About Academy of Health Professions
advertisement

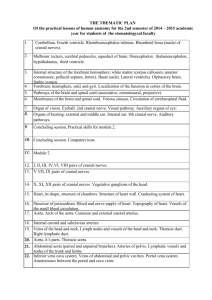
Maryland State Department of Education Academy of Health Professions Course 1: Foundations of Medicine and Health Science Unit 2: Medical Assessment Section 4: Nervous System WORKSHEETS UNIT 2: INTRODUCTION Many different fields of biology, chemistry, and physics converge in the application of medical diagnostics, where a combination of chemical tests, physical evaluations, and advanced imaging techniques are used to assess body functions, and detect possible abnormalities. Many of these techniques are used in routine preventative care, but are also an essential part of the tools used to identify injuries in emergency room situations. In this unit, you will investigate different methods of evaluating body function, as well as learning basic anatomy, and the structure and function of selected body systems. Contents 2.4 Nervous System 2.4.1 Cranial Nerve Function 2.4.2 Neurological Assessment 2.4.3 Sheep Brain Dissection © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 1 Academy of Health Professions Course 1: Foundations of Medicine and Health Science In an Instant© Part II After arriving at the hospital, many examinations and tests were performed on Jake, Rebecca, and also Marylou. With regard to Jake, the flight paramedic informed the trauma staff that Jake remained unconscious during the entire flight but maintained breathing and a pulse. At the accident scene he received IV fluids. He was transported with a C-collar and on a backboard to protect the spine from further injury. He was placed on supplemental oxygen (100%) while on the flight but did not need to be intubated. Jake regained consciousness shortly after arriving at the hospital but had no recollection of the event, or any idea about where he was or the date and time. Even though he was having difficulty speaking, he complained of a severe headache and excruciating pain in his leg and back. He also said he could not feel his arms, hands, and feet. Upon arrival to the trauma unit, many things were happening to Jake at once in order to accurately assess the extent of his injuries. After his clothing was removed, his vital signs were taken and he was evaluated for injury. At the same time blood was drawn for a type and screen, CBC, BMP, and a toxicology screen. Urine was collected for urinalysis. A head CT, chest x-ray, abdominal ultrasound, spinal MRI as well as Cspine, T-spine, L-spine films were taken. Finally a full body CT scan was conducted looking for other injuries for which he had no obvious symptoms. Attempts at finding a pulse in the broken leg failed repeatedly. Further testing for the vascular and neurological status of the leg was performed. Results from the testing determined that Jake had suffered a subdural hematoma from the traumatic impact of the accident and hitting the ground. He also had a broken right femur and fractures in the tibia and fibula of the same leg. The blood flow to the leg was compromised and the cause needed to be further evaluated to determine if surgery was necessary. In addition, the sensation in his hand, and feet were found to be caused by nerve damage resulting from a spinal cord injury and he was suffering from internal bleeding from a third degree splenic tear. Jake was started on corticosteroids immediately in order to prevent permanent paralysis. He was rushed into surgery in order to treat the subdural hematoma and to stop the bleeding from the splenic tear. Within 6 hours the vasculature in his leg would need to be repaired and blood flow restored in order to prevent amputation. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 2 Rebecca was examined and found not to have any physical injuries. Routine blood examinations were negative. Doctors and therapists determined she was suffering from acute stress disorder, which could develop into posttraumatic stress disorder if not treated effectively. She was released from the hospital. Over the next two weeks, she developed an extreme fear of vehicles and felt guilty for not getting Jake out of the intersection. She began reliving the accident through frequent nightmares and was unable to visit Jake in the hospital. She tried to avoid thinking about Jake and the accident as much as possible. Additionally, Rebecca suffered a loss of appetite and weight loss. The doctors recommended medications and therapy for Rebecca. Marylou Gonzalez was also taken to and observed at the hospital. Blood work revealed that two drugs in Marylou’s system caused a severe interaction, resulting in the symptoms she had suffered just prior to the accident. Other than that, Marylou was cleared by the hospital with a slight anxiety disorder. