Shoulder Arthritis: Causes and Treatment
advertisement

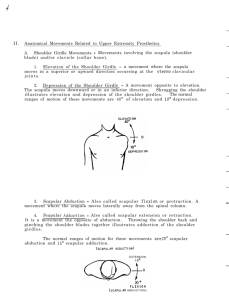
Shoulder Arthritis: Causes and Treatment 1. Pathophysiology of the Region: Arthritis of the glenohumeral (shoulder) joint can stem from a variety of factors. In the case of glenohumeral (GH) osteoarthritis, pain and loss of active range of motion is caused by a decrease in the articular hyaline cartilage of the corresponding joint surfaces. In the case of shoulder osteoarthritis, the articular cartilage of the head of the humerus corresponds to the surface of the glenoid fossa, formed by the anterior surface of the scapula and inferior surface of the clavicle. Osteoarthritis of the glenohumeral joint arises from factors such as: increasing age, trauma, surgical trauma, immobilization, muscle weakness, postural abnormalities, overuse, etc. In the case of postural abnormality, the patient typically presents to Physical Therapy with a forward head, rounded shoulders appearance. This presentation is indicative of "upper cross syndrome" in the upper quarter. "Upper cross syndrome" is a Physical Therapy-specific diagnosis caused by weak deep cervical flexor musculature, tight cervical extensor musculature, weak lower scapula retractors, and tight pectorals. The position of the scapula plays a major role in the patient's complaint of pain and lack of range of motion. With this presentation, the patient's humerus is internally rotated while the scapula is protracted and anteriorly tilted. Positioning of the scapula in this manner causes an "impingement" of the rotator cuff muscles and subsequent pain and lack of active range of motion. Lack of active range of motion cascades into arthritic changes of the glenohumeral joint. Correction of this dysfunction typically leads to decreased pain levels and improved bilateral shoulder active range of motion (AROM). A common misconception among Physical Therapy patients is that immobilization and "rest" will heal glenohumeral arthritis. However, osteoarthritis responds best to mobilization and therapeutic exercise; especially when combined with Acupuncture and traditional medical treatments. Mobilization of an arthritic synovial joint will improve the quality of the remaining hyaline cartilage and increase the amount of circulating synovial (lubricating) fluid within the joint itself. Research-Based Contribution: A Study on the Clinical Effects of Physical Therapy and Acupuncture to Treat Spontaneous Frozen Shoulder A quasi-experimental study performed in 2006 by Tsochiang Ma and colleagues explored the relationship between acupuncture treatment and Physical Therapy for adhesive capsulitis of the glenohumeral joint. The study divided a group of 75 patients into three groups: 1) A control group consisting of only acupuncture treatment 2) An experimental group consisting of only Physical Therapy treatment 3) A combination of the two treatments. In summary, treatment of adhesive capsulitis as related to pain level and functional mobility was most effective in experimental group III (combination group). subjective pain levels improved with acupuncture alone quickly; however, restoration of function in the shoulder joint was not seen until multiple weeks following the onset of treatment. The study suggests that although acupuncture and Physical Therapy can be used independently to treat pain and loss of function (ROM and strength loss), a combination of the two is most effective in this clinical scenario. Special Tests for the Glenohumeral Joint: - Neer Impingement Test - Hawkins Kennedy - Biceps Load I,II - Yergunson's Test - Load and Shift - Shoulder Apprehension - Obrien's Test - Functional Testing (ADL)