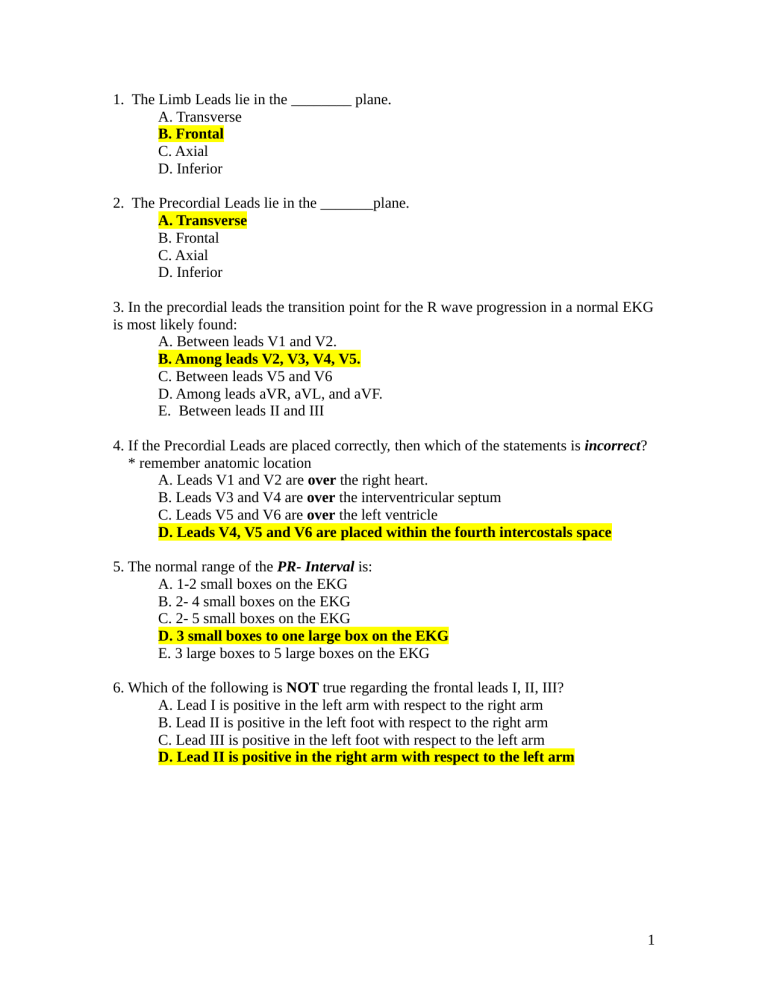
1. The Limb Leads lie in the ________ plane. A. Transverse B. Frontal C. Axial D. Inferior 2. The Precordial Leads lie in the _______plane. A. Transverse B. Frontal C. Axial D. Inferior 3. In the precordial leads the transition point for the R wave progression in a normal EKG is most likely found: A. Between leads V1 and V2. B. Among leads V2, V3, V4, V5. C. Between leads V5 and V6 D. Among leads aVR, aVL, and aVF. E. Between leads II and III 4. If the Precordial Leads are placed correctly, then which of the statements is incorrect? * remember anatomic location A. Leads V1 and V2 are over the right heart. B. Leads V3 and V4 are over the interventricular septum C. Leads V5 and V6 are over the left ventricle D. Leads V4, V5 and V6 are placed within the fourth intercostals space 5. The normal range of the PR- Interval is: A. 1-2 small boxes on the EKG B. 2- 4 small boxes on the EKG C. 2- 5 small boxes on the EKG D. 3 small boxes to one large box on the EKG E. 3 large boxes to 5 large boxes on the EKG 6. Which of the following is NOT true regarding the frontal leads I, II, III? A. Lead I is positive in the left arm with respect to the right arm B. Lead II is positive in the left foot with respect to the right arm C. Lead III is positive in the left foot with respect to the left arm D. Lead II is positive in the right arm with respect to the left arm 1 The following questions 7-11 are matching questions and the answers may be used more than once or not at all!!! A. Duration of ventricular depolarization and repolarization B. Junction of S and T wave C. Duration of ventricular depolarization D. Time onset from atrial depolarization to ventricular depolarization E. Repolarization of the ventricles 7. 8. 9. 10. 11. _D____PR Interval _C___QRS complex _B___ J point _E___ST segment and T wave _A___QT interval 12. True / False If clinically indicated, treatment of supraventricular tachycardia (SVT) consists of IV adenosine and vagal maneuvers. A. True B. False 13. True / False In a patient presenting with atrial fibrillation, immediate restoration to normal sinus rhythm is always the appropriate treatment. A. True B. False 14. An OMS III presents a patient and states that the R to R interval is ONE large box in its duration. What is the atrial rate of the patient? A. 300 BPM B. 150 BPM C. 100 BPM D. 75 BPM E. Unknown 2 15. Which of the above rhythm strips above represents Atrial Fibrillation, A or B? A Case History Question 16 – 75 year old male presents to the Emergency Department stating that he has passed out 2 times this morning after standing up. BP 130 /80 Respiratory rate – 12, Pulse oximetry – 98 % room air. 16. Which answer which best describes the above rhythm? A. Narrow complex bradycardia B. Normal sinus rhythm with aberrant conduction C. Accelerated idioventricular rhythm D. Ventricular tachycardia E. Indioventricular Accelerando Mundo 17. The above 75 y.o. male becomes unresponsive. You note a very weak femoral pulse which is bradycardic. Based on 2005 AHA ACLS guidelines, which of the following would be a reasonable intervention at this time. A. Transcuntaneous pacing B. Atropine C. Epinephrine D. Dopamine E. All of the above 3 18. Despite your intervention, the patient becomes pulseless. Based on this patient’s presentation, which of the following answers is the least likely cause of pulseless arrest? A. Coronary Thrombosis B. Hypoxia C. Hyperkalemia D. Tension pneumothorax E. Hypovolemia 19. The nurse states that the patient is “capturing”. Which of the following answers best explains what she means by this statement? A. External pacing of patient with