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 3 Academy of Health Professions Course 1: Foundations of Medicine and Health Science 2.4 NERVOUS SYSTEM The function of the nervous system is to sense, interpret and respond to changes in the external and internal environment to maintain a steady state within the body (homeostasis). The nervous system is divided into major structures: the central nervous system (CNS) which is comprised of the brain and the spinal cord, and the peripheral nervous system (PNS). On arrival at the scene of the accident, paramedics would have evaluated Jake’s vital signs such as heart rate (pulse), blood pressure, and respiration rate. Once this initial assessment had been conducted, a preliminary neurological assessment would have been conducted at the scene to determine the likelihood of any brain injury. When Jake arrived at the ER, a more comprehensive evaluation of his nervous system would have been conducted to identify the presence and extent of any damage. 2.4 Activity Learning Objectives: After completing this section student should be able to: Name the twelve cranial nerves. Describe the function of each of the twelve cranial nerves. Predict the effect of damage to any of the cranial nerves. Conduct basic neurological assessment procedures. Identify the presence of brain damage from neurological assessment responses. Correlate nervous system responses with nervous system function. Accurately record patient data using a medical chart. Analyze patient medical charts to interpret healthcare data. Conduct basic neurological assessment procedures Identify the presence of brain damage from neurological assessment responses. Accurately record patient data using a medical chart. Analyze patient medical charts to interpret healthcare data. Identify the major regions of the sheep brain. Correlate the structure of regions of the brain with their function. List several differences and similarities between the sheep and human. Use proper terminology to describe brain directions, planes, structures and surfaces 2.4 Activity Deliverables Upon completion of this section, each student will provide the following products to be included in a portfolio: 2.4.1 Cranial Nerve Function © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 4 o Worksheet 15: Cranial Nerves – to be inserted into the Course 1 Portfolio. 2.4.2 Neurological Assessment o Neurological Assessment Chart – to be inserted into the Course 1 Portfolio. 2.4.3 Sheep Brain Dissection o Worksheet 16: Sheep Brain Dissection – to be inserted into the Course 1 Portfolio. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 5 Academy of Health Professions Course 1: Foundations of Medicine and Health Science 2.4.1 Cranial Nerve Function 2.4.1 Activity Background There are twelve pairs of cranial nerves which are numbered I to XII starting with the most anterior. Each nerve responds to a different stimulus/stimuli, and damage to a particular nerve can be detected as a loss of that nerve’s function or response. 2.4.1 Activity Learning Objectives After completing this activity students will be able to: Name the twelve cranial nerves. Describe the function of each of the twelve cranial nerves. Predict the effect of damage to any of the cranial nerves. 2.4.1 Activity Deliverable Worksheet 15: Cranial Nerves: to be inserted into the Course 1 Portfolio. 2.4.1 Procedure 1. Using the internet, textbook, or another resource approved by your instructor, research the names, and functions of the twelve cranial nerves in humans. 2. Write your answers in Table 1 of Worksheet 15. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 6 Name:_____________________________ 2.4.1. WORKSHEET 15: CRANIAL NERVES Table 1. The Names and Function of the Twelve Cranial Nerves Cranial Nerve Cranial Nerve Name Function Number I II III IV V VI VII VIII IX X XI XII © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 7 Academy of Health Professions Course 1: Foundations of Medicine and Health Science 2.4.2 Neurological Assessment 2.4.2 Activity Background Neurological assessment is an essential tool in the evaluation of an acutely ill patient, and is used to quickly determine the level of function of the nervous system. It is used in all cases where there is the possibility of potential head injury, such as assessment of Jake following his accident. By identifying abnormal neurological responses, it is possible to detect the presence of nervous tissue damage. An assessment of neurological function would be conducted at different points in the care of a critically injured