fall management program - Communities of Practice
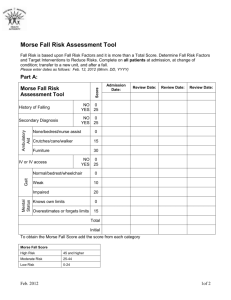
advertisement

NOR-MAN Regional Health Authority Acute Care Fall Prevention and Management Program February 8, 2012 Table of Contents Introduction __________________________________________________________________ 4 Goals: _______________________________________________________________________ 4 Objectives: ________________________________________________________________________5 Expected Outcomes _________________________________________________________________6 Definitions: ________________________________________________________________________6 Determining the Risk Of Falling __________________________________________________ 7 Risk Factors _______________________________________________________________________7 Documentation ________________________________________________________________ 7 Staff Education _______________________________________________________________ 8 Indicator Tools for Measuring the Incidence of Falls _________________________________ 8 FalI Rate__________________________________________________________________________8 Injury Rate________________________________________________________________________8 Risk Rate _________________________________________________________________________8 Evaluating the Effectiveness of the Fall Prevention and Management Program ___________ 9 REFERENCES _______________________________________________________________ 9 Fall Prevention and Management Self Learning Package ____________________________ 11 Overview ________________________________________________________________________11 Objectives ________________________________________________________________________11 What is a fall? ____________________________________________________________________11 Facts about Falls __________________________________________________________________11 Best Practice Recommendations _________________________________________________ 11 Assessment _______________________________________________________________________11 Interventions/Careplan _____________________________________________________________12 Education Recommendations ___________________________________________________ 12 Nursing Education ________________________________________________________________12 Organization & Policy Recommendations Least Restraint ____________________________ 12 Organizational Support ____________________________________________________________13 Fall Prevention and Management: ______________________________________________ 13 Goals of Fall Prevention AND MANAGEMENT Program ____________________________ 13 10676232412 DRAFT Page 2 of 16 Components of a Fall Prevention and Management Program ________________________ 13 Step 1 - Search for Causes __________________________________________________________ 14 Patient Risk Factors_______________________________________________________________ 14 Step 2 – Use Triggers to Implement the Fall Prevention and Management Program and Identify Patients at Risk for Fall ____________________________________________________________ 14 Step 3 – Implement the Program ____________________________________________________ 14 Step 4 – Assess and Reassess the Patient ______________________________________________ 15 Step 5 – Report Falls ______________________________________________________________ 15 Fall Prevention and Management Program: Test __________________________________ 16 10676232412 DRAFT Page 3 of 16 INTRODUCTION Falls can be serious and disabling. Hip fractures are the most fall related injury resulting in hospitalization. 90% of hip fractures are due to a fall and 20% of those die within a year. The presence of osteoporosis is the main reason given for the high incidence of hip fractures in older women. Women are three times more likely than men to be hospitalized for a fall related injury. There continues to be a debate as to whether the hip fracture precedes the fall or is a consequence of the fall. Falls are both common and serious events in the lives of older people. Falls are the 6th leading cause of death among older adults. Falls are the leading cause for injury admissions to acute care. One half of the falls among seniors result in a minor injury and 5% to 25% result in serious injury. Falls are likely to be the result of normal aging changes such as a decline in vision, postural balance, and environmental factors such as low lighting, shiny floors, furniture in the way, etc. In certain individuals, changes in the sensory, neurologic, muscular skeletal and cardiovascular systems may put these individuals at a greater risk for falling. The most important aspect of fall prevention and management is to predict the fall before it occurs. Analyzing and recording the events surrounding the fall is critical to preventing a similar reoccurrence. A "Fall Prevention and Management Program" is a preventative strategy that employs interventions to prevent falls. Even without injury, a fall can cause a loss in confidence and curtailment of activities. It must be noted that despite fall prevention and management efforts some falls will still occur. Therefore, it is imperative that an assessment of the circumstances surrounding the fall be carried out following each fall. In the management and treatment of falls as much information as possible surrounding the fall is needed. It is important to identify who is at risk; understand why the fall occurred; know when, where and how it occurred; know if the patient was on the program when they fell; document if there were any injuries; document the new interventions initiated to prevent a reoccurrence; and evaluate the outcome(s) of the intervention(s). GOALS: To identify the patients at risk for falling and initiate appropriate interventions. To reduce the number and severity of falls. To provide an interdisciplinary approach to the prevention and management of falls To educate and involve participation of patient, family and staff in the Fall Prevention and Management Program. 10676232412 DRAFT Page 4 of 16 Objectives: 1. Where possible, predict the fall before it occurs. Process: Complete MORSE Fall Risk Assessment Tool on every patient on admission, at change of condition; transfer to a new unit and after a fall. Add admission date or review date as appropriate. Score the number in the appropriate column. Based on the score identify the patient at low, moderate or high risk. For patients at low risk of falling, provide Good Basic Nursing Care. Bed on lowest setting except when care is being done. Ensure necessary items are within reach; Examples: call bell, over the bed table with personal items, water and/or urinal. Assess environmental area Encourage regular toileting Encourage regular exercises. If the patient scores moderate to high risk, implement the Fall Prevention and Management Program. Initiate all Level 1 interventions for all patients that qualify for the program. Initiate Level 2 interventions as appropriate for both moderate and high risk patients. On review of Morse Fall Risk Assessment Tool, if the patient no longer qualifies as moderate to high risk, then resolve the Interventions/Careplan, discontinue the Fall Prevention and Management Program and provide good basic nursing care. If the patient does not qualify for the Fall Prevention and Management Program and the nurse feels the patient is at risk, then implement the program and explain why. 2. Examine and record the circumstances surrounding the fall so that steps can be implemented to prevent a similar reoccurrence. Process: Document all falls on occurrence report (Policy # I-D-300) and in the nurse’s notes. Original occurrence report goes to Unit Manager. Do not photocopy. Do not chart in the nurse’s note that occurrence report was done. Document the fall only. Complete Acute Care Time of Fall Patient Evaluation (R-GEN-326). Be very specific and descriptive when charting the type of injury. e.g.: abrasions, swelling, etc. Photocopy and attach to occurrence report, original to stay on chart. Complete Acute Care Environmental Assessment Audit form IF applicable (R-GEN-328). Photocopy and attach to occurrence report, original to stay on chart. After a fall or with any review of the Morse Fall Scale, patient nurse and health care aide to review the patient care area and initiate additional interventions as appropriate. Interventions/Care Plan to be reviewed and updated, new plan of care to be communicated to all staff and added to team sheet. 10676232412 DRAFT Page 5 of 16 3. Develop an educational program to increase staff awareness of the "Fall Prevention and Management Program". Process: In-services will be held to educate all staff on any change to Fall Prevention and Management Program. Patient Safety Coordinator to cover Fall Prevention and Management Program during general orientation. Fall Prevention and Management Program will be reviewed during ward orientation. Staff will have the opportunity to implement the program and follow through the entire process, then have the opportunity to ask questions. Staff to read Fall Prevention and Management Program annually, (June) and do test. Staff will educate patient/family at time of admission and on a regular basis with safety precautions/interventions. 4. Monitor falls and any injuries resulting from falls and evaluate the effectiveness of the Fall Prevention and Management Program. Process: Patient Safety Coordinator to collect and enter data monthly using the Fall Rate. Patient Safety Coordinator to determine if the number of falls and severity of falls has been reduced. Coordinator will provide data to Unit Managers on request. Staff will be informed of the data at staff meeting and in writing by memos. 