symptomatic sinus bradycardia. B. Calculating the QT interval using Bazett’s equation C. Re- Entry of the electrical signal into the atria in the WPW D. Depolarization of the myocardium following the pacer spike 20. Which of the answers below best represents this rhythm? . FYI – disregard the numbers A. 3 rd Degree AV block B. 1 st Degree AV block C. Mobitz type 1, 2nd Degree AV block or Wenckebach D. Mobitz type 2, 2nd Degree AV block E. Marked sinus arrhythmia Match the following answers with the appropriate questions. Questions 21-24. Answers may be used once or more than once or not at all! A. 0 degrees to 90 degrees B. 90 degrees to 180 degrees C. 180 degrees to 270 degrees D. 0 degrees to – (neg) 90 degrees 21 Left axis deviation =__D____. 22. Right axis deviation =__B___. 23. Normal axis =__A___. 24. Severe right axis deviation =_C___. 4 For Questions 25 - 29, please choose the following answers to complete the statements below. A. Constant B. Irregular C. None of the above 25. In First Degree AV block, the PR interval is __A___. 26. In Sinus Arrhythmia, the PR interval is ___A____. 27. In Atrial Fibrillation, the PR interval is ___C____. 28. In Complete (Third Degree AV Block) Heart Block, the PR interval is __B___. 29. In Second Degree AV Block, Mobitz II, the conducted PR interval is __A____. Note the above tracing is for question #30 30. When viewing the above tracing ask your self the following questions. Are the P waves regular and are they associated with the QRS complexes? Which answer best describes this rhythm? A. Sinus arrhythmia with slow ventricular response B. 1St Degree AV Block C. Mobitz 1, 2nd Degree Type1 Block D. 3 rd Degree AV Block (Complete Heart Block) E. Mobitz 2, 2nd Degree AV Block, 31. True / False 2nd AV Block (Mobitz II) is considered a more serious life threatening block than Wenckebach, because it is sometimes followed by complete heart block ( 3rd AV Block ) A. True B. False C. The question is irrelevant 5 32. Which of the following answers best describes the above tracing? A. The ventricular rate is less than 60 BPM B. The QRS complex is wide (duration >0.12 ms) C. The P waves are disassociated from the QRS complexes D. This tracing represents 3 rd degree AV Block E All of the above 33. A 39 year old celebrity reported to have been drinking double shots of alcohol and taking methadone is found by EMS in her Florida hotel room unresponsive. You are an OMS III on EM rotation, you palpate no pulse. Pupils are mid, fixed and dilated. Which sequence is recommended by 2005 AHA ACLS guidelines? A. Chest compressions, defibrillation, vasopressor medication B. Pronounce the patient dead, claim to be the father of her children C. Defibrillation, vasopressor medication D. Epinephrine, vasopressin, magnesium and amiodarone 34 “R on T phenomena” refers to a time when an electrical stimulus can strike the latter portion of the T- wave in the”vulnerable period” (when the ventricles are hypersensitive) this might trigger ________ and possible sudden death. A. Ventricular Tachycardia B. Atrial Fibrillation C. MAT (multiatrial tachycardia) D. Atrial Flutter 6 Questions 35 – 37 35. Which of the following answers best describes the rate, rhythm and axis? A. Sinus bradycardia @50 bpm, normal axis B. Normal sinus rhythm @60 bpm, left axis C. Normal sinus rhythm@ 75 bpm, normal axis D. Normal sinus rhythm @60 bpm, normal axis 36. Which of the following best describes the QRS morphology? A. Wide complex QRS with R-R’in V1 B. Narrow complex QRS with R-R’in V6 C. Wide complex QRS with R-R’ in V6 D. Wide complex QRS with rabbit ears in V1 37. True / False A 75 year old male presents with