patient. Paramedics arriving at the accident scene after assessing the vital signs such as presence of a pulse, blood pressure, and respiration rate, would make an initial assessment which is known as the Glasgow Coma Scale. This assesses the level of consciousness of a patient which is an important predictor of traumatic brain injury. Consciousness is a state of awareness, and conscious patients are awake and responsive to their environment. A loss of complete or partial consciousness indicates a problem with brain function. The GCS evaluates two aspects of consciousness; arousal (wakefulness) where patients are tested to see if they are aware of their environment, and awareness, which tests their comprehension of what has been said. Patient’s arousal and wakefulness are evaluated by three behavioral responses: 1. Eye opening 2. Verbal response 3. Motor response Further neurological assessment would involve examining the responses of the pupils, the limbs, and individual tests of each cranial nerve. 2.4.2 Activity Learning Objectives After completing this activity students will be able to: Conduct basic neurological assessment procedures. Identify the presence of brain damage from neurological assessment responses. Correlate nervous system responses with nervous system function. Accurately record patient data using a medical chart. Analyze patient medical charts to interpret healthcare data. 2.4.2 Activity Deliverable Neurological Assessment Chart - to be inserted into the Course 1 Portfolio. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 8 2.4.2 Procedure Complete all of the assessments below on your partner and record the responses on the Neurological Assessment chart. 1. Glasgow Coma Scale: Eye Opening. Assessment of eye opening provides an indication of the patient’s state of wakefulness. Procedure (i) Without speaking or touching patient, check to see if their eyes are open. If their eyes are open, record a score of 4. (ii) If the patient’s eyes are closed, talk to them in a normal volume, and then speak louder if necessary. If they now open their eyes, record a score of 3. (iii)If the patient does not open their eyes, then you must test to see if they respond to a painful stimulus. In this exercise, you will administer a painful stimulus by gently pinching the skin on the forearm. CAUTION: Practice this procedure on yourself first to determine the minimum amount of pinching necessary. If the patient opens their eyes, record a score of 2. (iv) If the patient did not respond by opening their eyes to any of the above stimuli, record a score of 1. EYE RESPONSE SUMMARY Eyes open Eyes open to speech Eyes open in response to pain Eyes do not open to verbal or painful stimuli Patient unable to open eyes due to swelling, or a dressing SCORE 4 3 2 1 C 2. Glasgow Coma Scale: Verbal Response. An evaluation of verbal responses allows evaluation of awareness and appropriateness of speech. Procedure (i) Ask the patient his/her name, where he/she is, and current date and year. If answered correctly record score as 5. (ii) If the patient can hold a conversation but cannot answer the questions correctly, record a score of 4. (iii)If the patient is unable to hold a conversation, and is just saying single words or inappropriate words, record the score as 3. (iv) If the patient is groaning and not saying any recognizable sounds, record a score of 2. (iv) If the patient does not make any verbal response, record the score as 1. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 9 VERBAL RESPONSE SUMMARY Oriented Confused Inappropriate words Incomprehensible sounds No response SCORE 5 4 3 2 1 3. Glasgow Coma Scale: Motor Response. An assessment of motor response determines if the patient has the ability to respond by movement to verbal commands or painful stimuli. Procedure (i) Ask the patient to perform the following movements: 1. Stick the tongue out. 2. Squeeze your hand and let go. If the patient is able to do both properly, record a score of 6. (ii) If the patient does not respond to verbal commands, apply a painful stimulus by gently pinching the skin on the forearm. Observe any resulting movement and determine the appropriate score from the table below: MOTOR RESPONSE: MOVEMENT IN RESPONSE TO PAIN Obeys commands Purposely moves arm to the source of the pain Flexes or bends arm vaguely towards source of pain but does not locate it Flexes arms towards the body Extends and straightens arms No response SCORE 6 5 4 3 2 1 4. Calculating Glasgow Coma Scale Rating. After completing the above assessments, add up all of the points in all three sections to give you the Glasgow Coma Scale (GCS) rating for your