5. Evaluate the effectiveness of the "Fall Prevention and Management Program". Process: Plan for sustained improvement in reducing the number of falls and severity of falls. Use monthly data to monitor falls and facilitate sustained improvement Demonstrate an ongoing improvement of baseline data/2011 and sustain the improvement. If improvements not sustained then reevaluate the Fall Prevention and Management Program. Expected Outcomes To promote an environment that encourages independence, confidence, activity, and mobility, as well as promoting safety To reduce the number and severity of falls. To educate patients, families, and staff on Fall Prevention and Management Program. To provide an interdisciplinary approach to the prevention and management of falls. Definitions: Fall: Unintentionally coming to rest on the ground, floor or other lower level with or without injury No Injury: There is no evidence of abrasion(s) or bruising and no complaint of pain following the fall. Minor Injury: Any small bruise or abrasion that does not require medical treatment and will heal within several days. Moderate Injury: Injury requiring medical treatment that is not considered major. Bruises, contusions, and sprains are considered moderate if they require treatment. Suspected bone injury is considered moderate if an x-ray is ordered and there is no evidence of a fracture. A small cut that requires only a few sutures is considered moderate. Major Injury: A serious injury, including any fracture, head injury, or wound that requires major suturing. 10676232412 DRAFT Page 6 of 16 DETERMINING THE RISK OF FALLING Identifying patients at risk for falling is difficult because falls are typically the result of the interaction of more than one factor. In an attempt to identify those patients at risk for falling, a Morse Fall Risk Assessment Tool is required on admission, at change of condition; transfer to a new unit, and after a fall. Risk Factors The following shall be taken into consideration in identifying risk factors: History of falls Altered mental state (confusion, disorientation, uncontrolled restlessness, sedation) Ambulatory aid Limited mobility or abnormal gait Severely limited vision or hearing Restraint use History of crawling out of bed Unwillingness or inability to call for help while walking A recent history of dizziness or syncope IV access with tubing Lack of footwear Incontinence Age of 75+ Five or more medications Secondary diagnosis Unmet needs (hunger, thirst, need to go to bathroom) Environmental causes Unfamiliar environment DOCUMENTATION Reporting and documenting all falls with or without injury is important. If a patient falls once, the risk of falling again is increased. The most important aspect of prevention is to predict a fall before it occurs, to report the circumstances surrounding the fall, then implement interventions to try to prevent the fall. Ensuring that the interventions are communicated to all members of the Health Care Team is an essential component to preventing and managing falls. When documenting the implementation of the Fall Prevention and Management Program, ensure that: 1. Morse Fall Risk Assessment Tool is done on Admission, with change of condition; transfer to a new unit and after a fall. 2. Fall Prevention and Management Interventions/Careplan with Level 1 & 2 interventions has been individualized and initiated. 3. All vital information is documented on the Nursing/Physician Order Flow Sheet (NN) and team sheet. 4. Accurate shift to shift reporting occurs. 5. Accurate nurse to healthcare aide report with up to date interventions. 10676232412 DRAFT Page 7 of 16 STAFF EDUCATION Educating all staff in the importance of a Fall Prevention and Management Program is vital to the success in reducing falls and severity of falls. The following methods will be utilized to ensure the Fall Prevention and Management Program is communicated to all disciplines: The Fall Prevention and Management Program will be included in General Orientation and Ward/Department Orientation. All staff will be expected to review the Fall Prevention and Management Program by reading the program and doing the test annually (June). Patient/Family will sign adult database acknowledging teaching was done on admission. INDICATOR TOOLS FOR MEASURING THE INCIDENCE OF FALLS Fall Rate The “Fall Rate” is the most reliable method of measuring the incidence of falls because it includes every fall in the calculation, not just the number of patients who have fallen. Although a patient who falls repeatedly may artificially inflate the statistics, it is an accurate reflection of the number of times a patient is actually at risk of injury. The "Fall Rate" is calculated on the number of patient bed days, rather than the number of patients at risk, which does not consider the length of stay. This is used as