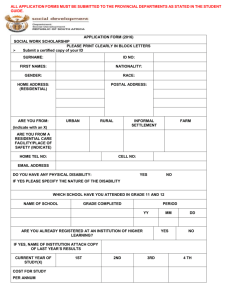
219Kb Word doc - University of the Witwatersrand
advertisement

FROM POLICY, THROUGH BUDGETS, TO IMPLEMENTATION: Delivering quality health care services Authors: Barbara Klugman, Women’s Health Project, University of the Witwatersrand Di McIntyre, Health Economics Unit, University of Cape Town May 2000 For the Women’s Budget Initiative 1 Acknowledgements We would like to thank the following people for participating in the initial workshop: Alex van den Heever, Department of Health, Gauteng Debbie Budlender, Community Agency for Social Enquiry Essina Mabitsela, Department of Health, Northern Province Khin San Tint, Women’s Health Project Peter Barron, Initiative for Sub-District Support Sanjani Varkey, Women’s Health Project Sharon Fonn, Women’s Health Project Nancy Nyathikazi, national Department of Health Maki Pooe, national Department of Welfare Suzette Kotze, national Department of Welfare Marion Stevens, Women’s Health Project Mastoera Sadan, Idasa Budget Information Service We would like to thank Lucy Gilson for her input regarding the interview schedule and comments on an earlier draft, Peter Barron and Khin San Tint for comments on various drafts, Neva Seidman-Makgetla for providing the employment statistics, and Debbie Budlender for her support and helpful inputs throughout. The authors remain responsible for any errors and omissions. 2 1 1.1 THE POLICY CONTEXT INTRODUCTION 1.1.1 What this paper is about This paper explores the experiences and views of government health officials in managing the rapid policy change and ongoing restructuring since 1994. It considers the impact of policies and restructuring on government’s goal to deliver equitable and high quality health services. The research for the paper was done as part of the Women’s Budget Initiative (WBI). The WBI analyses the impact of government budgets on women and men, girls and boys, and different groups of these. The analysis involves four steps: describing the situation of women and men, girls and boys in a particular sector; deciding if policy matches that situation; seeing if the necessary budget is given to implement gender-sensitive policy; and assessing what happens when it is implemented. The WBI was established in mid-1995. In the first three years the initiative looked at the budgets of all national - and to a lesser extent provincial - departments. For example, the second year’s studies included an analysis by Marion Stevens of health policy and budgets (Stevens, 1997). In the fourth year, the WBI looked, among other things, at the budgets of five municipalities. This paper starts to look at the linkages between the different spheres. It focuses, in particular, on how national, provincial and local relate to each other in the policymaking, budgeting and implementation for new policies. The paper is divided into three sections. The first section provides a brief description of the political and structural context of health system reform. The second section presents the research findings. There are three sub-sections to this section. The sub-sections match the second, third and fourth steps listed above: policy decision-making issues; budgeting and financial management issues; and service delivery or implementation issues. The third section of the paper discusses the linkage between broad policy regarding spheres of government, programming and budgets, and attempts to provide high quality health services to meet the health needs of different members of society and to promote social justice in general and gender equality in particular. 1.1.2 Why should a Women’s Budget Initiative look at general budgeting? When interviewees were told that this research was being done for the Women’s Budget Initiative, and that the interviewer was from the Women’s Health Project, they assumed that we would be discussing reproductive health. However, neither health policy content generally, nor women-specific policies in particular, are the focus of this study. 3 What is ‘women’s health’? Many interviewees assumed that a study for the Women’s Budget Initiative must be concerned with reproduction. Government policy also often equates ‘women’ with ‘mothers’ and ‘reproduction’ (Klugman, 1999). Firstly, girls’ and womens’ needs in relation to health services begin long before adolescence and end in old age. Reproductive matters are an important, but not the only, component. Secondly, in addition to women’s individual needs, women are the main caregivers in society. As caregivers they come into contact with the health services both when bringing the sick, whether children or the elderly, to use health services, and in caring for them in the home. Finally, the vast majority of health workers are women. Their role as workers is not fully valued because it is seen as ‘women’s work’. The study takes as given the gender-sensitivity of Department of Health policy since 1994 (See Stevens, 1997; Klugman, 1999 for discussion). It can do this because, in broad terms, the policies of the Department of Health show a clear commitment to equity, particularly to meeting the needs of the poor and of the predominant users, women and children (see Stevens, 1997, for previous WBI analysis of South Africa’s health policy and budget). This study moves beyond this question, to explore constraints in moving from policy to implementation. Policy does not have any value for women users if the services aren’t accessible and of good quality. There are three important issues which emerge immediately when looking at implementation of health policy in post-apartheid South Africa. Firstly, because of the way the Constitution allocates functions, health, in particular, has to find ways for all three spheres – national, provincial and local – to work together if implementation is to be effective. Added to this is the health district concept which, at present, sits somewhere between provincial and local. So one major strand of the report looks at relationships between spheres. The second issue is the large number of new policies introduced since 1994. So a second major strand is how services have been affected by multiple, simultaneous and rapid changes. The third challenge is that all this change must be implemented through and in structures which are top-down and which do not value initiative or problem-solving from below. These characteristics are gendered to the extent that those ‘below’ are overwhelmingly women, while men predominate in the top positions. Further, even when women are in leadership posts, they often follow the established (male) ‘way of doing business’. Gender is about relationships, and relationships are about process and power. This paper looks at how relationships and power, both within the health services and between service providers and users, must change if the government is to realise its goals of promoting good health and preventing illness. The study asks who makes decisions, particularly about financial and other resources, and how such decisions are made. It asks whether there is transparency in decision-making; whether people at all levels are valued, and whether their experience and knowledge is taken into account. 4 1.1.3 Where this paper fits in with other research This paper adds to a growing pool of South African research on related issues. Other research has also looked at how resource allocation decisions are made nationally (Gilson et al, 1999) and provincially (Brijlal et al, 1997; McIntyre et al,1999). Research has also investigated the challenges to delivery of specific policies in the context of health service restructuring (Fonn et al, 1998a; 1998b). Likewise, research has looked at how policies such as free primary care services (Gilson et al. 1999) and termination of pregnancy (Stevens, 1998; Klugman, 2000) were developed and implemented. This paper confirms some of what was found by those other studies. It adds to previous research in looking at the relationships between national, provincial and local government. The interviews tell us that to bring about change, we need to know not only in which direction we want to move, but also how to get there. In other words, we need to think about decision-making processes as well as policy (Walt and Gilson 1994; Friedman, 1999; Klugman, 1999). 1.1.4 Methodology The research began off with a workshop of experts from government and health research bodies. The workshop and a literature review then informed the development of the schedules for the interviews which formed the main source of information for the study. Telephonic interviews were held with officials of provincial, regional, district and local government in Gauteng, Northern Cape and Northern Province as well as with a key actor from the national Department of Health, and representatives of the South African Local Government Association (SALGA). Where requested, the interview schedule was sent to interviewees beforehand. Gauteng, Northern Cape and Northern Province were chosen because of their diversity in terms of population size, infrastructure, access to resources and the way in which health delivery is organised. The findings from the study may not be representative of all other provinces, but they do provide some insights, from the implementers themselves, as to current struggles and challenges. 5 The three provinces Gauteng is the mining-industrial heart of the country and makes the largest provincial contribution to South Africa’s economic production. It has the smallest physical area but the second largest population size, and is thus the most densely populated province (432 people per km2). Only 3% of the population in Gauteng live in rural areas. It has a relatively large white population – 23% compared with national average of 11% - while 70% are African compared with the national average of 77%. Gauteng has very large African townships adjacent to wealthier areas, which could mean increased demand for decent services. Gauteng has the highest per capita expenditure on health services. The provincial health budget was R931 per person without medical scheme cover in 1999/2000, compared with the national average of R501. The academic hospital services are also used by residents of other provinces. If we exclude these services, Gauteng still has by far the largest level of per capita public health spending. Northern Cape has the largest physical area but the smallest population. Its population density is only 2,3 people per km2. The vast area and sparse population makes service delivery difficult and relatively costly. It has a large coloured population (52%) and relatively small African population (33%). This population composition means that there was moderate service provision during apartheid through most of the province, with significantly better services in the urban area of Kimberley. The Northern Cape has below average levels of health spending. The provincial health budget was R402 per capita in 1999/2000. Northern Province was formed from four different ‘homelands’ all of which were underfunded during apartheid. Its population density (40 per km2) is similar to the national average (33 per km2). It has the highest level of rural residents. Nearly nine in every ten (89%) people live in rural areas compared with the national average of 46%. It also has the highest percentage of African residents, at 97%. Along with the Eastern Cape, the Northern Province has the highest poverty rate. The Northern Province has one of the lowest levels of health expenditure in South Africa. In 1999/2000, the per capita provincial health budget in Northern Province (R306) was less than a third of the Gauteng per capita health budget (Statistics South Africa, 1998; McIntyre et al, 1999). 1.2 HEALTH POLICY SINCE 1994 1.2.1 The legacy of apartheid Until 1993, there were eighteen Departments of Health at the central and regional government levels. There was the Department of National Health and Population Development, three ‘own affairs’ Departments of Health for coloured, white and Indian people, the health departments of the ten former ‘homelands’ for African people, and the departments of the four former provinces. In addition, half of all local authorities – approximately 400 in total – were involved in health service delivery. Public sector health services were fragmented in a variety of ways. Firstly, there was geographic fragmentation in that there were different types of facilities and different policies in the various provincial and ‘homeland’ health departments. Secondly, there was fragmentation along racial lines. Until the late 1980s, there were separate 6 hospitals for different race groups. Finally, there was fragmentation between curative and preventive health care. The provincial and ‘own affairs’ health departments were responsible for curative care, while local government was responsible for preventive care. The result was a serious lack of coordination in the development of health service infrastructure, inefficient duplication of services and lack of integrated primary health care service provision. Integrated, comprehensive care was provided in former ‘homelands’, but inadequately and with very limited resources. The health system was also biased towards hospital-based, doctor-centred curative care. In 1992/93, 81% of total public sector health care expenditure was allocated to hospitals. Academic and other tertiary hospitals alone accounted for 44% of the total, while only 11% was spent on non-hospital primary care services (McIntyre et al. 1995). In addition, there were large inequities in access to health services between geographic areas and socio-economic groups. 1.2.2 New health policies The White Paper on Health proposed a major reorientation of the South African health sector. A key policy aim was to reduce the disparities and to increase access to improved services. The White Paper specifically states that ‘emphasis should be placed on reaching the poor, the under-served, the aged, women and children, who are among the most vulnerable’ (Department of Health, 1997:13). In line with this commitment, high priority was given to maternal, child and woman’s health (MCWH). A related aspect of the new policy was to achieve universal access to an essential package of primary health care services. The White Paper also says that government will promote ‘a caring ethos’. Means for achieving this include working with health workers and users to define a Charter of Community and Patients’ Rights, and rewarding health workers for ‘compassionate and caring service’ (Department of Health 1997:Ch 4.3). This aspect is now being linked to a general campaign within the civil service called Batho Pele – People First. Building health worker morale and positive attitudes to clients, whether men, women or adolescents, is critical when dealing with health problems that are intimate and frequently caused by gender inequality, such as unwanted pregnancy or HIV. The White Paper’s objectives also include the development of health promotion activities – both provision of information and empowerment of individuals and communities to protect and promote their own health. This is important in relation to gender. Health problems such as violence or sexually transmitted diseases require community-based interventions which target women and men of different ages and actively promote gender equality in order to address the underlying causes. But the White Paper is not explicit on how many of the commitments can be realised, let alone how gender inequity can be addressed within them. 1.2.3 Employment patterns among health workers The White Paper commits government to implement affirmative action within the health services. Since the change of government, women have been promoted into many senior positions in government. However, there has been relatively limited progress within the health sector. 