patient. The maximum score is 15, and the minimum is 3. The GCS score gives the emergency room (ER) personnel an indication of the immediate care required by the patient. For example: Any ER patient with a score less than 15 must be examined immediately. A GCS score of 13-15 indicates mild head injury. A GCS score of 9-12 indicates moderate head injury. A GCS score of 8 or less indicates severe head injury. o Usually indicates a comatose state 5. Pupil Response. The pupils are the ‘black hole’ in the center of the iris of the eye which regulates the amount of light entering the eye. Assessment of the pupil’s size and response to light © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 10 can provide information on the presence of a head injury. Working in pairs, you will examine the pupil response of each other, and record the results on the neurological assessment chart. There will be no role play for this activity. Pupil Size and Shape Procedure (i) Observe the size and shape of both pupils (without the aid of a light). Record: a. Whether they are of equal size. b. The shape of each pupil. c. The size of the pupil using the chart below: Pupil Sizing chart Pupil Reactivity Procedure (i)Turn on a penlight. Holding it 6 inches from the face, bring the light from the right side of the face to shine in the center of the patient’s right eye. Observe the reaction of pupils of both eyes. Remove the light source and observe the response that follows. (ii) Repeat for the left eye. (ii) When the light is shone in one eye, both pupils should constrict. Record this as “equally reactive to light” in both the left and right columns. If the pupils do not react to light, record as non-reactive. 6. Limb Movement. Assessment of a patient’s ability to move their limbs can also give information regarding the presence of a head injury, or other neurological damage. Working in pairs, you will examine the limb movement of each other, and record the results on the neurological assessment chart. There will be no role play for this activity. Arms Procedure (i) Cross your middle and index finger and instruct the patient to grip and squeeze your middle and index fingers of both of your hands at the same time as hard as possible until asked to stop. The middle and index fingers are crossed to avoid a painful squeeze. The patient squeezes with both hands at the same time, as it is easier to make a comparison. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 11 (ii) Observe whether the grips are strong and of equal strength. (iii) Record strength of left and right hands as strong, or weak, and note if of equal strength. If patient is unable to respond to these commands, record “no response”. Legs Procedure (i) Ask the patient to lie down, if not already doing so. (ii) Place the palms of your hands against the bottom of the patient’s feet. (iii) Ask the patient to push with both feet at the same time hard against your hands. It is easier to make a comparison if the patient pushes with both legs at the same time. (iv) Record the strength of left and right legs as strong, or weak, and note if of equal strength. If patient is unable to respond to these commands, record “no response”. 7. Nerve Function. The function of individual cranial nerves can be tested by the following procedures to identify and localize any damage to the brain. Working in pairs, you will assess the function of the cranial nerves of each other, and record the results on the neurological assessment chart. There will be no role play for this activity. First Cranial Nerve Procedure (i) Ask the patient to close both eyes, and hold one nostril closed with their finger. (ii) Place the opened container of the test substance under their nose and ask the patient to identify the smell. (iii) Repeat with the other nostril. (iv) Record whether substance was correctly identified. Second Cranial Nerve Procedure (The 2nd cranial nerve is assessed by measuring visual acuity, that is, the ability to see. To do this, a standard visual exam is conducted). Procedure – far vision (i) Stand the patient to stand 20 feet from the eye chart mounted on the wall. (ii) Ask the patient to cover one eye with the eye occlude card, and to read all of the letters on the vision chart down to the 20/20 line. (iii) Record the lowest line that the patient is able to correctly read. (iii) Repeat for the other eye. Procedure – near vision (i) Have the patient hold the chart 14 to 16 inches from the eye at eye level, and cover one eye with the eye occlude. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 12 (ii) Ask the patient to read the letters from the chart. (iii) Record the lowest line that the patient is able to correctly read. (iv) Repeat for the other eye. Third, Fourth, and Sixth Cranial Nerves Procedure (The 3rd, 4th, and 6th cranial nerves can all be tested at the same time as they all regulate eye movement). (i) Hold one finger up about 6 inches from the patient’s face. (ii) Ask the patient to follow the movement of the finger with their eyes without moving their head. (iii) Slowly move your finger to the right and to the left. (iv) Observe whether the eye follows the finger and whether the movement is equal in both eyes. Fifth Cranial Nerve Procedure (The motor function and sensory function of the fifth cranial nerve can be tested by two separate procedures). Procedure – Motor Function (i) Ask the patient to bite down hard on his teeth. (ii) Gently assess the muscles of both sides of the jaw using your finger tips to determine if they are equally tight. (iii) Record whether the jaw muscles are equally tight on both sides or record any difference in size. Procedure – Sensory Function (i) Ask the patient to close their eyes. (ii) Gently touch the cotton ball to areas of the left side of the face. (iii) Ask the patient to say “yes” every time they feel something touch their face. (iv) Repeat for the right side of the face. (v) Record the number of correct responses for each side of the face. Seventh Cranial Nerve Procedure (i) Ask the patient to give a big smile. (ii) Observe whether the smile is equal and symmetrical on both sides. (iii) Record if equal on both sides or if any differences are present. Eighth Cranial Nerve Procedure (The 8th cranial nerve is tested by assessment of hearing). (i) Place the ticking clock 20 feet from the patient. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 13 (ii) Ask the patient to block the left ear with their finger. (iii) Record whether the patient can hear the ticking clock. (iv) Repeat for the right ear. (v) Record whether the patient could hear the ticking clock and whether there were any differences with each ear. Ninth and Tenth Cranial Nerve Procedure (The motor function of these nerves is tested using the gag reflex). (i) Ask the patient to open their mouth. (ii) Wearing gloves and using the tongue depressor, push down gently on the tongue and ask the patient to say “ahh”. (iii) Observe the uvula and soft palate. These should rise. (iv) Record if correct response is presence or absence. Eleventh Cranial Nerve Procedure (The 11th cranial nerve controls movement of the trapezius and sternocleidomastoid muscles. To assess function of this nerve, you will observe the ability of the patient to push against resistance using these muscles). Procedure – Sternocleidomastoid Muscles (i) Place your hand on the left side of the patient’s face. (ii) Ask the patient to move their head to the left while you apply gentle resistance with your hand. (iii) Observe the strength of the movement of the patient’s face, and also observe if the sternocleidomastoid muscle in the neck is prominent during this exercise (it should stand out). (iv) Repeat for the other side of the face. (v) Record muscle strength and any differences on each side. Procedure – Trapezius Muscles (i) Place your hands on the patient’s shoulders. (ii) Ask the patient to shrug their shoulders while you apply gentle resistance. (iii) Record muscle strength and if any differences are presence on either side. Twelfth Cranial Nerve Procedure (The 12th cranial nerve is assessed by observing movement of the tongue). (i) Ask the patient to stick out their tongue. (ii) Observe whether the tongue is extended in a symmetrical manner or if there are differences between the left and right sides. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 14 2.4.2 Glasgow Coma Scale - Student Role Play Cards Patient 1 Patient 2 You will open your eyes and look at You will have your eyes open and the person examining you. look at the person examining you. You will speak normally and You will speak normally, but you answer questions appropriately are confused. You don’t know where you are, and give the wrong You will be able to squeeze the month and year when asked. examiner’s hands and stick your tongue out. You will be slow to follow the verbal commands, but will be able to do what is asked. Patient 3 Patient 4 Your eyes will be closed even if You will keep your eyes closed, someone pinches you. even if someone pinches you. You will make no sound, even if You will groan in response to being someone pinches you. pinched, but will not say any recognizable words. You will not respond to verbal commands at all, even if pinched. You will not follow commands, but if someone pinches you, you will