What is otitis media
advertisement
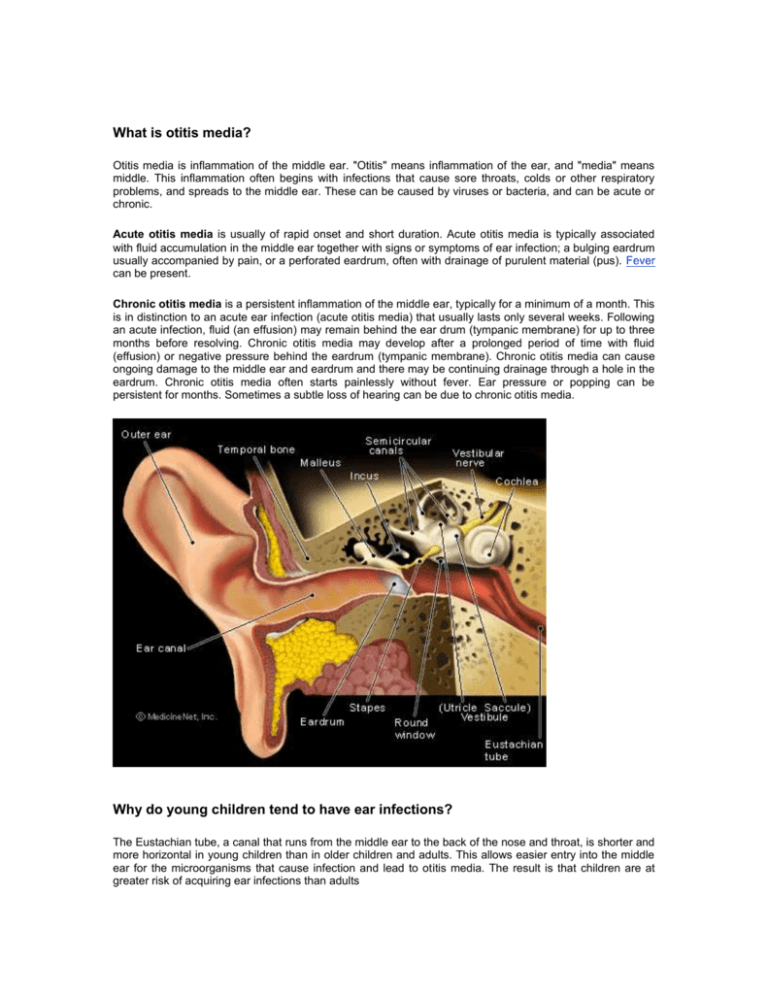
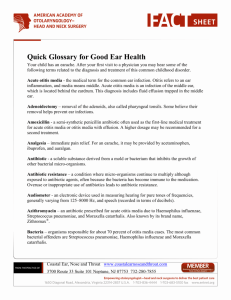
What is otitis media? Otitis media is inflammation of the middle ear. "Otitis" means inflammation of the ear, and "media" means middle. This inflammation often begins with infections that cause sore throats, colds or other respiratory problems, and spreads to the middle ear. These can be caused by viruses or bacteria, and can be acute or chronic. Acute otitis media is usually of rapid onset and short duration. Acute otitis media is typically associated with fluid accumulation in the middle ear together with signs or symptoms of ear infection; a bulging eardrum usually accompanied by pain, or a perforated eardrum, often with drainage of purulent material (pus). Fever can be present. Chronic otitis media is a persistent inflammation of the middle ear, typically for a minimum of a month. This is in distinction to an acute ear infection (acute otitis media) that usually lasts only several weeks. Following an acute infection, fluid (an effusion) may remain behind the ear drum (tympanic membrane) for up to three months before resolving. Chronic otitis media may develop after a prolonged period of time with fluid (effusion) or negative pressure behind the eardrum (tympanic membrane). Chronic otitis media can cause ongoing damage to the middle ear and eardrum and there may be continuing drainage through a hole in the eardrum. Chronic otitis media often starts painlessly without fever. Ear pressure or popping can be persistent for months. Sometimes a subtle loss of hearing can be due to chronic otitis media. Why do young children tend to have ear infections? The Eustachian tube, a canal that runs from the middle ear to the back of the nose and throat, is shorter and more horizontal in young children than in older children and adults. This allows easier entry into the middle ear for the microorganisms that cause infection and lead to otitis media. The result is that children are at greater risk of acquiring ear infections than adults What microorganisms cause otitis media? Bacteria and viruses can cause otitis media. Bacteria such as Streptococcus pneumoniae (pneumococcus), nontypable Hemophilus influenzae and Moraxella account for about 85% of cases of acute otitis media. Viruses account for the remaining 15%. Affected infants under six weeks of age tend to have infections from a variety of different bacteria in the middle ear. What is the relationship between bottle-feeding and otitis media? Bottle-feeding is a risk factor for developing otitis media. The position of the breastfeeding child is better than that of the bottle-feeding position in terms of function of the Eustachian tube that leads into the middle ear. If a child needs to be bottle-fed, it is best to hold the infant rather than allow the child to lie down with the bottle. Ideally, the child should not take the bottle to bed. (In addition to increasing the chance for acute otitis media, falling asleep with milk in the mouth enhances the risk of tooth decay.) What are the risk factors for acute otitis media? Upper respiratory infections predispose to acute otitis media. Exposure to groups of children (as in child care centers) results in more frequent colds, and therefore more earaches. Exposure to air with irritants, such as tobacco smoke, also increases the chance of otitis media. Children with cleft palate or Down syndrome are prone to ear infections. Children who have episodes of acute otitis media before six months of age tend to have more ear infections later in childhood. What are the symptoms of acute otitis media? Young children with otitis media may be irritable, fussy, or have problems feeding or sleeping. Older children may complain about pain and fullness in the ear (earache). Fever may be present in a child of any age. These symptoms are often associated with signs of upper respiratory infection such as a runny or stuffy nose, or a cough The buildup of pus within the middle ear causes pain and dampens the vibrations of the eardrum (so there is usually temporary hearing loss during the infection). Severe ear infections may cause the eardrum to rupture. The pus then drains from the middle ear into the ear canal. The hole in the eardrum