7 In March 2000 a total of 218 244 people were employed by the national and provincial Departments of Health. Overall, women accounted for 74% of these employees. Table 1 indicates that women and black people cluster at the bottom of the hierarchy. The 70 000 unskilled employees account for about one in every ten employees. These workers earn between R1 900 and R2 200 a month. Close on two-thirds (62%) of these lower-paid workers are women, and over half (55%) are African women. Only 2% are white men. In the public service as a whole, there are more or less equal numbers of women and men doing unskilled work. The relatively high share of women in unskilled work in health is probably because most of these jobs involve cleaning, cooking and laundry – traditional women’s roles. Unskilled workers in health face two sector-specific problems. First, they need special skills for dealing with sick people and contagious waste. While some hospitals provide training for cleaners, most do not. And there is neither certification nor additional pay for unskilled employees who acquire this knowledge and skill. Second, there is no clear career path to link unskilled workers to nursing assistants, who make up most of the semi-skilled level in health. As a result, many health workers have stayed on level 2 of the salary scale for decades. Women dominate even more among semi-skilled and professional workers. They account for over three-quarters (77%) of the semi-skilled and unskilled personnel, and 83% of the professional staff such as nurses. Again, African women account for over half (55% and 57% respectively) of these employees. The professions alone account for 36% of all national and provincial health staff, and the semiskilled and skilled account for a further 33%. Nursing is particularly important because, with teaching, it forms one of the two main professions traditionally open to women. Nurses earn an average salary of around R4 200 per month. African nurses earn, on average, ten per cent less than white nurses. These differences reflect the fact that more Africans are staff nurses, who are less qualified than professional nurses and therefore start at a lower salary level. They also reflect the fact that promotions in the public service were historically biased toward whites. The proportion of women declines sharply in management. Just over a third (35%) of middle managers are women, and only 14% of top management. African women account for 9% and 4% respectively of the two groups. White men, meanwhile account for 36% of middle managers and a full 65% of top managers. The latter includes directors and above, who earn over R200 000 a year. The two management groups account for only 3% of all national and provincial health staff, but will make most of the decisions discussed in this report. Table 1: Race and gender in national and provincial health departments African Coloured Indian White Women Men Women Men Women Men Women Men Unskilled 55% 32% 6% 3% 0% 1% 1% 2% Semi- & skilled 55% 17% 11% 2% 2% 2% 9% 2% Professions 57% 10% 10% 2% 3% 1% 14% 4% Middle mngmt 9% 17% 1% 2% 4% 10% 21% 36% Senior mngmt 4% 10% 1% 2% 1% 9% 8% 65% Total 54% 19% 9% 2% 2% 2% 9% 4% Total 100% 100% 100% 100% 100% 100% 8 There are no figures available for employment in health departments of local government. However, previous research has shown that local government employs proportionately fewer women than men. For example, in 1997 under a quarter of all local government employees were women, whereas there were more or less equal numbers of women and men employed in national and provincial government combined (Budlender, 1999:38). Table 2 provides information on average salaries for different occupations within the national and provincial health departments as at March 2000. One weakness of the table is that the employment figures are for all workers in these occupations across all national and provincial departments. For the directly health-related categories, most of the workers will be employed by health departments. For other categories, such as cleaners, many will be employed by other departments. A second weakness of the table is that it reflects basic salaries without overtime. Overtime payment is received predominantly by the higher-paid health workers and will, therefore, make the differences between occupations even bigger than shown in the table. The table does, nevertheless, provide useful information on the comparative financial rewards for different workers. The first three numeric columns in Table 2 give the percentages which white men, African women, and all women constitute of total employment in the category across all government departments. The next column gives total employment in that category, and the final column shows the average annual salary. Cleaners account for 13% of all public service workers and are the lowest paid workers in the health departments. They earn an average annual salary of R23 500. Less than 1% of the cleaners are white men, and 59% are African women. Medical and dental superintendents are the highest paid category, earning an average of R127 700 per year. Over two-fifths (41%) of the superintendents are white men and only 6% are African women. The biggest single health-related category consists of professional nurses. Less than 1% of these workers are white men, only 7% are men, and 73% are African women. Their average salary, at R56 500, is less than half that of the superintendents. 9 Table 2: Average salaries for occupations in health Cleaner Food services worker Household worker Laundry worker Clinical technologist Emergency care practitioner Medical technical officer Chiropodist Clinical psychologist Dental technician Dentist Dietician Forensic analyst Health therapist Medical orthotist and prosthetist Medical physicist Medical technologist Nutritionist Orthopaedic shoemaker Pharmacist Supplementary diagnostic radiographer Medical natural scientist Medical officer Medical/dental superintendent Medicine control officer Optometrist Specialist Nursing assistant Professional nurse Staff nurse White men 0% 1% 0% 0% 25% 9% 4% 47% 24% 65% 38% 1% 42% 1% 54% 59% 8% 0% 42% 21% 1% 24% 37% 41% 21% 38% 59% 1% 0% 0% African women 59% 54% 46% 62% 9% 3% 46% 0% 13% 4% 9% 19% 5% 23% 1% 0% 21% 48% 0% 10% 59% 10% 7% 6% 7% 21% 3% 66% 67% 73% Total Total women employ 67% 57930 71% 11605 88% 13330 74% 4293 60% 261 10% 1814 66% 285 40% 15 66% 287 22% 68 33% 560 94% 269 49% 153 84% 3840 10% 165 19% 32 64% 1393 87% 31 0% 36 59% 1396 60% 138 61% 169 33% 8194 22% 232 57% 28 38% 24 23% 4455 91% 28913 93% 53351 94% 22016 Average salary 23500 25100 26800 25500 54100 38500 39000 51900 61200 66400 101100 58700 86200 56200 56800 91700 65500 77100 50800 69800 42300 96700 88400 127700 104700 26200 98100 33500 56500 41600 The figures above reflect the institutionalisation of white power under apartheid. They also reflect the institutionalisation of men’s decision-making, even in an area such as health which employs mostly women and serves mostly women and children. This is the workplace and health system culture into which new policies are being introduced. Before and since the White Paper, there have been a number of specific policies which address women’s reproductive health needs or which have other clear gender implications. For example, in April 1994 President Mandela announced that there would be free health care for all expectant and lactating mothers and for children under six. In the context of women’s lesser access to income, this policy is directly redistributive towards women and children. In 1996 the Termination of Pregnancy Act was passed, providing – in law if not yet adequately in practice – for much greater freedom of choice in respect of abortion. More recently, a cervical screening policy has been approved which promises ten-yearly checkups for women from age 30. At the practical, administrative level, the Department of Health has approved the idea of women’s health cards. It has also launched a system of confidential enquiries into maternal death, ensuring that every pregnancy-related death in hospitals is 10 investigated, and drawing on these findings to improve service quality (Department of Health 1998). 1.2.4 Restructuring the public health sector Restructuring aims to transform the previous fragmented system into a comprehensive and integrated one. The 18 health departments have been streamlined into one national Department of Health and nine provincial health departments. This process was not simple. The appointment of senior health department managers was only completed some 18 months after the April 1994 elections (Tollman and Rispel, 1995). Further, transformation has happened alongside the introduction of new policies. This research illustrates the many ways in which these simultaneous processes have complicated each other. The Constitution allocates health functions between national, provincial and local government. National government is primarily responsible for policy development and overall health sector coordination. The provinces have the greatest service provision responsibilities. These include all hospital services and some, mainly curative, primary care services. In many provinces, health regions have been created and some service management responsibilities decentralised to this level. The regions are seen as an interim structure until health districts (see below) have been successfully developed. The exact responsibility of local government remains unclear. The Constitution states that local government is responsible for ‘municipal health services’ but does not define these. Only in mid-2000 was there some agreement that municipal health services should be interpreted as integrated and comprehensive primary care services. The attempt to provide integrated services is affected by the history of service provision in the country. The historical separation of preventive and curative services is one impediment. This is exacerbated by the entirely separate provision of some services, such as ‘family planning’, from other primary care services. The debate about definitions was complicated by the historically uneven provision of health services by local government. In larger cities and towns, particularly in the metropolitan areas, municipalities had an extensive network of clinics providing preventive health services. The clinics often operated side-by-side with separate provincial clinics which provided curative services. The majority of small town and rural municipalities meanwhile provided minimal health services. In former ‘homeland’ areas, there was no local government health service provision. Instead, integrated, but poorly resourced, primary health care services were provided by the homeland authorities. Today most municipalities continue to be largely responsible for preventive and promotive primary care services. However, there is a gradual shift towards all primary care facilities – whether provincial or local – providing comprehensive, integrated primary care services. The historical patterns are, however, reflected in a bias among our interviewees in that we do not have local government representatives in areas where local government is not responsible for any health service delivery at present. 11 The creation of a District Health System (DHS) was proposed in the African National Congress’ National Health Plan. The White Paper on Health sees health districts as the ‘major locus of implementation’ (Department of Health 1997:12). It is proposed that districts will be responsible for non-specialist hospitals and comprehensive primary care services. Regions and districts – each province is different There has been uneven progress towards the development of districts in the different provinces. In Gauteng there is a clear distinction between regional offices and districts. Regions in Gauteng operate as extensions of the provincial sphere. In Northern Province there is no clear distinction between regions and districts. The province is waiting for demarcation of local government boundaries to be finalised. Northern Cape has regions rather than districts because of the large distances and small population. There are two important obstacles to the implementation of a DHS. Firstly, there are problems with demarcation of district boundaries. National guidelines suggested that the district boundaries should preferably match those of local government, and the administrative boundaries of other sectors. Matching boundaries are important if there is to be effective inter-sectoral collaboration. Some provinces such as the Eastern Cape and Mpumalanga have already gone ahead with health district boundary demarcation, although these will require revision to account for changes in local government. Others are leaving the final decisions until local government boundaries and structures are finalised in mid-2000. The second big obstacle to DHS development is the continuing debate about governance. All recent policy documents say that district health services must be accountable to local government rather than provincial. However, provinces are allowed to develop the governance mechanisms that they regard as appropriate. For example, if they think that local government does not have the capacity to provide health services, provinces could provide them. This has resulted in different governance options in different provinces. Very recently, it has been decided that local governments in the metropolitan areas will assume responsibility for all primary care services as soon as possible. Handing over power is also never easy. Power and Robbins describe the challenge facing provincial health department managers as follows: ‘Having been charged with overall responsibility, and having painstakingly gathered the reins of overall control into the provincial fist, the next step … [is] to give a lot of it away again to the regions and districts (and in many areas, local authorities)’ (1996: 35). Nevertheless, there is a firm commitment to the establishment of a DHS. 1.2.5Budgeting processes Overall government spending limits are determined through the medium-term fiscal framework. The framework is based on estimated growth rates of gross domestic product (GDP), and the budget deficit and other targets set in the Growth, Employment and Redistribution Strategy (GEAR) strategy. The fiscal framework 12 covers the vast majority of government revenue, apart from the small amount of ‘own revenue’ generated by local government. A ‘top-slice’ is removed from this global budget to cover debt-servicing costs, standing appropriations (such as the International Monetary Fund subscription) and a contingency reserve. Funds remaining after the ‘top-slice’ are then allocated to the three spheres of government – national, provincial and local – in what is called the ‘vertical division’. This division is based on the service and other responsibilities which each sphere has. The total provincial allocation is then divided between the nine provinces through the ‘horizontal division’. A formula which estimates the relative need in each province for specific services (including health, education and social welfare) is used for the horizontal division. The formula previously gave an extra weighting to women, children and old people in its health component because these groups tend to need health services more. For the 1999/2000 budget, the Department of Finance removed this weighting, making the formula less gender-sensitive. The health component now consists only of the proportion of the population which is not covered by medical aid schemes plus a small allowance for those who are members of medical schemes. The Department of Finance used a horizontal division formula for the local government sphere for the first time in the 2000/01 budget cycle. The local government formula is based on estimated expenditure needed to deliver basic services to poor residents who cannot pay for services themselves. The formula is adjusted for ‘own revenue’ generated by local government. Provinces have very limited revenue-raising powers, but some of the wealthier urban municipalities are able to generate considerable revenue through turnover and payroll levies, property taxes, sales of electricity and water, and other sources. At present, the basic services included in the local government formula are electricity, water, sanitation and refuse removal. Provision of health services by local government is not taken into account when calculating either the vertical or horizontal divisions for local government. The national Department of Health and all other national spending agencies negotiate with the Department of State Expenditure for their share of the total allocation to national government. Similarly, provincial Departments of Health and other departments negotiate with their treasuries for a share of the provincial resources. Total provincial resources are made up of the allocations from the vertical and horizontal divisions, together with a small amount – usually less than 5% - of provincially generated revenue. In addition, provincial health departments also receive funds from the national Department of Health in the form of conditional grants. Conditional grants are a mechanism of ‘protecting’ (‘ring-fencing’) funding for specific activities that are regarded as priorities. The funds are given on condition that they are used only for the purpose specified. The health sector has conditional grants for: Central hospitals: This grant is only given to Gauteng, Western Cape, KwaZuluNatal and Free State to cover the costs of tertiary and referral services used by residents of other provinces. Health professionals’ training and research: All provinces receive a grant, but the largest shares go to Gauteng, Western Cape, KwaZulu-Natal and Free State. 13 Redistribution of specialised health services: These grants are for the development of specialised services in provinces that currently do not have them. The Primary School Nutrition Programme (PSNP): All provinces receive this grant. The largest shares going to the Eastern Cape, KwaZulu-Natal and Northern Province. Hospital rehabilitation and construction: This grant helps provinces improve their hospital services. Durban and Umtata hospitals: This grant goes to KwaZulu-Natal and Eastern Cape respectively. Because health services are not included in the vertical and horizontal divisions for local government, municipal health departments are funded through allocations from local government ‘own revenue’ and subsidies from provincial health departments. Many municipalities do not provide health services and thus receive no subsidy from the province. These tend to be smaller municipalities which also have very little ‘own revenue’. Among municipalities that do provide health services, subsidy payments vary significantly. Subsidies to large urban municipalities tend to be higher in absolute terms because these municipalities have relatively extensive health services. However, subsidies as a percentage of total health expenditure tend to be higher in small towns because their ability to generate ‘own revenue’ is lower. 