Quality Improvement Data Collection Tool
advertisement

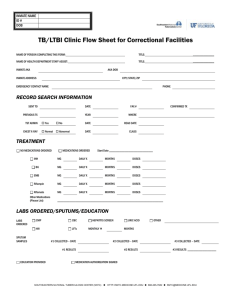
Quality Improvement Data Collection Tool TB – Active Cases/Suspects Facility Sample Size Data Collector(s) Date DATA COLLECTED # 1 1 Is date of incarceration listed/ documented? 2 Were there symptoms on admission to the facility? 3 4 Were the smear results positive? 6 Was NAAT/MTD test done? 7 Were the culture results positive? 8 Was the TST/IGRA positive? 9 Was the CXR result on chart? 10 Was the inmate placed on recommended 4-drug therapy? 11 Were initial liver enzymes normal at baseline? 12 Was HIV counseling and testing done? 13 Were the results of the HIV and other lab tests on the chart? 14 If positive smear/culture, were contacts identified? 16 17 2 3 4 5 6 7 8 9 10 THRESHOLDS + - 0 (yes) (No) (N/A) COMMENTS GOAL ACTUAL Was the inmate isolated in an Airborne Infection Isolation (AII) room within 5 hours of the first symptom? Was the health department notified within the appropriate timeframe of the suspect case? 5 15 TOTALS INDICATOR If positive smear/culture, were contacts evaluated? Was appropriate therapy initiated for LTBI contacts? Was initial contact information given to HD within 7 days? PUT CHART IDENTIFYING INFORMATION HERE SOUTHEASTERN NATIONAL TUBERCULOSIS CENTER (SNTC) HTTP://SNTC.MEDICINE.UFL.EDU 888-265-7682 SNTC@MEDICINE.UFL.EDU Instruction Tool 1. Is the date of incarceration listed? This is a computergenerated date and can be obtained from Classifications or the computer. The content of these cells will not be +/-, but should identify the date the inmate came into the facility. NOTE: This date will be important to identify potential teaching opportunities during the intake process if the inmate is not identified early into the incarceration. 2. Were there symptoms on admission to the facility? This can be obtained from the intake sheet or a TB or cough questionnaire the facility may have developed. NOTE: This information indicates a potential for education that may be needed in the Intake area or follow-through that may be needed. 3. Was the inmate isolated within five hours of the first symptom? Check for documentation in the progress notes of the chart or a date/time on a Sick Call Slip or Isolation log. NOTE: This will assist in the event a contact investigation is needed. 4. Was the health department notified within the appropriate time frame of the suspect case? This can be identified from the HD record as well as the facility record. Documentation can be located within the progress notes of the record or a specific area. The time frame is identified to meet local/state laws. 5. Were the smear results positive? This will assist in prioritizing contact investigations, as well as identifying a need for focus studies with regard to collection of the sputum. NOTE: If any of the sputum is inadequate or overgrown, or not cooled when transporting, this would indicate a need for education for adequate collection of sputa. 6. Was NAAT/MTD test done? This should be done on all sputum samples submitted initially. NOTE: This is an identification tool that can facilitate early release from isolation. [NAAT = nucleic acid amplification; MTD = mycobacterium tuberculosis direct] 7. Were the culture results positive? This is documented on the lab slips. Note: this information will assist in identification of prioritizing contact investigations, as well as identifying a need for education of collection of sputa. 8. Was the TST/IGRA positive? The results of the tuberculin skin test must be documented in millimeters. NOTE: Aids in identifying issues with regards to TST (tuberculin skin testing) or IGRA (immune gamma response assay) and education for providers. The statement “negative” or “positive” is not appropriate for TST. If TST is negative, it should be documented as “0 mm”. 9. Was the CXR result in the chart? A copy of the results of the recent chest x-ray should be located in the chart. NOTE: This is a CXR form, not a notation in the progress record. This is a “yes” or “no” in all cases, and would be “Not Applicable” only if no CXR was ordered. 10. Was the inmate placed on recommended four-drug therapy? This includes Isoniazid, Rifampin, Ethambutal and Pyrazinamide (INH, RIF, ETH, and PZA). Other regimens require documentation of consult with a TB expert. This information is documented on a physician’s order. NOTE: If sensitivities were returned with resistance to any of these, the inmate would be changed to different TB medications. Special Note: If low level resistance to INH, some MDs will keep INH in the regimen. Consult with a TB expert. SOUTHEASTERN NATIONAL TUBERCULOSIS CENTER (SNTC) 11. Were initial liver enzymes normal at baseline? This would be a “yes” or “no” response. NOTE: The lab slip would indicate the liver enzymes, such as SGOT, SGPT and Bilirubin and the range. 12. Was HIV counseling and testing done? There would be documentation stating the client was offered counseling and testing or a lab slip with refusal. NOTE: Documentation would be on a form or a lab slip, a refusal or on a progress note (may include signature). This would be Not Applicable if the facility does not include HIV counseling and testing in their policy, although it is recommended for every facility. 13. Were the results of the HIV and other lab tests on the chart? A lab slip, indicating positive or negative, should be in the chart. Include all other applicable lab tests, such as viral load, CD4 count. NOTE: The only time this would be “not applicable” would be if no labs or HIV test was ordered. 14. If positive smear or culture, were contacts identified? There is generally an indication in the chart’s progress note that a contact investigation was initiated, and, if done, a sheet either with the chart or a total number of contacts identified should be included. This would be “not applicable” if the client was extrapulmonary or documentation by HD staff no contact investigation was needed. NOTE: A contact investigation should be done for every pulmonary case of tuberculosis. If positive smear or culture, were contacts evaluated? This can be located on a contact evaluation sheet that would be included with the inmate record, or in a separate file from Infection Control. NOTE: This would be “not applicable” if the client was extrapulmonary or documentation by HD staff no contact investigation was needed. Contact evaluation is important to ensure no new cases of tuberculosis are missed. 15. Was appropriate therapy initiated for LTBI contacts? A physician’s order for INH or Rifampin therapy is documented in the doctor’s orders. NOTE: This would be INH (Isoniazid) for nine or six months, depending on the length of stay of the inmate. Rifampin for four months should be used for inmates staying at the facility for at least six months and only under the guidance of a TB physician and directly observed treatment. 16. Was initial contact information given to the HD within seven days? Documentation in the form of a Progress Note would satisfy these criteria. NOTE: This would be “Not Applicable” if the patient had extrapulmonary TB. This information is essential to ensure appropriate follow-up and completion if the client is released from the facility. Put Chart Identifying Information Here This area of the form is for documenting the initials or number of the client’s chart for follow-up at a later date, if needed. HTTP://SNTC.MEDICINE.UFL.EDU 888-265-7682 SNTC@MEDICINE.UFL.EDU