THE RESPIRATORY SYSTEM
advertisement

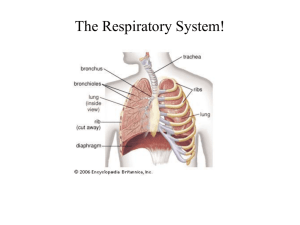
THE RESPIRATORY SYSTEM Diane Hickson-Bick, PhD. Reading: Gartner and Hiatt, Chapter 12, p 235; Klein and McKenzie, pp199-210. Learning Objectives: Understand the differences between the conducting and respiratory portion of the respiratory system. Define the roles and composition of these two regions. Key Words: Conducting, respiratory, alveoli, cartilage, trachea, bronchus, bronchioles, vocal cords. The respiratory system The means by which, through a system of tubes, the body exchanges carbon dioxide for oxygen, which is then distributed throughout the body. 2 Parts: An upper conducting portion and a lower respiratory portion. A. CONDUCTING PORTION Consists of the extra-pulmonary nasal cavity, nasopharynx, larynx, trachea, bronchi and the intrapulmonary bronchi, bronchioles and terminal bronchioles. It serves two main roles: 1. To provide a conduit through which air can travel to and from the lungs 2. To condition the inspired air. Components of the Conducting System Cartilage (primarily hyaline) from C-shaped rings to irregular rings and small plaques. Prevents collapse of the walls. Collagen fibers Elastic Fibers: Tend to be oriented longitudinally in this area. Smooth muscle: From trachea to alveolar ducts. Contraction reduces diameter of tubes and restricts airflow Respiratory Epithelium Lines the conducting portions Ciliated, pseudostratified columnar epithelium Does not mediate gas exchange. Functions to cleanse, moisten and warm air before it enters the lungs. Numerous serous and mucous glands and a rich superficial vascular network in lamina propria. Goblet cells, producing a rich mucous secretion, abundant in the upper portions of the conducting tubes. The number of goblet cells, along with the amount of ciliated epithelium and cartilage, decrease as the conducting tubes gradually proceed into the respiratory portion. At the same time the content of smooth muscle and elastic fibers progressively increases. Ciliated pseudostratified columnar epithelium transitions to a simple columnar and finally a simple squamous epithelium in the alveoli. The rich goblet cell population tapers off in the smaller bronchi and these cells are absent from the terminal bronchioles. Ciliated cells continue beyond the goblet cells, preventing the accumulation of mucous. Cilia move fluid and mucus toward the oral cavity where it is swallowed or expectorated. Respiratory epithelium consists of 5 cell types: 1. Ciliated columnar cells; Most abundant, each having about 300 cilia on their apical surface. Many apical mitochondria provide energy for beating. 2. Mucous goblet cells; Contain polysaccharide-rich mucous droplets. 3. Brush cells; Many microvilli on their apical surface and afferent nerve endings on their basal surfaces; considered to be sensory receptors. 4. Basal (short) cells; Small round cells lie on the basal lamina, do not extend to the luminal surface. Believed to be generative cells and give rise to other cell types by mitosis. 5. Small granule cells; Resemble the basal cell but contain numerous dense granules and form part of the diffuse neuroendocrine system. Table 1 B. RESPIRATORY PORTION Consists of alveolar ducts, sacs and pores. Gas exchange occurs between the alveolar and capillary lumen, across the squamous epithelium of alveolar pneumocytes and the capillary endothelium. Nasal CONDUCTING Trachea Bronchi Large Pseudo/ Pseudo/ Pseudo/ columna columna columna r r r +++ +++ +++ +++ +++ ++ +++ ++ ++ + +++ ++ --+ + + + ++ Larynx Bronchioles Large Small Pseudo/ Simple/ columna cuboid r +++ +++ + ----------++ + ++ ++ RESPIRATORY Alveoli Small Pseudo/ Pseudo/ Simple/ columna columna Squamous r r Cilia +++ +++ --Goblet +++ + --Glands +++ + --Cartilage + + --Muscle --+ --Elastic --++ +++ NASOPHARYNX First part of the pharynx, continuous with the oropharynx. It is lined with respiratory epithelium where it is in contact with the soft palate. LARYNX An irregular tube that connects the pharynx to the trachea. Number of laryngeal cartilages found within the lamina propria. Most of these cartilages are hyaline but some of the smaller ones are elastic cartilage. The epiglottis projects from the rim of the larynx extending into the pharynx. The lingual surface of the epiglottis is covered by a stratified squamous epithelium that transitions to a ciliated pseudostratified columnar epithelium on the laryngeal side. Mucous and serous glands are also present in the lamina propria beneath the epithelium. Below the epiglottis the mucosa forms two pairs of folds that extend into the lumen of the larynx. The upper pair are the false, or vestibular, vocal cords which are covered by typical respiratory (ciliated pseudostratified columnar) epithelium beneath which are numerous serous glands. The lower pair of folds are the true vocal cords. Large bundles of elastic fibres composing the vocal ligaments lie within the true vocal cords. Parallel to the ligaments are bundles of skeletal muscle, the vocalis muscle. The true vocal cords are covered by a stratified squamous epithelium. Epitheliu m TRACHEA A thin walled tube approximately 10cm long extending from the larynx to the point at which it divides into the two main bronchi. Lined with a typical respiratory epithelium. 