a sudden onset of substernal chest pain radiating to his L arm and neck which started 2 hours ago. The nurse shows you an EKG from one week ago which is a NSR @ 75, normal axis and normal intervals. You quickly compare it to the above EKG. Should this be considered an ACUTE myocardial infarction? A. True B. False 7 Question 38 – 40 38. Which of the following best describes the rate, rhythm and axis? A. Sinus tachycardia@ 130 bpm, normal axis B. Atrial Fibrillation @130 bpm, L axis C. Atrial Fibrillation @130 bpm, R axis D. Atrial Fibrillation @130 bpm, normal axis 39. The patient is a 30 year old binge alcohol drinker. He is awake and alert and not complaining of chest pain. Based on the 2005 AHA ACLS guidelines, which would be the most appropriate intervention to control the heart rate? A. immediate synchronized cardioversion B. Precordial thump C. Beta Blocker or Diltiazem IV D. Atropine IV E. 4 chewed 81 mg Asprin 40. Which of the following answers best describes the QRST morphology? A. Narrow complex QRS B. Wide complex QRS C. Wide complex QRS with ST segment elevation in III and aVF D. Narrow complex QRS with ST segment elevation in III and aVF 8 Questions 41 – 43 41 When describing a completed purely inferior transmural myocardial infarction one expects Q waves in which lead(s)? A. Lead II B. Lead III C. Lead aVF D. All of the above E. None of the above 42. 54 year old male with hypertension, diabetes, and hyperlipidemia present to the EM stating that he has a crushing pressure across his chest. The pain started 2 hours ago. He appears pale, diaphoretic and short of breath. Which of the following intervention is the best combination for this patient? A. O2, IV, moniter, asprin, nitroglycerin and beta blocker B. IV, O2, cardiac moniter, nitoglycerin and morphine C. Immediate thrombolytics (no additional questions are required) D. IV, atropine, transcutaneous pacing, nitroglycerin E. Precordial thump 43. This infarction pattern represents which coronary artery? A. Left main B. Left anterior descending C. Left circumflex D. Obtuse marginal E. Right coronary artery 9 Questions 44- 45 44. Which answer best describes this EKG? A. NSR @81, Right axis, RBBB, 2nd Degree type I AV block B. NSR @ 81, Right axis, LBBB, 1st degree AV block C. NSR @81, Left axis, LBBB, 1st degree AV block D. NSR @81, Right axis, RBBB, 1st degree AV block 45 Which of the following clinical scenarios could explain this EKG? A. Left ventricular hypertrophy B. Pulmonary embolism C. Hyperkalemia D. Hypothermia E. None of the above 46. To conclude that a normal sinus rhythm is present you must see: A. QRS complexes B. Heart rate from 60 to 100 C. P waves preceding each QRS complex D. all of the above E. None of the above 10 Questions 47 -48 47. 64 year female states that’s she has had intermittent chest pain, shortness of breath and sweating for the last 3 days lasting approx. 30 minutes. She denies prior history of myocardial infarction. Which answer best describes this EKG? A. NSR @ 64, R axis and anterior / lateral wall myocardial infarction B. NSR @64, L axis and anterior / lateral wall myocardial infarction C. NSR @64, R axis and anterior /lateral wall ischemia D. NSR @64, L axis and anterior /lateral wall ischemia E. None of the above 48. Which coronary artery is most likely involved? A. Obtuse marginal B. Right C. Left circumflex D. Left anterior descending E. Unknown 49. To correct for the effect of heart rate on the QT interval you must divide the measured QT interval by: A. The square root of the QRS complex B. The square root of the PR interval C. The square root of pie D. The square root of the R-R interval 11 50. What