a standard measure. The Fall Rate is calculated by: Number of patient falls X 1000 Number of patient bed days Injury Rate An injury rate provides an important indicator monitoring facility falls. Only one injury per patient is included - if two injuries occur in one fall that is counted as only one injury. It may be helpful to calculate the rate of minor, moderate, and major injuries separately. The Injury Rate is calculated by: Number of patients Injured X 100 per time period (i.e. per month) Number of patients who fell Other statistics, such as the "Number of patients at risk", the "Number of repeated falls" and the "Number of patients injured", should be reported so that all necessary calculations and comparisons can be made. Risk Rate All patients are at risk of falling. The number of patients at risk equals the number of patients admitted during the study period. "At Risk" does not refer to risk factors contributing to a fall. This method includes the multiple, or repeated falls of any patient in the numerator. Number of patient falls X 100% Number of patients at risk 10676232412 DRAFT Page 8 of 16 EVALUATING THE EFFECTIVENESS OF THE FALL PREVENTION AND MANAGEMENT PROGRAM Evaluating the Fall Prevention and Management Program is important for several reasons: 1. It enables the identification of the pattern of falls and the implementation of additional intervention if appropriate. 2. It provides positive feedback to frontline staff and the facility that the program is indeed assisting in reducing falls which in turn encourages more staff buy-in to the program. 3. It enables the facility to provide an increased quality of life for patients through the assessment and evaluation of intervention strategies. 4. It also allows the identification of the cost savings to the health care system (cost in human suffering, and subsequent decrease in the quality of life), that result from a Fall Prevention and Management Program. The overall effectiveness of the program will be seen in the general reduction in patient falls and decrease in the severity of falls. Monthly calculations of the Fall Rate and making these stats available to all staff serve as a reminder to all the importance of the Fall Prevention and Management Program. In Conclusion: If a patient falls, it is a failed strategy, not a staff fault. It is important to analyze why the patient fell and to implement a different intervention as appropriate. REFERENCES Bayne1 C. Grisham. Falling: Why and What to Do About It. Nursing Management, May 1999 Fall Prevention. Making It Work. Associated Health Systems, Inc. Edmonton, Alberta Managing Falls: Identifying Population Specific Risk Factors and Prevention Strategies. Ignatavicius Donna. Do you help staff rise to the fall-prevention challenge? Nursing Management, January 2000. Jewell, Laura. Falls Intervening Clinic - Aging, Health and Society. Morse, Janice M. Preventing Patient Falls Sage Publications, California, 1997 Morton Dolores. Five Years of Fewer Falls. American Journal of Nursing. Sullivan, Ruth P and Bad ros, Karen K. Recognize Risk Factors to Prevent Patient Falls - Nursing Management. May 1999 Canadian Fall Prevention Curriculum (CFPC) January 2009 Nursing Care Plans 6th Edition, Gulanick/Myers 10676232412 DRAFT Page 9 of 16 NOR-MAN Regional Health Authority Acute Care Fall Prevention and Management Self Learning Package February 8, 2012 10676232412 DRAFT Page 10 of 16 FALL PREVENTION AND MANAGEMENT SELF LEARNING PACKAGE Overview The purpose of this self-learning package is to enhance the understanding and knowledge of health care providers regarding best practice for patient fall prevention and management. Objectives Upon completion of this module, the learner will be able to: Recognize the risk factors associated with patient falls. Discuss the incidence and morbidity of falls occurring in hospitals. Inspect patient care areas to identify and remove extrinsic hazards that may lead to patient falls. Define the components of a comprehensive Fall Prevention and Management Program. Evaluate the need for patient supports; grab bars, and other fall prevention devices to provide a safe patient environment. Complete Fall Prevention and Management test annually with 90% or greater What is a fall? A fall is unintentionally coming to rest on the ground, floor or other lower level with or without injury. Facts about Falls In Canada, falls are the 6th leading cause of death among older adults. Falls are the leading cause for injury admissions to Acute Care. Hospitals It is estimated that of the 1 in 40 who are hospitalized as a result of a fall, only 50% will be alive one year later. Falls account for up to 84% of inpatient incidents. Fall injuries pose a significant burden in terms of loss of life, reduced quality of life and economic cost. Most falls occur between the hours of 0630-1600H – during peak activity