spp., Enterobacter spp. , Klebsiella spp. , Proteus spp. . b. Pathogenic bacteria - E. coli (some strains) Shigella - Shigella dysenteriae. S., flexneri, S. boydii S. sonnei Salmonella - Salmonella typhi , - Salmonella paratyphi A&B 55 Escherichia coli : General properties of E. coli the normal intestinal flora member gram –ve ,motile ,non-spore forming , a typically produces positive tests for indole, lysine decarboxlase and manitol fermentation , hemolysis on blood a agar ,produces gas from glucose . and certain related bacteria (e.g. Klebsiella, Enterobacter, Citrobacter) form the group known as the Coliforms. - Characteristics of E. coli : Ferments lactose on MacConkey agar Produce gas when fermenting glucose Produce indol when breaking down tryptophan Gram-negative, Motile , Virulence factors : Exotoxin and Endotoxin - Pathogenesis of E. coli : E. coli cause gastroenteritis, urinary tract infection, neonatal meningitis, secondary pneumonia nosocomial infections The most serotype pathogenic . E coli-Associated Diarrheal Diseases : Enteropathogenic E coli (EPEC) Enterotoxigenic E coli (ETEC) Enterohemorrhagic E coli (EHEC) Enteroinvasive E coli (EIEC) verotoxin very similar to shigellosis Enteroaggregative E coli (EAEC) causes acute and chronic diarrhea -Lab diagnosis Clinical picture, age of patient, travel history are important in diagnosis. Sample from feces, infected tissue, blood, urine collected are 56 using for visitation of UTI and cultured on media and differential media. Biochemical analysis and stereotyping. - Treatment Rehydration with electrolyte-rich antibiotics used in patients with chronic infections of their location Trimethoprim-sulfamethoxazol. Shigella : Shigellae are nonmotile and usually do not ferment lactose but do ferment other carbohydrates, producing acid but not gas. They do not produce H2S. The four Shigella species are closely related to E coli. General properties of Shigella : Gram-negative, non-motile non-fermented lactose on MacConky agar, not produce gas from fermented carbohydrate, not produceH2S from thiosulfate. a. Group A. S. dysenteriae. b. Group B. S. flexneri. c. Group C. S. boydii. d. Group D. S. sonnei. - Pathogenesis : Shigella is the agent of bacterial dysentery shigellosis, it causes watery diarrhea, severe abdominal cramps, stools containing blood and mucus. - Lab. Diagnosis : Shigella must be isolated from sample : Feces, rectal swab, mucosal ulcer cultured on media and selective media as SS agar MacConky agar. - Treatment : supportive therapy by fluid replacement. Antibiotics Ampicillin, Amoxicillin, Trimethoprim-sulfamethoxazol, Cefalosporines. 57 new generation of Salmonella : Salmonellae are often pathogenic for humans or animals when acquired by the oral route. They are transmitted from animals and animal products to humans, where they cause enteritis, systemic infection, and enteric fever. General properties of Salmonella are : Gram-negative, motile, non-spore forming non-fermented lactose on MacConkey agar produce gas when fermenting glucose, produce H 2S from thiosulfate. (TSI) Major species include : - Salmonella typhi - Salmonella paratyphi A and Salmonella paratyphi B - Salmonella enteritidis Pathogenesis : - Endotoxin contain LPS with D antigen. - Invasine adherence to and penetration of intestinal epithelial cell - Capsule resistance to phagocytosis. - Iesistance to acidic pH of stomach. - Vi Virulence antigen (special capsule polysaccharides . causes Enterocolitis (Salmonellosis). Lab. Diagnosis: Culture and isolation are essential to confirm infection based on biochemical test. Treatment : Chloramphenicol, Amoxicillin or Ampicillin with Trimethoprim-sulfamethoxazol, Quinolones (Ciprofloxacin). Ceftrixon. Vibrionaceae Vibrio cholerae : General properties of Vibrio cholerae is a comma shaped, rod 2–4mm long, gram-negative, motile Oxidase-positive with single polar flagellum non-spore curved. It is actively motile by means of 58 a polar flagellum. On prolonged cultivation, vibrios may become straight rods that resemble the gram-negative enteric bacteria - Major species : 1. Classic cholera O1 group – two biotype. El Tor