is the condition that is associated with tachyarrythmias, shortened PR interval and a Delta wave that may produce intermittent symptoms in otherwise young healthy individuals? A. Marfans Syndrome B. Wolff – Parkinson – White (WPW) C. Left Posterior Fasicular block D. Paroxysmmal Supraventricular Tachycardia 12 Answers: 1. B 2. A 3. B 4. D 5. D 6. D 7. D 8. C 9. B 10. E 11. A 12. A 13. B 14. E 15. A 16. C 17. E 18. D 19. D 20. C 21. D 22. B 23. A 24. C 25. A 26. A 27. C 28. B 29. A 30. D 31. A 32. E 33. A 34. A 35. D 36. C 37. A 38. D 39. C 40. D 41. D 42. B 43. E 44. D 13 45. B 46. D 47. D 48. E 49. D 50. B Question Answer IF there is a Pwave, the rhythm will be one of theses Sinus Rhythms: Sinus Rhythm: Normal Sinus Rhythm, Sinus Bradycardia or Sinus Tachycardia If you do not have a P-wave the Ventricular rhythm is: Determine the Rate: 60-100 (NSR or AJR)<60 (SB, or JR)> 100 (ST or JT) PR Interval = <.12 (less than 3 little = Junctional Rhythm, nextlook at rate boxes) PR Interval = . 12-.20 = (3 to 5 little boxes) = Sinus Rhythm, Sinus Brady, Sinus Tach PR Interval = >.20 1st degree heart block. Type of rhythnm = with 1st degree heart block No P-wave= Ventricular Tachacardia, ideoventricular, Atrial flutter, Fixed conduction (...!...!...!) Regular QRS = 0.06-0.10 Super Ventricular Tachycardia <3 little boxes When do you cardiovert When you have a pulse When do you Defibulate When you have no pulse What drug(s) do Epinephrine, and atropine 14 you use for Asystole The drug used to Chemicaly Cardiovert SVT is Adenosine Fear, Deficient knowledgeIneffective cardiac tissue perfusion, Decreased cardiac output, Nursing Diagnosis Impaired gas exchange, Risk for imbalanced related to CABG fluid volume, Disturbed sensory perception, Acute pain, Ineffective tissue perfusion, Ineffective thermoregulation CVP normal value:Wedge pressure:PAP CVP:0-4 Wedge pressure:8-15 PAP 20-30/515 Massive left sided heart failure, full of fluid, pink frothy secretions, Treatment: diuretics Pulmonary Edema (lasix first line)If pt has renal failure then (nitroglycerin and morphine) Irregular Rhythms A-flutter, Sinus Arrhythmia, 2 degree or 3 degree heart block, A-fib Narrowing pulse pressure would be Tamponade, also massive JVD seen in which patient Pacemaker Information required on Chart Model of pacemaker, type of generator, date and time of insertion, location of pulse generator, stimulation threshold, Pacer settings (eg, rate, energy output, sensitivity, and duration of interval between atrial and ventricular impulses) Endocarditis Infective Risk factors Risk factors: heart valve prosthesis, hx of heart disease (mitral valve prolapse), chronic dibilitatin disease, IV drug abuse and immunosuppression Pericarditis Friction rub. notched T wave, S/S: fever, positional chest discomfort, nonspecific ST- 15 segment elevation, elevated ESR erythrocyte sedimentation rate, retrosternal pain that worsens during supine positioning, pulsus paradoxus hypokalemia wave U uaves after the T form changes hyperkalemia Tall QRS complexes hypomagnesium Torsades de pointes Medications to treat ventricular dysrhythmias Lidocaine, Beta blockers, amiodarone (drug of choice for v-tac) JVD, Dependent Edema, right upper gastric Right Heart Failure pain(Right heart handles systemic blood (chronic condition) return) Left Heart Failure Bibasilar fine crackles, dyspnea, tachycardia, S3 and S4 heartsounds,fatigue, hemoptysis, non-productive cough, cool pale skin, PMI displaces toward the left anterior axillary line Inferior wall myocardial Infarction T-wave inversion:inadequate blood supplyST-segment elevation:injury prolonged ischemiaPathologic Q waves