16-20 c-shaped rings of hyaline cartilage in lamina propria keep the tube open. Fibroelastic cartilage and a bundle of smooth muscle (trachealis muscle) bridge the two ends of the cartilage. Contraction of this muscle narrows the lumen and is used in the cough reflex. BRONCHIAL TREE The trachea divides into two primary bronchi. After entering the lungs the primary bronchi give rise to lobar bronchi which supply a pulmonary lobe. There are three lobar bronchi in the right lung and two in the left. Lobar bronchi divide repeatedly giving rise to smaller bronchi whose termini are the bronchioles. Each bronchiole enters a pulmonary lobule where it branches to form 5-7 terminal bronchioles. Primary bronchi histologically resemble the trachea however as one proceeds towards the respiratory portion the epithelium and lamina propria become simplified. Bronchi: Bronchial diameter decreases. Cartilage rings are replaced with isolated plates, or islands, of hyaline cartilage. In the lamina propria are bundles of smooth muscle which become more prominent near the respiratory zone. The lamina propria also contains many elastic fibers, abundant mucous and serous glands and many lymphocytes along with lymphatic nodules. Bronchioles: Intralobular airways with diameters of 5mm or less. Mucosa contains no glands or cartilage. In the larger bronchioles the epithelium is ciliated pseudostratified columnar which decreases in height to become ciliated simple columnar or cuboidal epithelium in the terminal bronchioles. Within the terminal bronchioles the epithelium also contains Clara cells. These cells have no cilia but contain secretory granules and secrete glycosaminoglycans that serve to protect the epithelium. The lamina propria contains mainly smooth muscle and elastic fibers. Respiratory Bronchioles: Each terminal bronchiole divides into 2+ respiratory bronchioles where the conducting portion transitions into the respiratory portion. The mucosa of the respiratory bronchioles resembles that of terminal bronchioles except the walls are interrupted by numerous saccular alveoli, sites of gas exchange. At the rim of the alveolar openings the ciliated cuboidal epithelium becomes continuous with the squamous alveolar lining cells. Alveolar Ducts: Where the number of alveolar openings increases to the point that the bronchial wall disappears the tube. Squamous alveolar cells line alveolar ducts and alveoli. In the lamina propria, around the rim of he alveoli, is a network of smooth muscle cells that appear as knobs between adjacent alveoli. This smooth muscle disappears at the distal ends of the alveolar ducts. Alveolar ducts open into atria, which communicate with alveolar sacs. A complex network of elastic and reticular fibers encircle the atria, alveolar sacs and alveoli. Alveoli Saclike structures about 200M in diameter. Approximately 300 million of these with a surface area of 140m2 form the spongy structure of the lungs. Within these specialized structures oxygen and carbon dioxide are exchanged between air and blood. Each alveoli wall usually lies between two neighbouring alveoli and is called an inter-alveolar septum. An alveolar septum consists of two thin squamous epithelial layers between which lie capillaries, fibroblasts, elastic and reticular fibers and macrophages. The capillaries and the connective tissue form the interstitium. This interstitium contains the richest network of capillaries within the body. The inter-alveolar septum may contain one or more pores known as the pores of Kohn. These pores connect neighbouring alveoli and can equalize pressure or allow collateral circulation when an alveolus is blocked. Alveolar macrophages can also pass through these pores. Air in the alveoli is separated from blood in the capillary by three components called the bloodair barrier: Components of the blood-air barrier 1. Surface and cytoplasm of the alveolar cells. 