times. Most falls occur from or near the patient’s bed while trying to transfer from one location to another (e.g. the bathroom). BEST PRACTICE RECOMMENDATIONS Assessment Assess fall risk on admission. Assess fall risk after a fall. Assess fall risk when significant change in condition and with transfer to a new unit 10676232412 DRAFT Page 11 of 16 Interventions/Careplan Exercise Regular exercise is encouraged for all patients. Patients qualifying for moderate or high risk of falls are assessed by physiotherapy. The physiotherapist makes specific recommendations for individual patient exercise/activity. Interdisciplinary Team The multidisciplinary team implements multi-factorial interventions to prevent and/or minimize falls. Medications Doctors, nurses and pharmacist conduct periodic medication reviews in an attempt to decrease falls. Patients taking antihypertensive, diuretics, laxatives, narcotic analgesics, psychotropic’s or more than five medications have been identified at risk for falls. Vitamin D The team provides patients with information on the benefits of vitamin D supplement in relation to reducing fall risk. In addition, information on dietary, life style, and treatment choice for the prevention of osteoporosis is relevant in relation to reducing the risk of fracture. Patient/Family Education The patient/family will be educated on admission in regards to the level of risk and the interventions in place to attempt to prevent or minimize a fall. The patient/family will receive updated information as the plan of care changes. Environment The team includes environmental modifications as a component of the Fall Prevention and Management Program. EDUCATION RECOMMENDATIONS Nursing Education Education on The Fall Prevention and Management Program should be included in nursing curricula and on-going education with specific attention to: Promoting safe mobility Risk assessment Multidisciplinary strategies Risk management including post-fall follow-up Alternatives to restraints and/or other restricted devices ORGANIZATION & POLICY RECOMMENDATIONS LEAST RESTRAINT Nurses should not use side rails for the management of falls or recurrent falls for patients receiving care in an acute care facility; however, other client factors may influence decision-making around the use of side rails. Organizations establish a corporate policy for least restraint that includes components of physical and chemical restraints. See Acute Care Restraint Policy VII - F - 10 10676232412 DRAFT Page 12 of 16 Organizational Support Organizations create an environment that supports interventions for fall prevention and management that includes: Fall Prevention and Management Program Patient, family and staff education Multidisciplinary team approach for risk assessment and interventions/careplan. Availability of supplies and equipment such as transfer devices, high/low beds, and bed alarms. FALL PREVENTION AND MANAGEMENT: Building the Foundation for Patient Safety. A Self Learning Package and Test GOALS OF FALL PREVENTION AND MANAGEMENT PROGRAM 1. To create a safe environment that encourages independence, confidence, activity and mobility. 2. To identify the patients at risk for falling and initiate appropriate interventions. 3. To reduce the number and severity of falls. 4. To educate and involve participation of patients, families and staff in the program. COMPONENTS OF A FALL PREVENTION AND MANAGEMENT PROGRAM 1. Universal Fall Prevention and Management Program. 2. Admission assessment of all patients using the Morse Fall Risk Assessment tool to identify level of risk. 3. Risk Assessment Scores and level of risk recorded into the kardex. 4. If the patient is at low risk of falling, provide good basic nursing care. 5. If the patient is at moderate or high risk of falling, implement The Fall Prevention and Management Program. Initiate all Level 1 interventions for all patients that qualify for the program. Initiate Level 2 interventions as appropriate for both moderate and high risk patients. 6. Morse Fall Risk Assessment tool is to be redone if the patient falls, has a change in condition or is transferred to a new unit. All falls must be documented in the patient chart and on an occurrence report (Policy # I – D – 300). Complete the Acute Care Time of Fall Patient Evaluation (R – Gen – 326) and complete an Acute Care Environmental Audit if appropriate (R – Gen – 328) 7. Monitor falls and any injuries resulting from a fall. 8. Evaluate the effectiveness of the Fall Prevention and Management Program 10676232412 DRAFT Page 13 of 16 Step 1 - Search for Causes There are many causes of falls and some of them can be eliminated. Look for patterns or similarities in the falls in your workplace. Be sure to investigate. Patient Risk Factors History of falls Altered mental state (confusion, disorientation, uncontrolled restlessness, sedation) Ambulatory