Are all signs of tissue hypoxia Digoxin Hold if apical pulse is less than 60 bpm. Digitalis Toxicity = vision changes (halos), dysrhythmia, anorexia, nausea, vomiting, headache, and malaise. Increases force of myocardial contraction and decreases HR. A-fib Warfarin to prevent clots and decrease risk of stroke, Digoxin to control HR 12 Lead EKG ST elevation indicates immediate myocardial injury. ST depressions indicate myocardial ischemia. Q wave forms several days after a myocardial infarction, U wave is a sign of hypokalemia. Laxix Furosemide IV push: give at a rate of 20 mg/min or less. 16 Rapid injection can cause hearing loss as a result of ototoxicity.Normal daily dose: 40 mg. loop diuretic Nitroglycerin Reduces oxygen consumption to devrease ischemia and relieve pain. Vasodialator mainly in veins and reduces blood return to heart and preload is reduced. May cause a significant drop in cardiac output and B/P if pt is hypovolemic at higher doses. Calcium Channel Blockers Slows heartrate and decreases strength of contraction which decreases workload of heart. Relaxes blood vessels decreasing BP and increases coronary artery perfusion Rhumatic Fever Caused by strep S/S of Infective Endocarditis Osler's nodes (red, painful nodules on the fingers and toes) splinter hemorrhages, fever, diaphoresis, hoint pain, weakness, abdominal pain, new murmur, Janeway's lesions (small, hemorrhagic areas on fingers, toes, ears, and nose) Myocarditis S/S Flu-like symptoms.fatigue, dyspnea, palpitations, and occasional discofort in the chest and upper abdomen. My develop dysrhythmias, or ST-T wave changes. Systolic murmur, gallop rhtyhm, ACE Inhibitors promote vasodilation and diuresis by decreasing afterload and preload. Dobutamine left ventricular dysfunction. increases cardiac contractility. at high doses, it also increases HR and incidence of ectopic beats and tachydysrhythmias. take care in pt with a-fib. CK-MB earliest 4-8 hours, peaks 12-24 hrs, and returns to increase, peak and normal 1-3 weeks return to normal Troponin earliest 3-4 hours, peaks in 4-24 hrs and returns to 17 increase, peak and normal 1-3 weeks return to normal Labs for Heart failure BUN, TSH, CBC, BNP Mitral stenosis: Rhythms, S/S S/S: dyspnea, progressive fatigue, hemoptysis, paroxysmal nocturnal dyspnea, chough, wheeze, repeated respiratory infections. Dysrhythmias like A-fib. Tests Doppler echocardiography. Aortic Regurgitation: Cause Caused by inflammatory lesions that deformt he leaflets of the aortic valve. also infective or rheumatic endocarditis, congenital abnormalities, diseases such as syphilis, dissecting aneurysm, blunt chest trauma, or valve replacement. Forceful heartbeats in head and neck, arterial pulsations that are visible or Aortic palpable at the carotid or temporal arteries. Regurgitation: S/S Exertional dyspnea, fatigure, progressive s/s of left ventricular failure includie breathing difficulties, orthopnea, PND. take long term anticoagulant therapy, Valve replacement freequent follow up appointsments and teaching: pre and blood lab studies. mak need to take aspirin, post precribed medication teaching, Cardiac Tamponade S/S Life threatening need stat interventions. S/S fullness within the chest, substantial or ill defined pain. sob, massive JVD, falling systolic blood pressure, narrowing pulse pressure, rising venous pressure (increased JVD) and distant heart sounds Cardiac Tamponade treatment pericardiocentesis, pericardiotomy (pericardial window) CABG: 70% occlusion (60% if in the Left main). artery must me patent beyond the occlusion. Use greater saphenous vein, 18 lesser saphenous, chephalic and basilic veins. 19 20