2. Fused basal laminae of the alveolar cells and the capillary endothelial cells; 3. The cytoplasm of the endothelial cells. The total thickness of this barrier varies from 0.1-1.5M. Reticular fibers within the septum act as support for the anastomosing capillary network. Oxygen from the alveolar air diffuses through the layers of the alveolar septum whilst carbon dioxide diffuses in the opposite direction. The inter-alveolar septum consists of 5 main cell types: 1. Capillary endothelial cells, very thin and non-fenestrated. 2. Type I alveolar (squamous) pneumocytes. Very attenuated cells, 97% of the alveolar surface. All have desmosomes and tight occluding junctions so form a gas permeable barrier of minimal thickness. 3. Type II pneumocytes. Interspersed among the type I cells. Roughly cuboidal and usually found in groups of 2-3 at points where the alveolar walls unite and form angles. Resemble secretory cells with a well-developed Golgi network and microvilli on their apical surface. They have a foamy, vesicular cytoplasm caused by the presence of lamellar bodies containing lipid, glycosaminoglycans and protein. These lamellar bodies are continuously synthesized and released from the apical surface providing an alveolar coat or pulmonary surfactant that lowers alveolar surface tension. 4. Interstitial cells including fibroblasts and mast cells. Fibroblasts synthesize collagen, elastic fibers and GAGs. Collagen and elastic fibers add resilience and elasticity to the mechanical properties of the lungs. 5. Alveolar macrophages or Dust cells. Derived from monocytes. Can be found in the interior of the septum or on the surface of the alveolus. They can often contain large amounts of carbon and dust, which they phagocytose from the alveolar lumen. PULMONARY BLOOD VESSELS Systemic (bronchial) system: Follows the bronchial tree and supplies nutrients to the lung tissue up to the respiratory bronchioles. At this point these vessels anastomose with the small branches of the pulmonary artery and return blood via the pulmonary vein. Bronchial arteries branch from the aorta and thus carry blood at systemic pressure. Bronchial arteries have smaller lumens and thicker walls than pulmonary arteries. Their walls contain a distinct elastic lamina and a muscular media. Functional (pulmonary) system Pulmonary arteries are low-pressure vessels with thin walls. These vessels have an internal elastic lamina, smooth muscle and elastic fibers. Within the lung the pulmonary artery branches following the bronchial tree. At the level of the alveolar duct the branches form a capillary network in the inter-alveolar septum. Venules originate from the capillaries and enter the interlobular septum finally leaving the lobule to follow the bronchial tree to the hilum. PULMONARY LYMPHATIC VESSELS These follow the bronchi and pulmonary vessels and can occur in the interlobular septum. All drain into lymph nodes at the hilum. No lymphatics in the terminal portion of the bronchial tree or beyond the alveolar ducts. PLEURA A serous membrane covering the lungs. It consists of two layers, parietal and visceral, which are continuous at the hilum. Both membranes consist of a thin squamous mesothelium resting on a connective tissue layer containing collagen and elastic fibers. Under normal circumstances the space between these two layers is filled with a layer of fluid that acts as a lubricating agent. RESPIRATORY LAB SLIDE 46 – LARYNX Identify the following: Ventricle – a large fold invaginating from the lumen with vocal cords on opposite sides False vocal cords – ciliated pseudostratified respiratory epithelium and underlying glands True vocal cords - Non-keratinized, stratified squamous, underlying muscle, NO glands Glands – mucous and seromucous Lymphoid nodules – BALT Cartilage – what type? SLIDE 12 – TRACHEA Identify: Ciliated pseudostratified, goblet cells, basal cells, brush cells Basement membrane Elastic fibers (look in submucosa) Glands – What types are here? Blood vessels Hyaline cartilage Smooth muscle and connective tissue joining ends of cartilage ring SLIDE 47 – BRONCHUS Identify: Respiratory epithelium Bronchial lumen Cartilage – hyaline plates Glands Smooth muscle SLIDE 48 – LUNG Identify: Bronchioles; No cartilage, smooth muscle, ciliated epithelium Alveolar ducts and sacs Blood vessels in alveolar walls Type I pneumocytes – flat in alveolar walls Type II pneumocytes – surfactant; in angular regions and quite puffy looking Clara cells – domed shape in bronchioles Macrophages – Large cells in alveoli SLIDE 49 – LUNG – VVG STAIN Identify: Elastic fibers Collagen (Looks pinkish) Alveoli Bronchiole muscularis