Respiratory System
advertisement

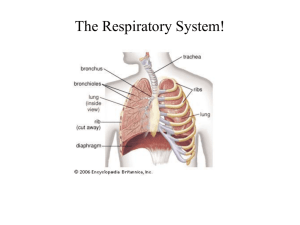
Respiratory System Medical Cell and Tissue Biology Dr. Cathleen Pettepher March 18, 2002 Larynx Framework of hyaline & elastic cartilages – False vocal folds – Ventricles – Vocal folds: • glottis – Vocalis muscle Vocal Folds – two mucosal folds – stratified squamous epithelium – protects the mucosa from abrasion caused by the rapidly moving airstream Contains: – a supporting ligament – vocalis muscle (VL) • generates tension in vocal fold Larynx Remainder of the larynx is lined with ciliated, pseudostratified columnar epithelium CT contains: – mixed mucoserous glands Laryngeal Glands Secrete via ducts onto the surface along rim of aryepiglottic folds & ventricular folds absent from vocal ligaments, reappear toward base of vocal fold Trachea Hollow, flexible tube – Begins at larynx – Ends at carina Bifurcates to form 1º bronchus for each lung reinforced by a skeleton of cartilage Consists of 4 layers – Mucosa – Submucosa – Cartilaginous layer – Adventitia Trachealis muscle - bridges gap between ends of cartilage – smooth muscle Tracheal Mucosa Secretory mucosa – contains exocrine glands Pseudostratified columnar epithelium – ciliated cells & mucous cells predominating – other cell types present but poorly resolved with LM Varies in appearance – sensitive to irritation – responds by increasing in height • mucous cells and glands undergo hypertrophy – with prolonged irritation • portions of epithelium may become stratified squamous epithelium • termed squamous metaplasia Tracheal Epithelium 5 different cell types present in the epithelial layer high levels of activity for mitochondrial and lysosomal enzymes – associated with oxidative phosphorylation – attributed to ciliated and mucous cells Ciliated Cells Mitochondria: – concentrated just beneath the basal bodies in the apical cytoplasm contain cilia and microvilli – ~300 cilia per cell Mucous Cells Exhibit characteristics of protein-secreting cells: – extensive ER in basal region of cell – supranuclear Golgi apparatus – coalescing mucous droplets in apical cytoplasma Basal Cells Non-ciliated epithelial cells Nuclei form a row close to the basal lamina These cells do not extend to the free surface Function as a reserve population for the epithelium Brush Cells Non-ciliated cells contain long, straight microvilli Some form epithelio-dendritic (afferent) synapses with nerve processes in CT May possess glycogen granules and a lot of sER Small Granular Cells Rare cells – Kulchitsky cells (K) – solitary & sparsely dispersed Characterized by small dense-core granules APUD cell – they take up amine precursors & store them in granules Epithelial Renewal All epithelial elements are joined to each other on the sides by desmosomes and if they reach the surface, by junctional complexes After trauma, neighboring mucous & basal (short) cells migrate to cover the denuded area – They lose their distinguishing characteristics – They divide and form a population of immature cells – these in turn divide and redifferentiate into mucous and ciliated cells Lamina Propria Loose CT containing: – interwoven collagenous & elastic fibers – many vascular channels – fixed & wandering CT cells Elastic fibers: – run in a predominantly longitudinal direction – interconnected by slender fibrils – peripherally these fibrils condense into an elastic membrane demarcating the lamina propria from the submucosa Submucosa fewer elastic fibers and more collagen fibers fibers run in bundles among the seromucous glands blends into peri-chondrium of the cartilages Intrapulmonary Bronchi Mucosa Muscularis – continuous layer of smooth muscle that maintains appropriate diameter of airway Submucosa Cartilaginous layer: – discontinuous plates – become fewer in # Adventitia Bronchioles (1 mm or less) Bronchopulmonary segments are further divided into pulmonary lobules with each lobule supplied by a bronchiole delicate CT septa separate adjacent lobules pulmonary acini are smaller units of structure that make up each lobule Respiratory bronchiolar unit: – smallest functional unit of pulmonary structure – consists of single respiratory bronchiole and the alveoli that is supplies these branch > smaller terminal bronchioles – final segments of conducting portion of respiratory system these branch >> respiratory bronchioles – contain alveoli – 1st respiratory unit of lung Epithelium gradually transforms to simple ciliated columnar epithelium – goblet cells present no submucosal glands present cartilaginous plates are replaced with a thick layer of smooth muscle Terminal Bronchioles Simple cuboidal epithelium – contains Clara cells that are found among the ciliated cells – occasional brush cells and dense core granular cells are present Circumferential layer of smooth muscle Clara Cells Non-ciliated cells with dome-shaped apical surface Secretory granules – Secrete a surface-active lipoprotein – prevents luminal adhesion should the wall of the airway fold on itself -- especially during expiration Respiratory Bronchioles Transitional zone – concerned with both air conduction & gas exchange Cuboidal epithelium: – Clara & ciliated cells Alveoli – thin-walled outpocketings – sites where gas exchange occurs Alveolar Ducts and Sacs Alveolar ducts: – elongated airways with few walls – alveoli act as their peripheral boundary Alveolar sacs: – surrounded by clusters of alveoli which open up into these spaces Terminal Air Spaces -- Alveoli Actual site of gas exchange between air and blood 100 million alveoli per lung thin-walled polyhedral chambers rings of smooth muscle in knob-like intra-alveolar septum Alveolar Epithelium Simple squamous epithelium composed of 3 cell types: – – – Alveolar type I cells Alveolar type II cells Brush cells Alveolar Macrophages dust cells – function both in CT of the septum and in the air spaces – scavenge the surface to remove inhaled particulate matter – also phagocytize red blood cells that may enter the alveoli in heart failur -- heart failure cells Alveolar Type I cells Pneumocytes extremely thin squamous cells line 95% of the alveolar surface deficient in most organelles joined to one another and other cells by zona occludens Alveolar Type II Cells Secretory (exocrine) cells Cuboidal cells that bulge into air space granules that contain stacks of parallel membrane lamella rich in phospholipids -surfactant forms a mono-molecular layer that reduces surface tension Alveolar Septum alveolar epithelial cells basal lamina of epithelial cells often fused with basal lamina of capillary endothelial cell endothelial cells Thin portion contains: – surfactant – Type I pneumocytes – basal lamina -- basal lamina – capillary endothelial cell Thick portion may contain CT cells & fibers --fluid can accumulate