and classic. about 75% of infections with the El Tor biotype. The incubation period is 1–4 days for persons who develop symptoms, depending largely upon the size of the inoculum ingested. There is a sudden onset of nausea and vomiting and profuse diarrhea with abdominal cramps. Stools, which resemble "rice water," contain mucus, epithelial cells, and large numbers of vibrios 2. Non-O2 group. – pathogenesis : Enterotoxin (choleragen) Aregion & B region - Adhesion factors, adherence and colonization secretion of cholera toxin. Increased adenylcyclase activity and accumulation of(cAMP). Lab Diagnosis. Fecal samples cultured on selective media, alkaline peptone broth, V cholerae grows well on thiosulfate-citrate-bile-sucrose (TCBS) agar, on which it produces yellow colonies that are readily visible against the dark-green background of the agar. Vibrios are oxidase-positive. Treatment : - Fluid replacement as intravenous glucose solution or oral 2% glucose sol. - Antibiotics therapy drugs of choice are tetracycline chloramphenicol, and cephalosporins. Chlamydia Chlamydiae that infect humans are divided into three species: Chlamydia trachomatis, 59 Chlamydia pneumoniae, Chlamydia psittaci The Chlamydiae can be viewed as gram-negative bacteria that lack mechanisms for the production of metabolic energy and cannot synthesize ATP. Thus, Chlamydiae are obligate intracellular parasites. Pathogenesis : The incubation period for chlamydial conjunctival infection is 3–10 days. In endemic areas, initial trachoma infection occurs in early childhood,. Chlamydial infection is often mixed with bacterial conjunctivitis in endemic areas, and the two together produce the clinical picture. The mucopurulent earliest symptoms discharge, of conjunctival trachoma are hyperemia,. lacrimation, Microscopic examination of the cornea reveals epithelial keratitis. It includes agents of human disorders such as trachoma, inclusion conjunctivitis, nongonococcal urethritis, cervicitis, pneumonitis of infants. Treatment : Sulfonamide, Erythromycin, and Tetracycline have been used to suppress Chlamydia and bacteria that cause eye infections. Mycobacteria : The mycobacteria are rod-shaped, aerobic bacteria that do not form spores. Although they do not stain readily, once stained they resist decolorization by acid or alcohol and are therefore called "acid-fast" bacilli. The most human pathogens are: - Mycobacterium tuberculosis causes tuberculosis (TB) - Mycobacterium leprae causes leprosy. - Mycobacterium avium -intracellulare (M avium complex, or MAC). - Other atypical mycobacteria frequently infect patients with AIDS, are opportunistic pathogens in other immunocompromised persons, and occasionally cause disease in patients with normal immune systems. 60 General properties : - slow-growing - Bacteria shape slender, straight or curved rods - Survive after ingestion by macrophages. Mycobacterium tuberculosis (TB) Motuberculosis are slender rod, (comma), acid-fast staining, slow growing, microaerophilic, or aerobe, grow best at 37 oC temp. contains glycolipid as mycolic acid in the outer surface of cell wall. Antibacterial resistance. Pathogenesis : Infection the lower lung primary infection, cause active tuberculosis, phagocytosed bacilli will diffuse through the lymphatic vessels and the blood stream reactivation of a latent infection may occur 20 years or lougher after primary infection. Clinical signs include coughing, hempotypsis, after noon fever, weight loss, and malaise. Lab. Diagnosis : Sample from sputum culture on special media required long incubation 1 to six weeks colonies appear, Tuberculin Test , volume is usually 0.1 mL injected intracutaneously, A positive tuberculin test does not prove the presence of active disease due to tubercle bacilli. Isolation of tubercle bacilli provides such proof .Also chest X-ray used. Treatment : Bacteria resistance to antibiotics, treatment should be continued for several months depending on the severity of the disease, the drugs The two major drugs used to treat tuberculosis are isoniazid and rifampin. The other first-line drugs are pyrazinamide, ethambutol, and streptomycin. 61