2 RESEARCH FINDINGS 2.1 DECIDING ON POLICY This section considers two different types of policy. Firstly, three are the policies related to the restructuring of health services described above. Secondly, there are policies related to specific ‘programmes’, such TB or termination of pregnancy (TOP). The national Department of Health coordinates the health sector reform strategy relating to health financing, establishment of districts, management of hospital transformation and so on. The national Department also develops policy on specific health problems such as mental health, mother/child health, nutrition and communicable diseases. At provincial level too, there are units who are responsible for implementation of specific health policies. The people staffing these units are referred to as ‘programme officers’. As noted above, the White Paper states a commitment to integration and provision of comprehensive services at primary care level. Integration cannot happen properly if specific health problems are treated as vertical programmes. Instead, these policies are all meant to be implemented by the same service providers at clinic level. As will be seen below, this can and does lead to tension. 14 2.1.1 Roles in national policy making KEY ISSUES There are clear initiatives to involve provinces and regions in decision-making Some new national appointees had little experience in policy making within government There is an overwhelming quantity of new policy for officials to implement All of those responsible for programming or district development at provincial level say that national asks for their input, which they give. A provincial programme manager explained that the provincial programme managers meet with national on a quarterly basis, send in their inputs, and that national then develops the policy: ‘They don’t do it without the province.’. The provincial managers, in turn, try to involve regional levels in providing such input. However, some of those interviewed at regional level said that this does not happen adequately. They said that this explains why national and provincial policies are not always implementable: ‘It’s totally top down.’ To complicate matters, the changes in government personnel after the 1994 elections meant that many of the new appointees to the national Department of Health had relatively limited policy making experience. In the interim some of the provinces moved ahead on their own. A more experienced provincial informant noted, however, that ‘national has now caught up and our role does have to change. We should … be feeding into their processes.’ There are a wide range of new policies. Some relate to structure – the integration of different authorities, the move towards a district health system, and some to finances – free health care, social health insurance, and mechanisms for financial management. Others relate to specific health programmes where there have been major policy shifts. These include everything from sexually transmitted diseases to TB. All the informants spoke of the impact and confusion created by this plethora of policies. Many felt there should be greater clarity about priorities rather than what a provincial interviewee termed ‘this shopping list approach to policy’. On top of health-specific policies, staff must deal with a range of internal institutional issues. A provincial official explained that there are: ‘the [Employment] Equity bill and the new Labour Relations Act. We’re bombarded with all this legislation in a very short space of time. To assimilate and implement it is quite difficult… and you’re not a legal person… All of a sudden you have to do something differently and you’re not quite geared for it.’ 15 2.1.2 Regional and district involvement in provincial policy making KEY ISSUES The roles and responsibilities of programme management and line management sometimes create contradictions There is often no time for consultation when time-frames are set for policy implementation One problem that was repeatedly raised was the division between programmes (responsible for specific components such as communicable diseases or mother and child health) and line management (responsible for overall health service delivery). Where provincial programme officers are prescriptive as to when and by whom policies should be implemented, it can create tensions at regional or district level, where there may not be the skills, human resources and management capacity in place. This applies even when the programme officer provides the necessary funds. A number of interviewees argued that it would be better if there were fewer programme officers. Others said it was a transitional problem and, with time, people were learning to work together. Another issue is that consultation takes time. Provinces often want to rework national policy to make it provincially relevant. If they attempt to incorporate participation from regions, it ‘takes quite a long time’. In other cases, policy doesn’t require reworking, but there are other time pressures. One provincial manager described how the Hib vaccine1 came with a ‘D-date’ – it had to be introduced on the first of July. This meant that every region had to have training in a short space of time. In another province, a regional manager complained that ‘They just tell us that ‘this is the policy from national and you have to implement it’ – like that Hib for children… It’s twice the price. When we heard about it, it was in June and implemented in July, so we didn’t even have time to argue about the whole issue.’ The reference to price alludes to financial resources. These are discussed in more detail below. 2.1.3 Local involvement in national, provincial and district policy making KEY ISSUES Most people agree that local authorities should be represented in national decision-making, but there are logistical difficulties. Local authorities tend to be represented at national level only in relation to financing or restructuring policy issues, but not in relation to policy on clinical issues. Provincial-local relations usually reflect lack of communication, mistrust and little joint planning despite their interdependence for the delivery of PHC services. Most informants acknowledged that local authorities need representation in policymaking at national level. There are logistical factors which make real representation difficult. The first relates to the fact that local boundaries have not yet been finalised. Hib – Haemophilus influenzae type b – is a newly introduced vaccine to address a bacterium which is the second most important cause of pneumonia and meningitis in children under five. 1 16 The second relates to lack of capacity of some local authorities. The third is the way in which local authorities are organised. Formally, the mechanisms for representation are in place. However, as a provincial representative noted, ‘Intention is one thing but implementing that is another. For instance in Minmec now officially we’ve got positions for local councillors but what’s happening is that how SALGA is structured is, it’s a national association of provincial associations, but the provincial associations are made up of individual councils. So it’s hard for provincial associations to represent individual councils.’ Those who have participated in the policy process since the change of government report substantial improvements, ‘Having worked in local government all my life, I’ve seen a very dynamic swing from national planning to bottom up planning… Certainly no decision will be accepted if there hasn’t been a SALGA input. National have realised you have to have local government input.’ Those who are not directly involved are more critical. One reported that he himself gave input to national level, but that he often had to take the initiative as papers for comment were not always passed on. In addition, there are gaps as to the kinds of policy issues on which there is formal representation of local government at national level. Representation tends to focus on major restructuring or financing issues, rather than issues of programming. This can be a source of tension. A researcher observes that ‘some of the more nitty-gritty stuff, like programme implementation, should involve all three spheres. You will be told that it is being done like that, but it’s not being done enough’. Looking at province and local, in some areas, the policy-making and planning relationship seems to be good. A local government informant reported: ‘We’re very much involved from local level because of this technical team with regional directors and heads of health services…[It is] a political decision but as a technical group we provide the information.’ However, as with national policy, there are logistical problems. Firstly, not all local authorities can be represented directly. For at least one local informant, it appeared that, because of the number of local authorities, ‘mostly when they make decisions they make it on their own.’ Others observed, more optimistically, that after the demarcation there would be fewer local authorities. They said that this would ease, if not remove, this problem. The current difficulties are reflected in frequent expressions of frustration from local officials. The following is typical: ‘I don’t think that from the national or provincial side they’re aware of what is going on at grassroots level. They’re sitting with all these bills and acts and policies that we try to apply. But sometimes we’re not able to. We don’t have the human resources and financial resources.’ The same informant gave the policy on psychiatric services as an example. He pointed to deficiencies in both infrastructure and capacity. He said that he had told his colleagues ‘to discuss it with the province, rather than people saying we won’t do it.’ But he also noted that it was not always appropriate to blame the province, as local officials were ‘also clinging to old things. People have a lot of resistance to change’. 17 There were several other instances which pointed to differing perceptions of a single situation. For example, the manager of a historically white local authority said that the neighbouring historically black township desperately needed a clinic. He said the province refused to subsidise a clinic in the township, yet had built a health centre only 500 metres away from a hospital. The same informant said that the provision of different services by different authorities causes confusion for communities. He said he was also not able to respond directly to community requests for services, since the resources lay with province and there was inadequate cooperation. Yet a regional informant in the same region said that province and local were planning together well: ‘We sit around the table and see whether the department will afford (what the council asks for)’. While there are clearly ongoing difficulties with relationships, a local authority official reported that things were improving: ‘The days of territorial aggression are gone [in] most of the provinces. It exists on both sides but I’ve served on these committees … since ‘94 and before and I’ve seen a major shift in the relationships which has been very exciting.’ 2.1.4 Operating in the interim KEY ISSUES The interim state of local government makes the daily process of decisionmaking difficult. There is often ‘dual accountability’ where local management is responsible to both local councils and province because of provincial subsidies. There is slow but increasing recognition by management in other spheres of local authorities as equal partners. Racial tensions continue to colour some of the relationships. ‘We have new structures with old legislation. The Health Act of 1977 is still in force. The constitution makes reference to … ‘municipal health services’ which is not defined… There appears to be national agreement that local government must be in the foundation of service delivery including the district health system… but in some areas it’ll take years to get that capacity’ (Local government official). Interim arrangements still apply in two broad areas. One relates to the designation of districts, the mechanisms of decision-making for districts, and the relationship between districts and local authorities. The second relates to the division of responsibility for delivery of primary care services between local authorities and provinces. In some cases, such as the Northern Cape, which have traditionally provided most of the funds to local authorities, the province has decided to take over local authority services. However, in most provinces, where there are long-standing, functional local health services, these are continuing. In these cases there are, nevertheless, still tensions around subsidies and around decision-making. The situation is one of ongoing negotiation, tension and uncertainty. Provincial informants spoke about how different employers in the local sphere create dual 18 accountabilities, confusion and lack of parity in conditions of service. A regional manager described the tension of knowing that services will ultimately be run at local level, but seeing that there is little capacity – or even willingness – at present to do so: ‘We almost completely run the local authority services anyway. They more or less wash their hands of them. We’ve given them money for running cost,s but sometimes they’ll refuse to buy cleaning material and that kind of thing, saying they’ve run out of money’ A local official meanwhile stressed the need for joint planning, but said this was impossible, despite ongoing meetings, when demarcation had not been finalised. Managers of urban councils, largely historically white, generally have more confidence in their capacity to manage delivery, but acknowledge that provinces will probably retain responsibility for the meantime in rural areas: ‘[Urban] municipalities are in a better position at this point in time – they are on top of things. The rural areas are where the province is busy.’ Sometimes the barriers to collaboration are a direct result of the apartheid divides. Few interviewees were explicit on this issue, but it is clear that in many areas there is distrust across race lines. Some of this is based on real experience, and some on the assumption that white officials will not want to participate in the new dispensation. A white local authority official described the problem thus: ‘ Transformation is taking place, but not as fast as the political bodies would want it to take place…A new government has a lot of people they don’t want there and can’t get rid of them… I want the job to get done and I get blocked because of suspicion that I have a hidden agenda.’ An aggravating factor is that many (mainly white) senior officials operate in an ‘acting’ capacity for long periods of time while other candidates are sought. Meanwhile these acting officials are expected to implement new policies without the necessary trust and authority. 2.1.5 Involvement of politicians KEY ISSUES Politicians are beginning to recognise that policy must be realistic Some officials complain that politicians’ personal priorities do not match equity imperatives Local authority managers seem to have closer links with councillors than provincial or regional managers do with MECs. Health officials said that politicians had in the past failed to consider the financial implications of new policies. As in many other areas, however, they said there had been an improvement. A local authority official explained: ‘The paw-paw hit the fan with free PHC service, and politicians are beginning to realise that they can’t make broad policy decisions without realising the financing implications… People are cautious now about making rash decisions.’ But officials noted that politicians sometimes don’t adopt budget-related proposals which might be politically unpopular, and that this constrains their ability to control expenditure. A regional manager cited the example of a 5 000-person town with a 19 hospital but where ‘no politician is prepared to close the hospital. So we’re told to fiddle around the edges when those big political things are decided.’ Another interviewee reported a case where politicians ‘for their own political reasons’ will not close a regional office for which there are no funds. Both provincial and local spheres of government have formalised systems whereby officials give input to, and gain guidance from, politicians. Those responsible for managing health in the local government sphere seem to have closer and more responsive relationships with politicians. One described the relationship as follows: ‘Any new policy or new thing I have to implement I always go to council, give the details, advise them on all those things. Normally they take note and approve.’ This informant also noted that, before reporting to council, he liaised closely with province. In the provincial sphere the most senior officials engage with the Health MEC, but the rest appear to feel rather distant from the politicians. Regional managers, likewise said they do not have formalised ongoing interaction with politicians. Instead there are once-off interactions. They said the result was that politicians criticised them ‘ for the smallest thing.’ They also complained about inconsistent cooperation from local politicians: ‘If the local politicians want something, then the councillors are keen to work with us. But if they decide it’s a boring issue, we don’t see them in our meeting. But when the pawpaw hits the fan, then they run straight to the MEC.’ Some efforts are being made to overcome these difficulties. One local level official described the Gauteng District Health Systems Committee which includes all the heads of health services of local government and the five regional directors at provincial level. This is a technical support body to politicians who sit on the Interim Provincial Health Authority, which is chaired by the MEC for health and has 22 local government politicians. The official said that the mechanism is helping all spheres cope with the transition. The situation contrasts starkly with another province where a regional manager noted: ‘There is a meeting between MECs and local government people but we’ve never attended that meeting although we were promised we should, and they look at plans.’ 2.2 BUDGETS AND FINANCIAL RESOURCES Question: Do you know how much money you can spend this year? Answer: ‘They know but I don’t know’ (Clinic Sister) ‘If something new comes in, someone has to work out what they cut’ (Provincial finance manager) The bulk of public sector health care expenditure occurs within the provincial sphere. This section therefore focuses first on provincial health departments and, in particular, the challenges facing health district and regional managers. Thereafter the section looks at the interaction between provincial and local government health departments around financial resources. Finally, donor funding and funding of NGOs are briefly reviewed. 20 2.2.1 Budget decision-making processes KEY ISSUES Budget decision-making is still highly centralised Financial information systems remain weak in some provinces There is inadequate understanding of resource allocation and budget decision making processes at lower levels There is limited integration of planning and budgeting There is wider involvement in the budgeting process within local governments The Primary Health Care (PHC) approach suggests that detailed health service planning, and decisions about how resources are to be used, should be decentralised as far as possible. This should ensure that locally identified needs can be met optimally. Within the South African health system, it means that the district office (or the regional office where districts have not been established) should be responsible for planning and budgeting for health services. At the same time, plans and budgets developed at a decentralised level need to be balanced with the goal of equitable distribution of health care resources between and within provinces. Previous research has shown the enormous inequities in the distribution of health care expenditure between health districts and regions (Brijlal et al., 1997; McIntyre et al., 1999). Some provinces have developed needs-based formulae to assist in determining equitable health district or region budgets. These formulae are usually based on the size of the population in each district or region. They may also include other indicators of relative need for health services such as the age and gender composition of the population and relative poverty levels (McIntyre et al., 1999). Equity is not only about the distribution of funds geographically. It is also about the nature of services provided. Despite government’s commitment to increasing access at primary care level, most of the money still goes to hospitals, and particularly to academic and other specialist hospitals. In response to this, government is currently developing and costing a PHC package. This package will provide a norm for the quantity and quality of primary care health services that each province should provide. The package specifies the type of services that should be provided, a target utilisation rate and quality standards that should be applied. The package is intended to promote more uniform provision of high quality services across provinces. However, provincial health departments will still have to find ways of securing adequate resources to fund this package. All three provinces are undertaking major reforms in their budgeting and financial systems. One financial manager described both the goals and difficulties: ‘In the past… one person sat in a room and did it. Now … the high levels are decided by the Health Department management i.e. the allocations by programme and subprogramme. Then there is a process of discussion and further consultation about more detailed allocation within that… It doesn’t work smoothly at the moment because the departmental structures themselves are such that they don’t have adequate support for responding…But I think that what we’re doing now is to make the bigger decisions around a table – a budget committee has been set up with chairs 21 of sectoral committees… They’d go away and prioritise the individual entities within them.’ At present budget information usually does not penetrate beyond senior management. Many interviewees described their frustrations with this situation. A provincial director complained that she knows neither how much the directorate is allocated, nor how much has been spent: ‘Every year we sit down, plan and budget. Then present it. Then they’ll tell you it’ll be discussed by senior management but you’re never told ‘yes you can spend x much money or more’… We just work and spend and as long as it’s within my signing powers, I sign. As long as I’m sure it’s not corruption. But I don’t know how much my directorate as a whole has spent from April 1999 until now.’ The financial manager from the same province explained that it had not at first been possible to budget accurately because there was no historical data on spending: ‘In the past at head office level they wouldn’t necessarily have had their budgets revealed to them because it was all centralised, primarily because expenditures weren’t tracked at a directorate and chief directorate level… If you don’t know what they were spending in the past, it’s impossible to budget.’ The financial manager explained that it was only in the 1999/2000 financial year that there had been real budgeting based on expenditure for programmes. The lengthy process of improving financial management systems is one part of the problem. Another relates to the decision-making process itself in a situation of tight resources. A provincial manager argued as follows: ‘I know there’s no money (but) we should be included in the decisions of the budgets at provincial level.’ There are efforts in most provinces to promote decentralised budgeting. Regions (and districts where they exist) are requested to prepare their own plans and budgets and submit them to provinces. There is, however, a perception at region and district level that local plans and budgets are not given adequate consideration. A district manager reported as follows: ‘We do plan and give it to them and it comes back being a different thing altogether …We’re asked to budget and send figures, and then it gets cut.’ In some provinces provincial changes to the budgets submitted by lower levels may occur because the province is aiming at greater equity between districts or regions. If this is the case, it seems that the province level has not communicated adequately about equity-based resource allocation procedures. Previous research has indicated that one reason that provincial level staff do not base allocations on locally developed budgets is because they are regarded as ‘completely unrealistic’ (McIntyre et al., 1999). On the one hand, the preparation of ‘unrealistic’ budgets may be due to ‘budget gaming’ whereby district or regional staff deliberately inflate budgets in the knowledge that they will be cut. They hope that, after the cut, they will then get an amount closer to what they actually need. One district interviewee suggested this practice when he said that ‘sometimes we exaggerate what we need.’ Another problem is that districts or regions are sometimes not fully informed about overall budget constraints (McIntyre et al., 1999). Where guideline 22 allocations are provided, the purpose is not always properly explained or understood. A regional official complained: ‘We end up having a sort of an amount we should budget within. You are made to feel that you are contributing but at the end you are told not to exceed here.’ Another area of conflict arises because of the institutional confusion - described above - between regional structures and programmes. One regional manager reported: ‘We do strategic planning together with the vertical programmes and we tell them what our needs are, and they identify more needs. But they don’t come back and tell us what they’re going to do to meet those needs, nor what it will cost. Or they don’t budget from their budget – they expect all the money to come from the region.’ One way of promoting greater realism is to integrate planning and budgeting. A detailed district or regional plan identifies health service priorities and evaluates what can feasibly be achieved within the coming year and in the medium-term. If this planning occurs within the context of a guideline budget allocation, realism can be enhanced. Numerous interviewees referred to the current lack of integration of planning and budgeting processes. Thus, a provincial official explained that they are ‘developing five year plans which is linked to deliverables but we haven’t aligned it to the MTEF [medium term expenditure framework] … the two processes aren’t tied together’. Another provincial interviewee noted that ‘there isn’t a language of dialogue between you [planners/operational managers] and the budget. We haven’t bridged that interface. We don’t talk the same language’ Again, however, there are some positive reports. A provincial official described a collaborative process for budgeting at regional level as follows: ‘I do [district budgeting] together with community matrons responsible for each district… In the initial budgeting when we’re all seated together there – we have the cake there and we’re cutting it. The matrons are motivating what they need. They come to the meeting prepared. Then sometimes if there’s shortage somewhere we have to prioritise, negotiate with the other ones on what can wait until the next year’. Within the local government sphere, long-established local authorities described formalised and effective systems of budgeting and financial management. Where, however, they relied on subsidies from the province, the unreliability of the subsidy payments was said to undermine local government systems. 2.2.2 Financial management capacity issues KEY ISSUES There are still capacity constraints, despite ongoing attention to this issue Financial management training has been initiated but capacity development will take considerable time and energy Provincial managers do not want to decentralise responsibility too rapidly, but regions and districts are eager to assume responsibility Financial management capacity is better developed at local government level than within many provinces 23 Most informants agree that devolution of budgeting and financial management is desirable because, as a provincial financial manager expressed it, ‘when it happens centrally you can’t take into account any subtlety’. However, this presumes capacity, which by and large is still not there. Interviewees cited the lack of skilled personnel and adequate information systems as key obstacles to successful decentralised budgeting. Despite attention being focused on this issue since at least 1997, there appears to be limited progress. One possible interim solution is to redistribute certain managerial staff from head offices. However, a frustrated regional manager observed: ‘They’ve done decentralisation hard here in the Northern Cape… We do all that and not one person has been decentralised from Kimberley.’ Capacity is about lack of systems and lack of downward accountability as much as about lack of skills. Thus many lower level interviewees talked about the difficulties of keeping to budget in the absence of financial information: ‘In the middle of the year we find we don’t have that amount of money anymore, so we can’t continue our plans… They don’t … correspond with us. We just see in the reports what has been spent. And when we do inquiries we hear ‘No, they took away some money from here or there.’’ In some provinces, systems for financial monitoring appear to be operating at least within the provincial sphere. Officials spoke about how these systems have improved both their ability to plan, and their sense of control over their work. Thus one official in the Northern Province explained: ‘Each time you spend on any activity you’re able to check expenditure against budget. Every programme can tell very easily without having to go to finance people.’ Another confirmed that ‘every month [I get] a printout to show what I’ve spent on travelling, workshops etc.’ Provincial level officials clearly have concerns about decentralising too rapidly. One interviewee noted: ‘There’s enormous risks when you decentralise because they may make mistakes and leave the department in jeopardy.’ The interviewee went on to suggest that it was not only capacity, but that lower level officials may not ‘fully feel accountable for what you delegate to them.’ However, district and regional managers are eager to take more management responsibility, including planning, budgeting and expenditure control. A regional manager in the Northern Province suggested: ‘Let each cost centre have authority to manage budgets and if anything goes wrong, let that cost centre be held responsible.’. In some provinces, regions and districts have been given ‘responsibility’ for budgeting, but are not given authority for making decisions which impact significantly on resource use. For example, one regional level manager reports that, after asking for security, the province contracted with a private company without involving the regional office in the negotiations: ‘Now we’ve got to pay huge amounts for a security service which we didn’t budget for.’ Within local authorities there seem to be stronger systems in place than within regions and districts. One official described how ‘I’m monitored in terms of performance and output and delivery in terms of an integrated developmental plan and thirdly an internal and external audit, and council … We’re monitored quarterly against the budget… If I want to start cervical screening programmes in informal settlements …, 24 I’d have to go to council and also show them which budgetary provision I would draw on, or find savings from another line item’ . This manager noted that she and her financial staff have been trained to operate cost centre budgeting: ‘Meeting with managers yesterday, they know what it costs to repair taps, to fix a window etc. and they can make an informed decision about what to do.’ Training is happening in other spheres as well. One financial manager used a medical analogy to describe the importance of training reaching all levels: ‘As you get the blood flowing in the system –information at every level, the right administrative personnel at every level, you have a system that can respond… If a region can’t track it’s own expenditure, you can’t expect from them.’ But this official went on to acknowledge that many of the province’s financial problems were at a higher level, and that these had had to be dealt with before the training of others could commence. 2.2.3 Resource constraints KEY ISSUES Resource constraints make restructuring and policy implementation very difficult Unexpected budget cuts and expenditure embargoes cause uncertainty about resource availability There is greater stability where local government health budgets are funded from own revenue Budgeting for new policies while ensuring the continued provision of existing primary care services is particularly difficult in a context of static – or in some provinces, declining – real health budgets. It is particularly difficult in areas that were historically under-resourced (particularly in the former homeland areas). In these areas, although health services were provided previously, they need to be expanded and their quality improved. Managers at all levels concur that resources for health service provision are extremely constrained. A district manager described the shortage of funds as ‘a common disease.’ The high proportion of fixed costs in most health budgets adds to the frustration. In the words of one regional manager: ‘80% of our money is tied in salaries. Another 10% is pharmaceutical services and sundries. So it doesn’t work when they say how much have you budgeted for TB programmes… Why are they bothering about the 6% of the budget we have some manoeuvrability about and not asking about the 94%?’ However, there is a growing awareness that resource constraints will not ease in the foreseeable future and that more can often be achieved with existing resources if there is better prioritisation. Further, when asked if shortage of funds is the biggest barrier to implementation of quality services, almost every interviewee cited health worker attitudes or staff morale as more important than financial resource constraints. Nevertheless, many informants did not see the shortage of funds as excusing arbitrary cuts in the middle, or near the end, of the financial year. Further, some programme managers said that they have sometimes been instructed not to spend except on essentials, even though budgets were not officially cut. These experiences not only 25 limit managers’ ability to implement plans, they may also create mistrust of, and apathy towards, budgeting processes. Clearly the cuts and spending embargoes have profound effects on service delivery. A regional manager described how expenditure can be frozen for months: ‘If something runs out, you can’t replace it. Oxygen cylinders. It’s crazy.’ This same manager observed that budget cuts only seem to affect service delivery while national and provincial level management structures remain unscathed. Activities such as health promotion, community outreach and staff training appear to be particularly ‘soft targets’ in coping with unexpected budget cuts. In addition to budget cuts, some informants spoke of the difficulty in accessing budgeted funds. A provincial official said: ‘You get the budget approved but sometimes must struggle for it to be paid’. Those with more experience of government systems seem to be better placed to overcome this problem: ‘You do access money but it’s tedious. Many signatures. You have to start early.’ Local government interviewees indicated that budgets allocated to them are relatively secure from arbitrary cuts. When asked about cuts, one local government health manager explained that ‘Council doesn’t function that way’. Interviewees nevertheless indicated that subsidies from provincial health departments introduced insecurity into their health budgets. In at least one case, while the province is consciously cutting subsidies, they are expecting the local authority to continue the service without discussion as to whether this is feasible. 2.2.4 Provincial–local government interactions: resource control issues KEY ISSUES Provincial-local government financial interactions involve much conflict and little transparency Local government health services appear increasingly vulnerable due to reducing provincial subsidies and, in some cases, declining budget allocations from own revenue Some local government officials favour direct financing of health services from the national Department of Finance The interaction between provincial and local government health departments around financial resources is usually far from smooth. There is a clear lack of communication about their respective budgets even though both local and provincial managers indicate that the lack of transparency is an impediment to rational planning for integrated service delivery. From the provincial side, interviewees indicated that contributions to health services from local government own revenue are ‘a state secret’. Yet without this information, they argue that they cannot ensure equitable allocation of primary care resources between health districts and regions. On the other hand, local government managers are not provided with information on expenditure at provincial facilities within the boundaries of their local government. Local authority managers also talked about the lack of transparency as to how subsidy decisions are made: ‘No-one knows how the subsidy works - what’s the amount, what’s the percentage… 10 or 15 years ago you’d know what percent.’ This interviewee suggested that the province itself ‘doesn’t know, can’t tell you’. Further, 26 he said that there is no process to facilitate communication: ‘There was a time when they sent us a form to help them budget so we would say what we would need. But that’s come to a standstill.’ Another local interviewee said that in their area subsidies stopped in 1995, but no reasons were provided: ‘We’ve written letters, seen the guys, talked to them. The last reason that we’ve got is that they’re still in the administration process and when it’s finalised they’ll see to the subsidies.’ Provincial managers generally favour continued subsidisation of local government health services through the provincial health department route. However, they want routine information on local government own revenue contributions, and improved accountability for expenditure funded through provincial subsidies. At present, some feel that local governments are ‘doing whatever they want to do with the budget [subsidy]. This is not being controlled by provincial government’. The national Department of Health is developing guidelines for ‘service agreements’ between provincial and local departmentsl. Several provincial manager agree that ‘the service agreements will be useful – we’ll sign them and that will oblige people [local governments] to provide certain services.’ Some local managers – particularly in wealthier councils, are not eager to have their activities monitored by provincial managers. They argued that they are primarily accountable to their local councils: ‘Province provide 17% of my total health budget so I can’t be monitored by another authority who provides a small proportion of my budget’. Local government health managers find themselves under pressure from all sides. On the one hand, provincial health departments feel that insufficient revenue is being allocated by local governments for health services. In addition, provinces appear to be gradually reducing subsidies in anticipation of a unified system where local government is controlled by the third sphere and the province pays only for provincial programmes. Meanwhile, the continuing confusion over functions has been used by some local councils to cut their own revenue health allocations. As one local official explained: ‘Departmental heads think provinces should just take over and pay. But we’re working at community level and will lose that contact if we go to province. We think the municipality should pay more but the department heads don’t like this. Politicians don’t seem that aware of this issue.’ Some local government health managers feel that the solution lies not in the establishment of service agreements, but in direct financing of local government health services from the national Department of Finance level. They argue that health services should in future be taken into account in the vertical and horizontal revenue divisions. Such an arrangement would require increased collaboration between provinces and local government, yet without one of the parties controlling (at least partially) the purse strings for the other party’s services. A local government official argued: ‘It’s imperative that local council services work and you can’t work when someone else is pulling the purse strings.’ This interviewee feels that there is a ‘firm understanding’ of this argument within national government. 27 2.2.5 Donor funding KEY ISSUES Donor funding is not coordinated In most cases, donor funds appear to be negotiated at national level, and then provided to provinces for specific purposes. For example a provincial interviewee described how she was given support for certain aspects of the implementation of the Choice on Termination of Pregnancy Act. In other cases a province or local authority might approach donors directly. For example, one province described how with the Integrated Management of Childhood Disease training, they sent the donor a proposal and conducted the training ‘and they just sent a cheque.’ Similarly, a local authority informant reported: ‘We’re moving ahead with proposals for capital projects to take to donors… I put through a proposal to the regional office but also directly to the Norwegian embassy and all the embassies to ask if they’re interested and could fund part or whole’. It is not clear in this last instance whether the proposal was successful. Donor funding can be a source of tension between programmes and line functions. A regional manager complained: ‘We as regions don’t get donor money but the support services do get donor money and we don’t know what the amounts are and what for… That’s another secret… We are not involved in discussions with donors.’ 2.2.6 Donor and government financial support to NGOs KEY ISSUES Provincial subsidisation of NGO services is gradually increasing The relations between provinces and NGOs are becoming more formalised. In all provinces there are donor-funded activities undertaken by NGOs, universitybased groups or consultants, where the outside group has approached both the province and the donor. The province is asked to support the group’s doing the work within the public health services. The donor is asked to fund their costs and perhaps some of the costs to the province. Much of this work is done with the idea that effective interventions piloted in one place could then be undertaken elsewhere. In some situations, the province does not manage the funds or even the programmes directly, but rather agrees on the broad principles. As one provincial programme manager explained: ‘We work closely with the NGOs. They appoint their own directors and supervisors… We’ve agreed with them in the first place on how money should be spent’. In some cases the provinces subsidise NGOs to provide a service even where there are no external donors. One provincial programme manager said that some care is taken in selecting and monitoring NGOs: ‘We want an NGO that is organised, that has skill in that aspect and will be able to deliver… Then we attend what they do, watching them because we’re subsidising them so we must monitor and evaluate them and get monthly reports and yearly reports from them.’ This informant reported that local councils are involved in the selection and monitoring because it is there that the NGOs are operating. A provincial finance manager spoke about management of funds given 28 to NGOs on tender: ‘There are meant to be service standards with each contract. Contracting hasn’t been brilliant within the province but it’s moved a lot more in that direction.’ 2.3 SERVICE DELIVERY AND IMPLEMENTATION This section considers the implications of policy-making and budgets for implementation. A number of interviewees point out that many of the barriers to implementation lie outside the health services. For example, the policy that every woman should give birth at a health centre may be obstructed by poor infrastructure. A programme manager described how, for example, after two weeks rain’ it’s muddy so there’s no transport so people deliver at home. Ambulances can’t cross the river.’ The present research focuses on barriers within the responsibility of departments of health within all spheres. Many of the communication problems identified in relation to policies and budget apply equally in the process of delivery and monitoring. A provincial official complained: ‘When someone has an idea in September in the national department, it doesn’t seem that unreasonable to expect an answer in October but the request will only get to the region in mid-October… We see plans as an unfortunate thing that managers ask for… [So] everything is always a surprise and a crisis.’ 2.3.1 Budgeting for policy implementation KEY ISSUES Policy developers often don’t consider budget and operational constraints Interim funding helps only in the short-term There is increased awareness of the need to plan and cost new policies Policy implementation may be thwarted by lower levels of management Costing of a basic PHC package is intended to facilitate better prioritisation Many interviewees noted decision-makers’ failure to consider the resource implications of new policies. A provincial official said: ‘Our policies are pie in the sky rather than real… We started off saying things would be delivered because they were the right things and people were entitled. But entitlement without resources doesn’t get you anywhere.’ A financial officer noted that, constitutionally ‘the province has the right to refuse if money doesn’t come – because it’s an unfunded mandate’. However, no interviewee reported any instances of blatant refusal to implement a policy. Instead, those below and even at provincial level report the practical difficulties of implementing policies that may sound good. For example, one regional manager said that the ‘policy says two ambulance men always have to be on an ambulance, and every ambulanceman has to have a course on drowning – so I refused because I don’t have a river! Also there’s no way I’ll ever have two men. We can just afford one’. The same interviewee referred to the policy that no nurse may take X-rays ‘but we have no money for radiographers.’ Another regional manager referred to a policy directive that rape victims should receive AZT: ‘We asked ‘where does the money come from for AZT?’ We just have to provide it because someone has approved the policy… We didn’t have any chance to give our view on the issues.’ 29 Similar issues were raised by local government informants. For them the fact that they are accountable to a different authority exacerbates the tensions. Several local authority interviewees noted that province often fails to consider its funding responsibility in respect of new policy and that local authorities therefore carry an untenable burden. One interviewee observed that this burden comes on top of now having to provide a full range of services for previously under-served black townships: ‘Local government nationally is starting to run into a brick wall having inherited large areas with enormous debts and cultures of non-payment and trying to put money into disadvantaged areas. So in most areas local government can’t continue accepting unfunded mandates.’ Again there was the suggestion that some councils had simply decided simply to refuse to implement. Where policies are introduced in the middle of the financial year, national or provincial government sometimes pays the bill and provides materials for the remainder of that year but expects the implementing level to cover the costs in the following year’s budget. For example, a provincial programme officer described how for TOP she provided equipment and long gloves for all regions; for cervical screening she provided vaginal specula and sterilisers; for immunisation she ordered cooler boxes ‘for a start. Then from then it’s from their budget.’ Similarly, when the women’s health cards were introduced, national government provided the first supplies to the provinces and provinces supplied the regions and hospitals, but regions and hospitals were asked to budget for this the following year. Provinces found that some regions have done so and others have not. One provincial manager attributed this to poor financial management and lack of experience. She argued that ‘they have been workshopped’ but clearly workshops are not enough. A local authority manager complained: ‘We’re rearing to go but… the [women’s health] card is supposed to come from national level but there isn’t a guarantee that the card will be available so we’re scared to implement.’ He said that with the TB register they had implemented but two months later had run out of cards: ‘It becomes very demoralising because we get the flack from the patients.’ Several interviewees suggested that the understanding of policy makers is improving. They said there is increasing recognition that the amount of money available is unlikely to increase dramatically from year to year, and that what is needed is clearer prioritisation. One provincial manager noted that ‘amongst people developing policy … they now do [recognise] that it has to have a price tag attached, that it’s about choices. The idea that we’re going to have to make choices is a painful one … It hasn’t been politically acceptable to say choices are needed.’ Some spoke about how they had, practically, made the choices. Thus a manager in the Northern Province described how, with the introduction of the syndromic approach to STD management: ‘We didn’t motivate for extra money, but to transfer money from other sections in the same PHC budget. Just juggling around. Sometimes we had to give up something. Like we used to have promotional materials like T-shirts and now we have to use cheaper materials.’ 30 In some cases, regional levels have not budgeted for implementation of national and provincial policy even a number of years after implementation. The decision-makers in these regions have seemingly prioritised other expenditures. For example, one programme manager said the health services repeatedly ran out of the necessary equipment for TOP and then approached the province for funds from its contingency budget. The programme officer favoured decentralisation of services but felt disempowered by her lack of influence over the decision-making process: ‘I have to say ‘please, please do this or that’…But then the regions will raise their own constraints and will do it at their own pace.’ Gender issues in decentralisation Decentralisation presumes that decision-makers at lower levels will be guided by the interests of users. However, health priorities have been defined over centuries by a predominantly male profession. It is therefore not surprising that despite national and provincial policy to provide termination of pregnancy services, below provincial level this happens only in one province at one clinic. Yet a recent enquiry into maternal deaths found that unsafe abortion remains a key problem (Department of Health, 1998) and suggests that service managers should give priority to decentralised delivery of TOP services. In recognition of the ongoing problems caused by introduction of many policies without increasing funds, the national level, with the involvement of provinces, is costing a basic PHC package. 