from the rupture usually heals with medical treatment. How is acute otitis media treated? The treatment for acute otitis media varies depending upon the age and symptoms of the child. The American Academy of Pediatrics (AAP) and the American Academy of Family Physicians (AAFP) recommend the following AAP and AAFP Recommendations Age Certain Diagnosis Uncertain Diagnosis <6 months Antibiotics 6 months-2years Antibiotics Antibiotics Antibiotics if severe illness; *Observation without antibiotics option if non-severe illness ≥2 years Antibiotics if severe illness; *Observation option if non-*Observation option without antibiotics severe illness *Observation is an appropriate option only when follow-up can be ensured and antibacterial agents can be started if symptoms persist or worsen. Non-severe illness is represented by mild ear pain and fever <39°C (102.2°F) in the past 24 hours. Severe illness is moderate to severe otalgia (ear pain) or fever 39°C. If antibiotics are initiated, Amoxicillin is usually recommended as the first line treatment. This is usually prescribed for 10 days. About 10% of children do not respond within the first 48-72 hours of treatment, and antibiotic therapy may have to be changed. Even after antibiotic treatment, 40% of children are left with some fluid in the middle ear which can cause temporary hearing loss lasting for up to 3 to 6 weeks. In most children, this fluid eventually disappears spontaneously (on its own). Children who have recurring bouts of otitis media may be referred to an otolaryngologist (ear nose and throat specialist or ENT). Some of these children may benefit from having an ear tube placed (tympanostomy tube) to permit fluid to drain from the middle ear. In addition, if a child has a bulging eardrum and is experiencing severe pain, a procedure to lance the eardrum (myringotomy) may be recommended to release the pus. The eardrum usually heals within a week What causes chronic otitis media? The Eustachian tube normally prevents the accumulation of fluid by allowing fluid to drain through the tube. Chronic otitis media develops over time, and often starts with a chronic middle ear effusion (fluid) that does not resolve. This persistent fluid will often become contaminated with bacteria, and the bacteria found in chronic otitis media are often different from those found in acute otitis media. Therefore, anything that disturbs the function of the Eustachian tube can lead to chronic otitis media What happens to the eardrum in chronic otitis media? The eardrum (tympanic membrane) has three delicate layers that help keep the eardrum thin, but strong. A chronic middle ear infection causes changes in the eardrum that weaken it, and often lead to a hole in the eardrum (tympanic membrane perforation). Eventually, the eardrum looses its strength and begins to collapse into the middle ear space. When the eardrum collapses, it can attach to the other middle ear structures. It is frequently seen draped around the middle ear bones (ossicles) or the inner wall of the middle ear (promontory). This disrupts the conduction of sound through the middle ear, and may diminish hearing How is chronic otitis media treated? Initially, antibiotics may resolve the infection. If a tympanic membrane perforation is also present, topical antibiotic drops may be used. If eardrum or ossicle scarring has occurred, that will not be reversed with antibiotics alone. Surgery is often indicated to repair the tympanic membrane (eardrum), remove the infected tissue and scar from the middle ear and the mastoid bone Otitis Media At A Glance Otitis media is the most common diagnosis in sick children in the U.S. Otitis media is an infection and inflammation of the middle ear. Otitis media causes fluid buildup in the middle ear. A cold or other respiratory infection can lead to otitis media. Exposure to other children's colds, as in daycare, raises the risk. Bottle-feeding increases the risk of otitis media in babies. Otitis media features fever, ear pain and fullness, as well as fussiness and feeding problems in young children. Middle ear pus causes pain and temporary hearing loss. Rupture of the eardrum allows the pus to drain into the ear canal Otitis media is treated with observation, antibiotics, or ear tubes.