aid Limited mobility or abnormal gait Severely limited vision or hearing Restraint use History of crawling out of bed Unwillingness or inability to call for help while walking A recent history of dizziness or syncope IV access with tubing Lack of footwear Incontinence Age of 75+ Unfamiliar environment Five or more medications (antihypertensive, diuretics, psychotropic, etc.) Secondary Diagnosis Unmet needs ( hungry, thirst, need to go to the bathroom) Environmental causes Step 2 – Use Triggers to Implement the Fall Prevention and Management Program and Identify Patients at Risk for Fall Morse Fall Risk Assessment tool will identify patients that qualify for the Fall Prevention and Management Program. Documentation should reflect risk assessment, risk factors, interventions/care plan and the patient/family teaching. Step 3 – Implement the Program 1. If the patient is identified at low risk, provide good basic nursing care. 2. If a patient is identified as moderate or high risk for falling, implement the Fall Prevention and Management Program. Initiate all Level 1 intervention for all patients that qualify for the program. Initiate Level 2 interventions as appropriate for both moderate and high risk. 3. If a patient does not qualify for the Fall Prevention and Management Program and the nurse feels the patient is at risk, then implement the program and explain why. 4. For interventions see Fall Prevention and Management Interventions/Careplan on back of Morse Fall Risk Assessment tool. 10676232412 DRAFT Page 14 of 16 Step 4 – Assess and Reassess the Patient Step 5 – Report Falls Report falls with or without injury – use the occurrence report form (Policy # I – D – 300) Assess severity of injury/injuries resulting from the fall. No Injury: There is no evidence of abrasion(s) or bruising and no complaint of pain following the fall. Minor Injury: Any small bruise or abrasion that does not require medical treatment and will heal within several days. Moderate Injury: Injury requiring medical treatment that is not considered major. Bruises, contusions, and sprains are considered moderate if they require treatment. Suspected bone injury is considered moderate if an x-ray is ordered and there is no evidence of a fracture. A small cut that requires only a few sutures is considered moderate. Major Injury: A serious injury, including any fracture, head injury, or wound that requires major suturing. Reporting and documenting all falls is important. If a patient falls once, the risk of falling again is increased. The most important aspect of prevention is to predict a fall before it occurs, to report the circumstances surrounding the fall, then implement interventions to try to prevent a fall. Ensuring that the interventions are communicated to all members of the Health Care Team is an essential component to preventing and managing falls. When documenting the implementation of the Fall Prevention and Management Program, ensure that: All vital information is documented on the Nursing/Physician Order Flow Sheet (NN). Interventions/Care plan Level 1 and Level 2 interventions have been initiated as appropriate, and reviewed as necessary with new interventions initiated. If appropriate The Interventions/Careplan will be kept in Kardex to ensure all staff have access to pertinent information Accurate shift to shift reporting occurs. Nurse to health care aid reporting is essential. 10676232412 DRAFT Page 15 of 16 FALL PREVENTION AND MANAGEMENT PROGRAM: TEST True or False 1. Falls are the leading cause of death in the elderly. T F 2. Falls in acute care settings account for 50% of all inpatient incidents. T 3. Risk assessments should be performed on all admissions to hospitals. F T F 4. Anytime there is a change in the patient’s treatment, medication or condition, the fall assessment should be updated. T F 5. Laxative use can increase fall risk. T F 6. Relocating a patient to a new room may increase their risk for falling. T F 7. Whenever possible, reduce or change medications to ones not associated with sedation, disorientation or hypotension. T F 8. With a well established fall management plan, it is not necessary to include the patient or the family and friends in fall management efforts. T F 9. Electronic monitors which activate call lights and/or an audible alarm when the patient exits the bed, are effective as fall tools, and may help reduce restraint use. T F 10. Restraint use is an effective fall management strategy. T F 11. A successful fall prevention program includes assessment, minimization or elimination of hazards, intervention strategies, procedures and policies, staff and patient/family education, fall prevention devices and monitoring of program effectiveness. T F Attention Managers - for the answers to this quiz, please contact the Regional Patient Safety Coordinator. 10676232412 DRAFT Page 16 of 16