2.3.2 Programme priorities and service delivery KEY ISSUES New policies are being brought in when the basic requirements for delivery are not in place Programme managers are often caught between national and implementation levels Separate programmes lead to training overload and duplication Donor funding can undercut attempts at integration Implementation is influenced by the extent of managers’ commitment and capacity for innovation A theme which emerged repeatedly from interviewees responsible for regional or district delivery was that the pace of change was too fast. Interviewees complained that new policies, coming through programme officers, are being brought in when the basic requirements for delivery are not in place. An official responsible for districts complained: ‘Often we’re not doing basic things right yet and programmatic things are more fancy and we can’t afford it or haven’t got resources including ongoing support’. Much of the frustration was directed at programme officers. The method of work for programme officers differs between provinces. All provinces have programme officers at provincial level. However, in Gauteng, there are frequently also programme officers at regional level. These people are the first point of communication for the provincial officer. Elsewhere there are no programme 31 people at regional level, or people in regional offices double up. For example, one person may be responsible both for clinic supervision and AIDS programming. The basic procedure is the same in all provinces. The national develops policy which the provinces must then implement. On receiving the policies, provinces modify the guidelines to suit the situation. They then workshop the modified guidelines and protocols with officials from all levels. Additional training is provided where necessary. The lower levels are than meant to implement while province is responsible for monitoring. There are at least two difficulties with this process. Firstly, all the separate programmes wanting the same group of people to deliver their programmes, while the service deliverers concerned are striving to integrate services. Secondly, there is confusion about the rights and responsibilities of programme officials relative to those in service delivery. The result is frustration on all sides. In terms of the first issue, a regional manager reported: ‘We spend two days every month [at provincial level] and they line up programme people to speak to us – you go in with one wheelbarrow of problems and you leave with two. There’s no time to talk with each other or talking about how we solve problems.’ In relation to the second issue, a senior provincial manager commented on the way in which many provincial programme officers understand and perform their role: ’People need to understand that it’s not enough to be right. You have to come with evidence and we’re not used to evidence…We’re going to need at a policy level… people with skills rather than beliefs. At a local level, once the choices have been made, people need to co-ordinate a job of work rather than seeing themselves as advocates.’ The manager said that the current approach resulted in overlap of roles. A provincial programme manager herself recognised this difficulty and its roots in previous practices: ‘The province tends to keep hands on which is wrong, but with time they let go. Nutrition is a district function, but it’s still run by province… But we’re working on it. It’s the way some of these programmes from the previous government came in.’ The fact that programme officers carry responsibility for policy guidelines, but have no control over implementation creates substantial tensions: ‘You have to achieve things through others - you facilitate but you don’t have the power to say this should happen on this day’. Likewise from the other side, in the words of one regional manager: ‘There’s a tendency of programme managers to interfere with operational issues which drives us berserk.’ Another regional manager noted that, ‘They’re totally unclear on what their role is and national demands things and they’re in the middle and terrified to phone us because we don’t give them what they need.’ The provincial programme managers described one of their roles as monitoring. They do this through visits to sites or calling meetings. The language in which they describe this differs. One programme manager said: ‘We have a checklist and go out in the region and look at certain things to see if they’re done properly.’ Another programme manager focused more on the fact that she must offer support: ‘Involvement is very important, and giving people information is very important. You don’t just say ‘there’s a policy to implement’. They must tell you how they are going to implement – get input from them because the areas are not the same.’ 32 Some districts described provincial programme managers as supportive. Others argued that they never see the programme managers in the field, unless it’s when they bring important visitors, particularly from national. They said that programme managers often have to respond to demands for information from national level and this made them less responsive to districts’ needs. Some local council interviewees expressed confusion about the role of programme officers. They raised concerns both about programme officers’ competence and their understanding of local conditions. One used TB as an example: ‘Our own municipality has done some fundamental work on TB yet we get instructions from province on how we must implement our programmes. In terms of expertise our staff member could teach the province on how to implement a programme so it’s a waste of a resource.’ Another local council manager noted that ‘the provincial co-ordinator is often not au fait with local programmes. We’ve a lot of programmes going on that the provincial co-ordinator is not aware of… Money is given to NGOs by a provincial coordinator for AIDS – that provincial co-ordinator has no idea what that NGO is about. A politician who knows that NGO, if they’ve paid their rates and taxes – that’s the person who’ll know if they’re suitable or not to get HIV/AIDS money.’ This informant stressed that she felt there was a role for programme officers, but that it should be confined to monitoring rather than decision-making. The desire of programme officers to deliver on their job descriptions places pressure on the regional, district or local managers and their staff: ‘If you have competing advocates at provincial department, you get paralysed. High level managers all of whom want their bit because of its importance.’ One of the ways in which the pressure manifests is that each programme officer wants to ensure that clinic level staff are trained in relation to the policies for which they are responsible. Many interviewees recognised that the training can be useful. A local manager reported: ‘I send my staff because we haven’t got a training contingent in our authority… They’re doing a good job.’ However, a provincial manager acknowledged that the training is uncoordinated. She reported that one region said its staff were spending 40% of their time in training course: ‘We’re now discussing if we can’t give people guidelines, - do they need to be trained on everything?’ From the regional side, a manager reported: ‘We’re starting to decide [on training] more and more at a regional level but the reality of what happens is that the provincial office sends you a fax saying that next week there’s training on burns, please send someone. Then that there’s an HIV summit and the Minister wants someone to attend…Everyone’s trained up to their eyeballs.’ In addition to overload, there are financial constraints. For example, a regional manager spoke about the costs of S&T (subsistence and travel) for staff attending training courses. The lack of training co-ordination was raised repeatedly by both provincial and lower level officials. Northern Province officials reported that they had a Human Resource Development unit that was meant to coordinate all training, but that they were not using this resource. Gauteng, on the other hand, reported that it has begun to address 33 the problem. Instead of having different directorates training separately, with resultant depletion of service delivery, they are trying to develop generic and integrated training courses. One example is a ten-day integrated reproductive health course which includes STD, contraception, HIV/AIDS, TOP, violence against women and gender issues training. When there are donor funds or a national conditional grant involved, integration and coordination across programmes and between levels can be even more difficult. A number of provincial managers mentioned examples, such the Integrated Management of Childhood Illnesses. In this case, the Unicef and WHO approach involves training which should be run by districts, but at the moment remains at provincial level and is not integrated. Termination of pregnancy training was also mentioned as a donorfunded and NGO-run initiative which has not been integrated into planning or training at regional level. The impact of new policy is felt beyond the clinic level. In cases where policies require referral, the ability of higher tiers of the system to cope comes into question. A regional manager raised this in relation to cervical screening: ‘I said okay, so if I implement it routinely, what are the follow up services? They said there can be five people a week …at the hospital. I said ‘when you improve that, I’ll implement cervical screening.’’ New policies, money and delivery: DOTS One of the new policies which was frequently mentioned was DOTS: Direct Observed Treatment Short-course strategy for tuberculosis. A local authority person reported: ‘We’re doing 50 a week but can’t do a full investigation or break the cycle because of staff shortage… We could train people with matric but we’re not allowed to employ people… People who do DOTS work want money. SANTA is saying they’ll give T-shirts and lunch packs but this is not enough… They haven’t got jobs. It’s all money related.’ Other interviewees spoke of similar money constraints. One suggested paying the DOTS supervisor for every person cured or treatment completed. Another described the ‘children who volunteered’ as ‘hungry and unemployed.’ A local authority clinic had stopped doing DOTS ‘because of shortage of manpower because I’m alone since this millennium.’ Sometimes the money obstacle has been overcome. One region described how they planned training sessions but had to cancel at the last minute when Santa, the proposed trainers, phoned to say that the province was reconsidering its contract with them. The region was understandably upset as such an experience ‘upsets the community, they lose their confidence in you.’ Nevertheless, the region persevered and is now using local government councillors instead: ‘They’re paid and keen to be reelected. What better way to prove you’re concerned about your community that to be seen to be helping the sick?’ . 34 2.3.3 Local primary health care services KEY ISSUES There are big differences between and within provinces in respect of functional integration at clinic level In most provinces, local authority clinics are subsidised by province. In some cases location of provincial staff within clinics causes tensions over authority and accountability Provision of PHC services by province and local authority can confuse users The intention of the government is to provide integrated and comprehensive care at primary level. One aspect of integration is that service users must be able to get all their service needs met in one place at one time. This is a critical gender issue, since the vast majority of service users are women, and many of them need not only reproductive and other services for themselves, but also services for their children. Having all services available on one day saves women time and the money required for transport to clinics. It also prevents their losing money from wages or selfemployment. Having one provider meet a range of needs means that they are more likely to provide quality services, and have an understanding of a woman’s health needs as a whole, rather than one provider seeing a woman solely in terms of her contraceptive needs, and another in relation to a health problem. Integrated services are not always available even in the big cities When the National Association of Democratic Lawyers (NADEL) looked at women’s access to health care services, they found three clinics in Cape Town which each had very different levels of integration (Govender, 1999:16-7): The Western Cape province established the Michael Mapongwana Community Health Centre in Khayelitsha in 1996. Because it was created so recently, it provides a full package of preventive and curative primary health care services. However, the Maternity Obstetrics Unit is the only section that is open 24 hours a day. The Khayelitsha Clinic is run by the Tygerberg municipality. It shares a building with the Khayelitsha Community Health Centre and Maternity Obstetrics Unit which is run by the province. The clinic provides child health services, TB curative services, and family planning. It is open only during working hours. Manenberg Clinic falls under Cape Town municipality. It provides preventative and curative primary health care services, but does not have a full range of services. For example, the Clinic offers postnatal services, but not antenatal. The clinic is open only during working hours. One of the factors working against integration is that some services are provided by province and others by local authorities. A nurse at clinic level running a local authority service spoke about the problems that arise: ‘I do preventive. The [provincial] health centre does curative… I transfer people there – just 100 yards from where I’m working…We used to take maternity but there’s a problem because of financial problems so we refer to the health centre for delivery… I first send them to the health centre for booking, then they come back to me for general examination, observations and everything. Then when due they go to the health centre for delivery’. 35 Regarding sexually transmitted diseases, the sister said, ‘I do see patients and defaulters, then I send them back to the health centres to be seen by doctors… Minor STDs I do treat here. If I fail then I send to the health centre.’ Provinces and local authorities have developed different solutions in attempting to provide comprehensive care. Some reported that there are few problems and good cooperation. For example, a Northern Province local government official reported that there is ‘very good relationship. We liaise a lot… Any time they want to do anything, they consult with that.’ The regional office concerned reported that a few local authorities were not yet offering health services, but that the province was supplementing in all areas because the existing services were not adequate: ‘We are still in separate clinics but we meet, discuss, talk. We involve them in in-service training, in all the changes. We give them the health policies, whatever… It’s going well.’ On the other hand, the same regional manager noted resistance to actual integration: ‘We did try but we found that there was resistance from their side.’ One local authority manager described particularly far-reaching efforts at integration. The district has a health team which includes facility managers and which meets monthly to discuss implementation and share resources. Overall there are 20 provincial and 57 local government services, but the province employs 77% of the staff. The manager was proud to report that they had ‘come a long way. We don’t have a dichotomy of local government working in their own paradigm and province working in their own paradigm… In the past province only provided curative and local government your preventive/promotive. Now we’ve taken on curative in 56% of our facilities and province have taken on some preventive services and we also have a skills mix… We also run joint training programmes… When we drew up this action plan people focused on the issues… so people forgot about who has what conditions of service.’ Other informants described a range of difficulties which undermine integrated services provision. A provincial programme manager described the problem related to local and provincial staff having their own reporting structures, ‘So you can’t force them to do things if their seniors don’t see it as a priority… There are areas… where the clinics are working together… but you’re still separate. You still account to whoever you account to… so you still encounter questions like ‘whose budget is it’?’ A regional manager said the situation had improved but that there were still tensions because the local authority staff had been given supervisory posts and subsidised vehicles and tended to blame provincial staff when there were any problems. Many interviewees also described how incomplete integration of provincial and local staff caused tensions or ‘head butting’ between employees. Several referred to the fact that local salaries and conditions of work were often better. These issues are discussed in more detail below. 2.3.4 Reliance on other government departments KEY ISSUES Reliance on other sectors for basic services can be inefficient 36 Implementation is sometimes hindered by the division of responsibilities between sectors. Transport provides a good example. Some places have found good working solutions for transport. One region said that they had taken over all their transport needs: ‘We run the whole ambulance fleet, all the mobile services, everything. We took over running the vehicles from the department of transport. They‘ve done decentralisation hard here.’ In another province, transport remains in the hands of the Transport Department. One informant said that there is a well-coordinated system between the two departments which has also decreased theft of vehicles. However, in the same province a regional manager said that when vehicles were sent to Transport for repairs, ‘they take long to come back.’ Some local authorities described their transport management systems as working well, despite not being managed directly by health. A local authority manager reported that the ‘ admin person takes responsibility for the vehicles. I tell her I need 10 vehicles for World AIDS Day, for example. It works faster than the provincial side.’ But a nurse in charge of a local clinic had a different experience. She said, ‘I don’t have a vehicle – we share with the municipality… Sometimes they don’t turn up. Sometimes they come late and patients have gone.’ Transport is not the only area where delivery is dependent on the political priorities or practical capacity of other departments. As one regional manager noted, ‘Water in our clinics involves another department… We do meet with them to discuss getting water into the clinics. This involves a lot of departments and things are not as fast as that – it’s a stumbling block.’ 2.3.5 Shortage of funds or shortage of staff? KEY ISSUES Shortage of funds is not seen as the biggest barrier to implementation of quality services The pressures of ongoing restructuring together with new policies affects the delivery of quality services Resource shortages are most often expressed in relation to staff workload, but this is often a problem of poor organisation Institutional culture undermines local level initiative and problem solving Planning and priority setting can help to stretch resources Very few informants said that funds were the biggest barrier to the implementation of quality services. The following comment encapsulates the more common response: ‘We are moving too slowly for expectations and much too fast for the capacity of the system to sustain it… Our staff are reeling. I personally think one of the major errors we committed… we focused too much on restructuring and transition and not enough on service.’ Several interviewees pointed out that it was not only health that was restructuring. A district manager explained: ‘Districts involve not only health and welfare, but all departments, to have a ‘supermarket’ – agriculture, health, welfare all there… So that’s the problem, not money.’ 37 Further, while most interviewees said that funds were not the biggest problem, they were clear that more funds would allow better services. As one local manager reported: ‘We’re not doing what we’d like to do – for example we’re servicing informal settlements on a weekly basis. That’s not ideal… Also increased waiting time of patients in facilities’. The most commonly raised issue in relation to funding shortages was staff workload. As a provincial official expressed it: ‘Shortage of funds is shortage of staff. If you don’t have enough manpower [sic] then you don’t get everything done the way it should.’ Others spoke about demands on staff time in relation to training for and implementing policies such as free health care, screening of all patients for STDs or community-based systems for implementing DOTS. A clinic supervisor noted that these ’additional services lowered the morale because a lot of work has to be done .’ Demands on time vary in different areas. In many areas clinics are busy in the mornings, but staff have no work to do in the afternoons. In others the workload is substantial throughout the day. A Northern Cape interviewee said that while in Bloemfontein there are 35 people to see per professional nurse, ‘in our province they have to see 42 per professional nurse but they’re actually seeing between 50 and 55 per day at the moment – we don’t have enough funds to appoint more people’. Research reveals that staff find it easier to assume that the problem is staff time than to analyse how they are spending their time, and whether clinics are organised to make the best use of time and other resources. Khin San Tint of the Women’s Health Project is currently assisting regional and clinic staff in integrating services. She says: ‘Time flow studies show very clearly that there’s no shortage of staff but the utilisation and performance is not according to the standards… In Northern Province there are some very populated districts where you’ll see people are overloaded – one to 90 or one to 60. But in most sites they’re under-utilised.’ Rather than overload, the problem is management and organisational capacity, ‘the ability of people to find alternative ways of doing things.’ Tint notes that the problem results from the hierarchical structure: ‘People feel their supervisors don’t allow them to take initiative. It’s very rigid the way people perform their jobs.’ Government interviewees also pointed to poor organisation, duplication and ineffective functioning. For example, a Northern Province official described how both the departments of health and welfare are working on poverty and nutrition. The budgeted funds come from separate ‘votes’ and they are not able to transfer activities between votes so as to streamline nutrition-related activities. The official said that there is no time to think about and find solutions to such problems, and build a shared vision ‘because we also feel we have to account for a mechanical kind of quantitative productivity on a day to day basis… We actually could be achieving much more if we could organise our time much better and know who would be addressing those demands.’ 2.3.6 Health worker morale and attitudes 38 KEY ISSUES Health worker attitudes were repeatedly cited as the biggest problem undermining the delivery of quality PHC Poor attitudes are frequently ascribed to low health worker morale Initiatives are underway to address this problem but successful interventions are not being institutionalised The majority of interviewees cited health worker attitudes as the biggest problem undermining the ability to deliver quality PHC services. A regional manager reported on complaints from the public: ‘If you’re working in an office of PHC like me you get all these people coming in with their complaints and most of the things are attitudes of the workers.’ A provincial official reported particular instances of poor treatment, such as a youth being chased away from a family planning clinic and routine poor treatment at antenatal clients. An official from another province described an experiment which proved the importance of staff attitudes: ‘There was a clinic which was always full and another maybe seven kilometres from it which was not busy. But patients came from the empty one to the busy one. We took one nurse from the busy clinic and put her in the quiet clinic and that clinic within a short time was busy. So we could see this was an attitudes thing.’ Others had similar stories. A local government official told of a PHC nurse assigned to work alone in a mobile clinic. The nurse saw 70 to 80 patients a day. ‘She has community health workers she has recruited from the community. She’s sent them for HIV counselling training and other training and they work with her and support her in her service… She has patients sitting on the grass to see her, who give her support, for example telling her days not to come because of weather or political tension.’ The word ‘attitude’ suggests that the responsibility lies with the nurses. Other interviewees argued that the problem was health worker morale rather than attitude. For example, a clinic supervisor said that implementing new policies could be difficulty because ‘people are not very happy about change all the time - people fear change.’ The definition of the problem clearly depends on one’s position. A clinic supervisor said she thought the relationship between health workers and clients was ‘healthy. But you should ask what’s the relationship from clients – it varies from individual to individual. Nurses know they should react positively with whatever they get from clients’. Clearly this informant saw users rather than nurses as the problem. However, a local authority manager who was proud of his own staff’s attitudes, said: ‘I don’t have any problems. But we usually get complaints when people come from outside. We ask why don’t you go to your own clinic and they say it’s because people don’t treat them well and don’t have enough stock so they’d rather come here.’ Some interviewees argued that there are concrete reasons why nurses find their position difficult. These reasons cause low morale which, in turn, causes poor relationships with users. Other interviewees were less sympathetic. A regional manager complained: ‘There’s a moral apathy in the country at the moment. A sense of entitlement - why should I work for what I get?’ 39 Other, more specific, causes of poor morale mentioned were the following: Transparency in the restructuring process As part of restructuring, some provinces are cutting posts. A provincial official explained: ‘We’ve got lots of supernumeraries, inherited old staff. And new staff came in so our salary budgets are much more than the money used for service delivery’. Some staff are left wondering when it will be their turn. A provincial official’s comments reflected her sense of devaluation: ‘They mustn’t just cut and say we don’t want you old people. We all have experience… They have been too much in a hurry to cut out the old ones without making sure the new ones have experience and skill.’ A provincial programme manager acknowledged that part of the problem lay with the lack of communication, and that this resulted in uncertainty and rumours: ‘You get corridor gossip that this or that directorate is going to go. If someone would come and tell people that there’s no hidden agenda and spell it out upfront.’ Similarly, a local authority manager noted: ‘Morale is very low. There’s lots of uncertainty… Province wants to take over the service and reorganise it and then put it back to local level. This has created a lot of mistrust and confusion.’ Some of those who argued that health worker morale is the primary problem felt that there has been progress and morale is ‘picking up’. They said that uncertainty and fear was understandable given a new government and many changes. But, as a provincial manager explained, with time, ‘because of the training, capacity building, you see a light getting bigger and bigger in the tunnel until your morale is better.’ Salaries and conditions of service Salaries were mentioned by a number of interviewees as a problem – particularly the salary differentials between local and provincial health workers. The increase in public sector salaries has ameliorated this problem to some extent and some, such as this local government manager, argue that it is overstated: ‘In Durban a huge clinic had been functioning for 18 months with all staff under the same roof. It appeared to work far better than senior people thought… Sometimes we don’t give staff enough credit.’ Nevertheless, our interviews also revealed ongoing unhappiness. A clinic sister was frank about her fears: ‘I’m afraid of the new policy. At present I’m from a government [provincial] hospital. …When I came back to the municipality they took my pension for a year. …When I think of going back to government again it will be a problem for my pension.’ Similarly, a local government manager spoke about a R3 000 difference in monthly pay between a nurse working in Ennerdale and one working in Soweto, with further differences in uniform and other costs. The manager said that they were unable to achieve parity ‘because unions come to the bargaining council’. Some respondents identified low salaries, rather than differentials, as the barrier. A provincial official said: ‘Now there’s a shortage of trained nurses. They are taking packages. They go outside the country to Saudi Arabia, to England… Hard working people are not getting any incentive and a person will say ‘I’m 20 years but there’s no promotion, no extra money, no night duty allowance.’’ A regional manager from the 40 same province noted that nurses are drawn to the private sector where salaries are more attractive. Pace of change and workload In some cases, low morale was ascribed to workload in the context of political change, with resultant burnout. Change was said to be particularly difficult for older staff who had been operating in a particular way for decades. Their unhappiness demoralised younger staff ‘ who have innovative ideas and find the older group don’t want to change.’ Lack of support for nurses Some interviewees suggested that staff had little sense of being valued or appreciated, whether by their seniors or the public. As one regional manager explained: ‘Our people are overworked. Next thing the MEC wants a 24-hour service for Batho Pele and people feel they can’t cope with that as well. The public are demanding. They don’t come back and say thank you for the service. Nursing staff also have human rights. The public expect too much.’ There do not appear to be any fully institutionalised efforts to address health worker morale. In one province informants spoke of the implementation of Batho Pele as an enhancement of a ‘why’s’ programme that had been running to promote quality services. However, at regional level, officials were not really aware of this initiative. An intervention mentioned by all provinces is the Health Workers for Change (HWFC) series of workshops (Fonn and Xaba, 1995). This is a change-management methodology which draws out three skills – identifying health system problems; identifying the causes and impact of gender inequality on the health system, health workers and clients; and learning to solve problems collectively. HWFC was developed in South Africa by the Women’s Health Project, and has been shown here and elsewhere to have a positive effect on health worker morale and attitudes as well as on health system functioning. The efficacy of the programme was acknowledge by interviewees. A provincial manager reported that where staff had undergone HWFC training, they ‘feel that they’re contributing something despite that they may not be getting the necessary support which they need from the province.’ Nevertheless, in no cases is the method being used systematically or province-wide. Another donor-funded NGO initiative in the Northern Province, called the Community Responsiveness Project, is successfully training people on how to be responsive and to link with councillors, traditional leaders and other community members. Here too, there are no plans for institutionalisation. A number of other steps were mentioned. In Gauteng there is the Khanyisa award to reward the best unit and individual. At district level Gauteng has annual research conferences which encourage interest in work and reportedly generate some excitement. A manager in Northern Cape Province said that they try to bring in community participation and ‘being nice to clients’ as an ‘ongoing chant’. Local authority informants spoke of similar initiatives to encourage interest in work and good relationships. 41 2.3.7 Where is health promotion? KEY ISSUES Health promotion and community outreach are first to be dropped when there are resource shortages Clinical services always get priority over outreach Health promotion requires managers to move away from the medical paradigm in which they are trained The White Paper is very clear about moving from a curative to a preventative approach. The Paper emphasises health promotion as an important part of this. However, community outreach appears to be low on the agenda. It is not necessarily considered central to the job of health providers, and is amongst the first things to go when funds are short. Thus a provincial manager said that ‘to even think about community-based activities from the health budget is difficult… in terms of essential provision when we have to cut, such programmes would be the first to cut from, even if there has been approval… We survive on donor funding to be able to provide such services. There’s also a budget from national… but the magnitude of the problem… makes the budget approved by national insufficient.’ A few interviewees argued that the neglect reflected not simply fund shortages, but a deeper failure to move away from the traditional medical model of health. One provincial manager said: ‘Health promotion isn’t health education… I think we miss the opportunity of impacting in a great way on the health of the people and using our budget effectively by not really understanding.’ However, few interviewees took this broader approach. For example, when asked to what extent AIDS is given priority, or about implementation of a DOTS approach to TB, lack of staff capacity to do outreach was repeatedly mentioned. On the question of responsibility for building community understanding on STDs, one local authority clinic supervisor noted that ‘It is our business but there’s a staff shortage so we can only focus on those who come into the clinic and give talks, but with the added workload it’s a problem.’ A local authority official described how they manage the local ATTIC on behalf of the province. The province is meant to provide a 100% subsidy, but seldom pays it. The ATTIC office is responsible for the entire province, but has only two staff. If they are out of the office, there is no-one in the office to help people who come for information. With the ongoing lack of subsidy, the local authority has now cut the travel allowance ‘so that he can’t go around and do proper training any more.’ A clinic sister in a provincial facility gave the example of clinics giving women drugs to treat their partners for STDs, without ever seeing the partners. She said that they do not have capacity for the community outreach required to build people’s willingness to attend a clinic on the request of their partners. In addition, many husbands are migrant workers, and cannot access the clinic since it is closed on weekends. The current strategy presumes that women will be able to talk to their partners about STDs and that, should they broach the subject, their partners won’t assault them or accuse them of promiscuity. 42 Policy-makers are aware of the neglect of health promotion and are attempting to include it in the PHC package currently being costed. However, ‘in workshopping the package many nurses (in particular) said that they would not have time to do much of this.’ This response reinforces the fact that money alone will not resolve the problem. Further, exact costing is difficult if not impossible. As a provincial manager explained: ‘It’s difficult to cost it because some PHC services are not health-specific in the medical sense of the definition of health… In the minds of many people when you talk about health services you’re talking about tablets and institutions… However, there may be programmes that are necessary to intervene at the levels below those of addressing the symptoms.’ 3 CONCLUSIONS The interviews quoted above give a feel for the experience of health officials who are involved at different points of the policy-making and implementation process. A report based on people’s experiences can be seen as biased because each person’s own interests will influence what they say. But that is one of the important things that this research can teach us. The way institutions work will affect delivery, and that is part of what this study looks at. But, on top of that, institutions are made up of people and relationships. How those people understand the process of change will influence the way in which policies are made, implemented or ignored. The quality of relationships within institutions will likewise directly affect implementation The fear of job losses also influences people’s perceptions. Many people in both provincial and local government posts are worried about what will happen to them when integrated districts get off the ground, especially if their employer changes. Those in larger urban municipalities are currently relatively well paid and secure and fear that this will change. Those in smaller municipalities fear being taken over by province, demoted or even retrenched. This section summarises some of the lessons we can learn from the interviewees. A strong message from these interviews is that there is ‘transformation overload’. Many informants feel that ‘change has been too big, too huge, too fast, too wide’. A key issue is the difficulty of balancing the overall restructuring and transformation processes with the need to implement rapidly a wide array of new policies. Many people report that policy-makers often fail to consider the resource requirements for implementation. These resources may take the form of money, skills, facilities or management. Most people in regions, districts and local government feel disempowered when it comes to national or provincial policy making and implementing the policies. All but the most senior provincial officials feel disempowered in relation to decisions about budgets. For the most part people seem to be excluded for structural and logistical reasons, rather than because those at the top want to maintain their power and 43 control. Changes here must fight against long-standing bureaucratic rules and ways of working. Transformation will not happen if it is seen as simply a technical change, which focuses only on systems and structures. Systems and structures are made up of people, and these people need to change the ways in which they think, act and interact. The interviews show there are still fairly widespread problems of lack of communication and mistrust. Health worker morale and attitudes are a significant impediment to quality health services. The front-line staff who provide all the new services need to feel cared for and supported. They need to feel that they can influence decisions in some way. Only then will they feel inclined to address the needs of those they serve in a caring way. Another major obstacle to improved health service delivery is the lack of a coherent human resource strategy. This contributes to shortages of certain categories of staff, uncoordinated training programs and associated inability to redistribute staff between types of health facilities and geographic areas. One of the results is morale problems because of excessive workload in certain facilities. Some health services are faced with absolute financial (and other) resource constraints. Provinces which are largely rural and incorporate the former homelands have health expenditure levels which are well below the national average. The implementation of new policies in these provinces is particularly difficult. Some local government health services face increasing uncertainties over resource availability, particularly where they are heavily dependent on provincial subsidies. However, many interviewees – and the politicians who were not interviewed – are quicker to talk about the extra resources that are needed, and slower to talk about what can be cut. There is not enough acknowledgment that the size of the cake is relatively fixed, and that to get more for one purpose or area there needs to be less spent on something else. Even where there is recognition of resource constraints, it has proved extremely difficult to reallocate resources from hospitals, particularly the more specialist hospitals, to fund improved primary care services. It has also been difficult to reorganise local level services so as to deliver better quality services more efficiently. Resource allocation and budgeting processes are still highly centralised. This is partly due to lack of financial management capacity at lower levels. But the financial management systems exacerbate the problem because they do not usually provide the necessary information. Many health managers do not have a good understanding of budget-making principles. Regional, district and health programme managers do not understand the purpose of guideline allocations. They do not always have a good understanding of the equity considerations which determine, firstly, how much they get and, secondly, which should influence how they distribute what they get. 44 Officials are often told that they must make decisions about budgets which, in fact, can only be changed at the margins because of all the fixed costs. The enormity of considering the whole budget makes the task more complicated. A more sensible approach may be to tell officials which part of the budget can feasibly be changed. This would cut down on the size of their task, and make their decisions less easy to ignore. Figure 1 summarises what could be a better way of making decisions about budgets, from an equity perspective. It suggests, that guideline allocations from the province would be based on equity targets derived from a needs-based formula. These could then be modified after consideration of locally developed plans and budgets. 4 Figure 1: Suggested resource allocation decision-making process ACTION Provincial level 1. Determine guideline allocations to regions based on comparison of needs-based formula targets with current expenditure, and inform regions. 3. Negotiate with regions, based on needs-based formula targets (equity objective) and regional plans and budgets. 4. Make final allocation decision, and inform regions. Provincial 1 2 3 Region 4 5 Regional level 2. Undertake detailed planning and budgeting within context of guideline allocation. Present these to province. 3. Negotiate with province for adequate allocation to implement plans. 5. Finalise regional plan and budget based on allocation. Most interviewees are committed to the idea of a district health system, based in local government. Good cooperation between local government and provincial health departments seems to occur mainly where local government has well established health services funded largely through own revenue, i.e. where they are not heavily dependant on provincial subsidies. The issue of control over resources is a major impediment to a ‘partnership’ approach. There is great uncertainty in local governments about provincial subsidies and how the decisions about them are made. There are also multiple, and in some cases conflicting, lines of accountability for local government health departments due to multiple funding sources. There is an ongoing tension between restructuring for integrated delivery of services at primary level on the one hand, and introduction of new programmes 45 on the other. The system of integrated regional budgeting, for example, does not fit easily with having separate programmes which require designated funds for specific activities. Clinical services always get priority over health promotion and community participation. At times the reason is given as funding shortages – not having enough staff to move into communities. But it also reflects the overall orientation of the health system. 4.1 CONCLUDING COMMENTS The entire health system is engaged in a process of fundamental restructuring. There are, inevitably, difficulties. Some of these are being recognised and addressed as lessons are learnt. The areas of policy change and implementation which are structural and relatively technical, such as financial planning or restructuring into districts, appear to receive greater recognition than the ‘softer’ questions. The latter include health worker buy-in to the change process, health worker responsiveness to clients, and capacity for health promotion. These areas need serious consideration if we want equity in the provision of high quality services to women, men, adolescents and children. Many, if not all, of the observations and recommendations above are incorporated in the Health Sector Strategic Framework for 1999-2004 produced by the national Department of Health in 1999. This document includes the following in the Department’s ten-point plan: ‘Legislative reform; Improving quality of care; Speeding up delivery of an essential package of services through the district health system; Decreasing morbidity and mortality rates through strategic interventions; Improving resource mobilisation and the management of resources without neglecting the attainment of equity in resource allocation; Improving human resource development and management; Improving communication and consultation within the health system and between the health system and the communities we serve; and Strengthening cooperation with our partners internationally.’ (Department of Health, 1999:12). The challenge now for the national, provincial and local departments of health is to implement this plan taking into consideration the difficulties experienced in implementing previous policy proposals. 5 5.1 PART 4: REFERENCES AND ANNEXES REFERENCES Brijlal V, Gilson L, Makan B, McIntyre D (1997). District financing in support of equity: Tender Contract to provide technical assistance to provinces with obtaining equity in district financing. Report submitted to the national Department of Health. 46 Johannesburg: Centre for Health Policy, University of the Witwatersrand and Health Economics Unit, University of Cape Town. Budlender D (1999). ‘Women and the Local Government Budget’ in D Budlender (ed). The Fourth Women’s Budget. Cape Town: Idasa. Department of Health (1997). White Paper for the Transformation of the Health System in South Africa. Pretoria: Government Printer. Department of Health (1998). Saving Mothers: Report on Confidential Enquiries into Maternal Deaths in South Africa 1998. Pretoria: Department of Health. Department of Health (1999). Health Sector Strategic Framework 1999–2004. Pretoria, Department of Health. Fonn S and Xaba M (1995). Health Workers for Change: a Manual to Improve Quality of Care, Geneva: UNDP/World Bank/World Health Organization Special Program for Research and Training in Tropical Diseases and Women’s Health Project. Fonn S, Xaba M, Tint KS, Conco D, Varkey SJ (1998a). Maternal health services in South Africa: During the 10th anniversary of the WHO ‘Safe Motherhood’ initiative, South African Medical Journal, 88: 697-702. Fonn S, Xaba M, Tint KS, Conco D, Varkey SJ (1998b). Reproductive health services from rhetoric to implementation: South African experience, Reproductive Health Matters, 6(11): 22-32. Friedman M (1999) ‘Effecting equality: translating commitment into policy and practice’. Agenda: Translating Commitment into Policy and Practice? Special Education:2-17. Gilson L, Doherty J, McIntyre D, Thomas S, Brijlal V, Bowa C & Mbatsha S (1999) The Dynamics of Policy Change: Health Care Financing in South Africa, 1994-99. Monograph No. 66, Johannesburg, Centre for Health Policy, University of Witwatersrand/ Cape Town, Health Economics Unit, University of Cape Town. Govender P (1999) Women’s access to health care services in the Western Cape. Research Report No 5. Cape Town: National Association of Democratic Lawyers. Klugman B (1999). Mainstreaming gender equality in health policy, Agenda: Translating Commitment into Policy and Practice?, Special Edition: 48-70. Klugman B (2000). Empowering women through the policy process: the making of health policy in South Africa. In Presser H and Sen G (eds.) Women's Empowerment and Demographic Processes: Moving Beyond.Cairo, Oxford University Press, forthcoming. McIntyre D, Bloom G, Doherty J, Brijlal P (1995). Health expenditure and finance in South Africa. Durban: Health Systems Trust and World Bank. 47 McIntyre D, Thomas S, Mbatsha S, Baba L (1999). Equity in public sector health care financing and expenditure in South Africa. In: Ntuli A (ed.). South African Health Review 1999. Durban: Health Systems Trust. Power D and Robbins D (1996). Organisation and Management: Public Sector. In: Health Systems Trust (1996). South African Health Review, 1996. Durban: Health Systems Trust and the Henry J. Kaiser Family Foundation. Statistics South Africa (1998). The people of South Africa. Population Census, 1996. Census in Brief. Report No. 1: 03-01-11 [1996]. Pretoria: Statistics South Africa. Stevens M (1997) ‘Health’ in D Budlender (ed) The Second Women’s Budget. Cape Town: Institute for Democracy in South Africa:286-313. Stevens, M (1998) Factors impacting on the development of a pregnancy termination Bill. Masters of Management, Faculty of Management, University of the Witwatersrand. Tollman S, Rispel L (1995). Organisation, planning and management. In: Health Systems Trust (1995). South African Health Review, 1995. Durban: Health Systems Trust and the Henry J. Kaiser Family Foundation. Walt G and Gilson L (1994) ‘Reforming the health sector: the central role of policy analysis’ in Health Policy and Planning 9(4): 353-370. 5.2 ANNEX 1: PEOPLE INTERVIEWED Seokemong Absalom, Clinic supervisor, Galeshewe, Northern Cape Nafiesa Akharwaray, Deputy Director Financial management, Northern Cape Mr AJ Britz, Acting Chief: Health Services, Kimberley Local Council, Northern Cape Mr Buchanan, Acting Manager of Environmental Health Services, Kimberley Local Council, Northern Cape Elias Chokoe, Acting head of health care services, Chief Pharmacist, Moletji Matlala District, Northern Province Baski Desai, Specialist Post in Chief Directorate District Health Services, Gauteng Yvonne Holden, Sister in charge of Kuruman clinic, Northern Cape Mariana Loots, Assistant Director Diamond Fields Region, Northern Cape Marian Loveday, Regional health manager, Northern Cape Essina Mabitsela, Deputy Director Mother, child, women’s health, reproductive health and genetics, Northern Province Carvie Madikane, Deputy Director Maternal child and women’s health, Northern Cape Hlamalali Nellie Manzini, Regional Director, Central Region, Northern Province Carol Marshall, Chief Director Strategic Development, Gauteng Natalie Mayet, Executive Officer for Commmunity Health, South Local Council, Gauteng Rose Mazibuko, Chief Director PHC, Northern Province 48 Dr Mjekevu, Head of Department for Health, Kempton Park Tembisa Metropolitan Local Council, Gauteng and representative of SALGA to national department of health District Health System Task Team. Greg Munroe, Executive Director, Community Services, South peninsula municipality, Western Cape and SALGA representative on National Department of Health Provincial Health Restructuring Committee Lydia Ndhliwayo, sister, Messina local authority clinic, Northern Province M J Netshilindi, Deputy director PHC, Northern Region, Northern Province Yogan Pillay, past Director: Policy Analysis and Planning Unit, National Department of Health; now Deputy Director: National Expansion, the Equity Project Phillip Rousseau, Chief Health Services, Messina Transitional Local Council, Northern Province Mmipe Saasa-Modise, Director Mother, child health and nutrition, Gauteng Doreen Senokoane, Deputy Director Reproductive health, Gauteng Johan Swanepoel, Head of Community Health Services, Pietersburg Transitional Local Council, Northern Province Alex van den Heever, Financial manager, Gauteng 49