try to push his or her hand away. Patient 5 Patient 6 Your eyes will be closed, even if Your eyes will be open and you will someone calls you loudly. You will be looking around you with an open them if pinched. anxious expression on your face. You will say “Don’t!” or “Stop!” You will not answer questions at when pinched, but do not speak all. If pinched you will groan, but whole sentences and do not answer do not say any recognizable words. any questions. You will not follow commands, but if someone touches you (including You will not squeeze the examiner’s hands or stick out your to pinch you) you will grab hold of tongue, but you will quickly push his or her hand with both of yours. his or her hand away if pinched. Don’t let go easily. Patient 7 Patient 8 Your eyes will be closed, even if Your eyes will be closed, but you someone pinches you. will open them briefly if anyone calls loudly. You will make no sound, even if someone pinches you. You will not answer questions. If anyone pinches you, you will groan You will not follow commands. or yell, but not say any recognizable You will lie in a position where words. your closed fists are lying beside You will not follow commands, but one another at the top of your chest if someone pinches you, you will (decorticate posturing) and will not quickly push his or her hand away. move from this position. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 15 Patient 9 Your eyes will be closed, but you will open them if someone speaks to you. You will speak normally, but you are confused. You don’t remember exactly what happened to you, and you give the wrong month if asked. You will be slow to follow commands like, “show me two fingers,” but you will be able to do so. Patient 11 Your eyes will be closed, even if someone talks to you or pinches you. You will answer questions correctly. Mention that your head hurts. If anyone asks you to open your eyes, refuse and say "the light makes my head hurt really bad." Follow commands appropriately, but don't open your eyes Patient 13 Your eyes will be open. Your speech won’t make much sense. In answer to a question like, “what month is this?” you will say something like, “he, umm, he . . . My jacket. I don't . . . You will not follow commands, but if someone pinches you quickly push his or her hand away. © Patient 10 Your eyes will be closed, even if someone pinches you. The only sound you make will be a weak groan when someone pinches you. You will not follow commands, but if someone pinches you, you will try to pull away or turn away from the pain. Patient 12 Your eyes will be closed, but you will open them if anyone pinches you. Your speech will be fairly clear when you are aroused by a painful stimulus, such as a pinch, but you will only say, “leave me alone" or "what are you doing?" and soon go back to sleep. If someone asks you a question while you are still awake, you'll say, “I don’t know,” and go back to sleep. You will not follow commands, but if someone pinches you, you will quickly push his or her hand away. Patient 14 Your eyes will be closed, even if someone pinches you. You will not make any sound, even if someone pinches you. You will not follow commands. If someone pinches you, put your arms rigidly at your side (decerebrate posturing). Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 16 Patient 15 Patient 16 Your eyes will be closed, even if Your eyes will be closed at first, but someone pinches you. you will open them if someone calls you loudly.(3) You will keep repeating some meaningless phrase like, "I want my You will not say any recognizable bunny slippers, I want my bunny words. If someone asks you a slippers, I want . . ." Keep it up question, look confused and say, continually, and if someone pinches "mmm ? " without opening your you, just say it louder. mouth.(2) You will sit up and rock You will not follow commands. If continually. You will not follow someone pinches you, pull away.(4) commands. If someone pinches you, push or slap the hand away. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 17 Student Name:_____________________ Neurological Assessment Patient:_____________________ Date:____________ Time:__________ NEUROLOGICAL OBSERVATION CHART Limb Movement Pupil Response Best Verbal Response Best Motor Response GLASGOW COMA SCALE Eye Opening Spontaneously To Speech To Pain None Oriented Confused Inappropriate words Incomprehensible sounds None Obey commands Localize pain Flexion to pain Extension to pain None COMA SCALE RATING LEFT RIGHT Pupil Size and shape Pupil Reactivity Arms Legs 1st Cranial Nerve Function 2nd Cranial: Far vision Near vision 3rd, 4th, & 6thCranial 5th Cranial: Motor Sensory 7th Cranial 8th Cranial 9th & 10th Cranial 11th Cranial 12th Cranial © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 18 Academy of Health Professions Course 1: Foundations of Medicine and Health Science 2.4.3 Sheep Brain Dissection 2.4.3 Activity Background The brain is the largest structure of the nervous system and also one of the largest organs in the human body. It functions as the “command center” of the body as it receives, interprets, and responds to signals from all regions of the body, and coordinates the nervous system as a whole. For this reason, damage to regions of the brain can result in abnormal function in other parts of the body. Sheep brains are much smaller than human brains however they contain the same anatomical features as human brains. By dissecting a sheep brain students should get an appreciation for the structure of the human brain and be better able to relate this to its function. 2.4.3 Activity Learning Objectives After completing this activity students will be able to: Identify the major regions of the sheep brain. Correlate the structure of regions of the brain with their function. List several differences and similarities between the sheep and human. Use proper terminology to describe brain directions, planes, structures and surfaces. 2.4.3 Activity Deliverable Worksheet 16: Sheep Brain Dissection - to be inserted into the Course 1 Portfolio. 2.4.3 Procedure 1. Complete Worksheet 16: Sheep Brain Dissection. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 19 Student’s Name: _______________________ 2.4.3 WORKSHEET 16: SHEEP BRAIN DISSECTION (www.brainu.org) I. Characteristics of a brain Write down 5 physical characteristics of your sheep brain? (e.g. how the brain feels, color of the brain, etc) I. II. III. IV. V. ________ _ . ____ . _______ . _______ ___________ . . II. Identifying brain regions Body directions to use when talking about the brain: Caudal, dorsal, lateral, medial, rostral, and ventral. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 20 a. Draw the LATERAL (outer side) view of your sheep brain (include the cerebellum and brainstem). Label the different lobes. You can peel the covering halfway back. b. Looking at your drawing, find the different lobes of the brain on your sheep brain. List the functions of each lobe. 1. Frontal Lobe 2. Parietal Lobe 3. Temporal Lobe 4. Occipital Lobe © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 21 c. Draw the MEDIAL (inner side) view of the sheep brain. Label all of the brain parts that you can see. d. Look at your sheep brain and find out whether you have the right or left half (hemisphere). I have the _______________________ half (hemisphere). Find another group with the opposite half as yours and put both halves together. Compare the size of the brain to the size of a known object e.g. the whole sheep brain is as small as an apple. Write your comparison below. _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ III. Coverings of the brain The dura mater (tough mother) is a protective covering of the brain. Does your sheep brain have a dura mater? (Hint: it looks white or purplish) a. To take the dura mater off, locate the ROSTRAL end of your sheep brain. b. Using your thumb and index finger, peel the dura mater back towards the CAUDAL side. You might have to use the scissors to snip part of the dura mater at the ROSTRAL end. c. Remove the dura mater. d. Try pulling the dura mater apart. What do you notice? Does it rip like a piece of paper? Describe the properties of the dura mater. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 22 IV. First dissection – Exploring the Neuron and its parts a. Find the structure of a neuron from your textbook. Draw a neuron and label its parts. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 23 b. Place your brain with the cut-side (MEDIAL) down. c. Using your plastic knife, cut the brain about 1 inch from the rostral end (where the dent is located). d. Draw the inside of the cutoff piece. Label white and grey matter, and describe what it contains. e. What do you notice about the cut surface? f. Using the probe stick, poke the dark area? How does it feel? g. Using the probe stick, poke the light area? How does it feel? h. Identify the dark and light areas. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 24 V. Second dissection: Memory function of the brain What is the part of the brain that stores short term memories? a. To find this brain part, slide your thumb along the outside (lateral side) of the brain stem until it disappears under the cerebrum. b. Keep wiggling your thumb and dig it gently under the cortex until you can’t push it in any more. c. Pull back the cerebrum so that you break the brain into two pieces. The memory center is the white C-shaped band of fibers and the grey matter inside them right around the area where the brain broke apart. d. Try to pull it out. i. What do you notice about it? ii. What kinds of things does a sheep need to remember? © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 25 VI. Comparing Sheep Brains to Human Brains a. Label the brain parts in both the human and sheep brain picture. MEDIAL view of the human brain CAUDAL MEDIAL view of the sheep brain CAUDAL The outer layer of the brain is called the cerebral cortex is the thin layers of worm-like gray matter forming the surface of the hemisphere. The cortex is arranged in folds called gyri (singular = gyrus) which are separated from one another by folds called sulci (singular = sulcus). b. Observe the cortex in the sheep and the human brain. What do you notice about their relative size? © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 26 c. What is the role of this region of the brain? d. Why does it differ between human and sheep? © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 27 2.4.3 GLOSSARY Anterior – towards the head. Brainstem – the major route by which the forebrain sends information to and receives information from the spinal cord and peripheral nerves. It controls respiration and regulation of heart rhythms. Caudal or Posterior – towards the tail. Cerebellum – a structure located above or dorsal to the brainstem that helps control movement, balance and muscle coordination. Cerebral hemispheres – the two halves of the cerebrum. The left hemisphere is specialized for speech, writing, language, and calculations. The right hemisphere is specialized for spatial abilities, face recognition in vision, and some aspects of music perception and production. Cerebrum or Cerebral Cortex – Brain tissue seen from the side, top, front, and back that appears as tightly packed fat ridges and narrow folds. The outer cerebrum is responsible for all forms of conscious experience, including perception, emotion, thought, and planning. Cortex means bark in Greek. The bark of the cork tree looks a lot like the cerebral cortex of the brain. Corpus callosum – a large bundle of nerve fibers (myelinated axons) that link the right and left hemispheres of the brain. Dorsal – towards the back. Dura mater – Tough, leathery outermost layer of the membranes surrounding and protecting the brain. The dura mater lines the inside of the skull and drapes loosely around the spinal cord. Dura mater is Latin for ‘tough mother.’ Frontal lobe – front region of the cerebrum concerned with cognitive processes that include planning, inhibition of instincts and drives, and declarative memory. Gyrus (pl. = gyri) - the ridges or bumps of folded cortex Hippocampus – C-shape band of fibers located within the brain responsible for formation of declarative memory, transfer of short-term to long-term memories and has nerve fiber connection to the amygdala for emotional processing. Lateral – towards the outside. Medial – towards the middle. Meninges – three membranes (the dura mater and two other thin membranes) that cover and protect the brain and spinal cord against shocks, knocks, and vibrations. Blood vessels run through the thin membranes before entering the brain. Myelin – compact fatty material that surrounds axons of many neurons. Myelin acts as an insulator to speed action potential movement down axons. Occipital lobe –located in the caudal region of the cerebrum, receives sensory information from the eyes. Olfactory bulb – anterior part of the brain concerned with the sense of smell. Parietal lobe –located around the dorsal and medial region of the cerebrum that processes higher sensory and language functions. Pituitary gland – gland at the base of the brain that makes and releases growth, reproductive, and other hormones into the blood stream. Rostral or Anterior – towards the front or nose. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 28 Spinal Cord – bundle of nerve fibers, located inside the backbone, that connects the brain to different sensory and motor parts of the body. Sulcus (pl. = sulci) – the valleys or spaces between the folds or gyri of the brain. Temporal lobe – located near the temples and ear region of the cerebrum concerned with smell, taste, hearing, visual associations, some aspects of memory, and a person’s sense of self. Ventral – towards the stomach. Ventricles – fluid-filled cavities inside the brain. © Copyright, Stevenson University, 2009; AHP Course 1_Unit 2: Section 4_Teacher Version 2 Page 29