Guide to the Site Selection Process
advertisement

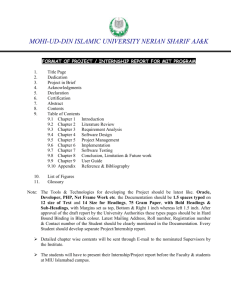
Guide to the Clinical Selections Process Nancy K. Erikson, PT, MS Director of Clinical Education Susan M. Parisot, PT, DPT, GCS Assistant Director of Clinical Education Doctor of Physical Therapy Program Eastern Washington University 2005, revised 2006, revised 2007, revised 2008 PURPOSE OF THIS GUIDE This Guide is intended to give Doctor of Physical Therapy (DPT) students an overview of the policies and procedures for selections of the clinical internships they will complete during the Program. The information in this Guide will: outline the curricular requirements of the clinical education component of the Program. inform students about clinical experiences available. clarify the roles and responsibilities of the student, the Director of Clinical Education (DCE), the Assistant Director of Clinical Education and the Clinical Education Program Assistant in the selections process. After reading this Guide, students will: be prepared to make informed choices about their clinical education in consultation with the DCE and Assistant DCE. have realistic expectations about the clinical selections process. This Guide is not intended to provide all the information needed by the students about the clinical education component of the Program. The Student Handbook provides specific information about the content, policies and procedures of the clinical education courses. This Guide addresses the clinical selections procedure. Students are encouraged to share the information in this Guide with members of their support system, including family, significant others and friends. The Guide highlights the personal and financial expectations and demands of the clinical component of the Program as related to the clinical selections process. The Guide was developed in 2005 by Nancy K. Erikson, PT, MS, DCE and Mellissa Thoreson, Clinical Education Program Assistant in consultation with Mary Weddle, PT, DSC, ACCE from St. Catherine’s College, Minneapolis, MN. It was reviewed by the following students: Patrick Bears, Rhiannon Braun, Jamie Rodgers, Charlie Howlett, and Elaina Erickson from the Class of 2007 and Tara Johnston, Cheryl Rudd, Ryan Myhre, Rebecca Cheney and Jamie Bean from the Class of 2006. Multiple students from the Classes of 2006 and 2007 contributed to the section on Facility Types. CONSIDERATIONS IN THE PLACEMENT PROCESS 2 The mission of the Department of Physical Therapy, Eastern Washington University, is to graduate an entry-level physical therapist. Our purpose is to prepare a generalist physical therapist who is capable of practicing and providing service in any setting and to any patient population. To this end, we encourage the widest possible exposure to a variety of practice settings throughout a student’s clinical education. INTERNSHIP EXPERIENCES The five (5) week internship may be completed in any available setting. The three ten (10) week internships: Students are required to complete one ten (10) week internship in a rehabilitation setting. This can be in an adult or pediatric inpatient rehabilitation facility, a subacute unit, a skilled nursing facility, an outpatient setting (i.e.: outpatient neurologic clinic, outpatient pediatric clinic, school system) or home health setting. To qualify as a rehabilitation setting, the majority of the patients must have neurologic diagnoses and the staff must include physical therapists, occupational therapists, speech language pathologists and other health care providers (social workers, nurses, physicians, dieticians and/or others) working in a collaborative or team format. Students are required to complete one ten (10) week internship in an acute care setting. This is a hospital setting that may include adults and/or children. Students are required to complete one ten (10) week internship in a setting of choice. Options may include an outpatient orthopedic clinic, an inpatient rehabilitation unit, an outpatient neurologic clinic, a subacute unit, an ambulatory outpatient unit, an acute care hospital, a skilled nursing facility, home health, an acute pediatric facility, an outpatient pediatric clinic or a school system. There are some sites that provide a combination of experiences during the ten (10) week internship. Examples include rural facilities where the physical therapists see patients in acute care, the outpatient clinic and the school system or home environment routinely. In these instances, the primary emphasis of the internship is based upon where the majority of the student’s experience will be as determined by the Director of Clinical Education, in consideration of the student’s entire Clinical Education program. The ten (10) week internships do not require any specific sequencing. SPECIAL NEEDS OF STUDENTS In some circumstances, a student may have a special need arise, educational or otherwise, that requires individual consideration in the placement process. Such accommodations must be arranged with the DCE and/or Assistant DCE. 3 The role of the DCE and Assistant DCE is to make the best possible match between available internship sites and the student’s educational needs and interests. Where and when possible, personal considerations will also be accommodated but not at the expense of providing a well-rounded educational experience. Clinical assignments are arranged through a mutual decisioning authority in order to best meet the educational goals of the Program. SITE DEVELOPMENT AND PROGRAM CONCERNS It is the responsibility of the DCE and Assistant DCE to utilize the clinical sites of the Program in an efficient manner, assuring the continued participation and development of the facilities contracted. New clinical internship sites are opened only when the DCE and/or Assistant DCE see a need for additional sites in a specific area of practice due to closure of previous sites, changes in staffing patterns limiting the number of students or other reasons affecting the clinical education component of the Program. Internship sites are selected in geographical clusters in the Northwest. This enables the DCE and/or Assistant DCE to visit the sites economically, provide professional development to the staff and provide on site student support when needed. The student will have an opportunity for input regarding choices of clinical internship sites, however all final decisions regarding placements are the responsibility of the DCE and/or Assistant DCE. The Program maintains over 200 contracts with clinical sites with about one-half of these sites used on a regular basis. In order to assure that students have good quality clinical experiences, the Program has adopted the policy of regularly utilizing those clinical sites that have consistently provided students with good learning experiences. The Program faculty believe that when clinical sites are used regularly by EWU students, the clinical instructors at those sites become more familiar with the Program and curriculum. Also, those sites tend to develop a commitment to continue providing clinical education experiences for the Program, year after year. Clinical internship sites are located in Alaska, California, Colorado, Georgia, Hawaii, Idaho, Minnesota, Montana, Nebraska, Nevada, Oregon, Texas, Utah, Washington, Wisconsin and Wyoming. The majority of sites are in the Pacific Northwest. Each March following the American Physical Therapy Association’s uniform selection protocol, the DCE and Assistant DCE request internship slots or positions for EWU students for the next calendar year. The number, location and variety of positions available vary from year to year depending upon staffing, numbers of students accepted and changes at the specific facility. Clinical Internship Selection Policies A student will not be placed at a facility in which the student has worked or volunteered in the physical therapy department or in a physical therapy related area within the last 3 years. A student will not be placed at a facility in which the student has been or is currently being treated as a patient in the physical therapy department or in a physical therapy related area. The Program believes that it may be more difficult for students to establish themselves as a student professional in such a setting, since former colleagues and therapists may continue to interact with the student within the context of the previously established roles. These roles may now be inappropriate for the student and may curtail the 4 student’s ability to develop the professional behaviors and relationships essential to success as a student physical therapist. A student will not be placed in a clinical internship at a facility that is funding a portion or all of the student’s education in the Program and/or has hired him/her to begin employment upon completion of the Program. In this situation, the funding and/or hiring arrangement presents a conflict of interest for the facility, the Clinical Instructor, the employer, the student and the Program. Upon entrance into the Program or if the situation occurs during the Program, a student who is receiving financial support from a facility with the expectation of becoming employed upon successful completion of the Program is required to disclose this arrangement in writing to the DCE. This policy does not prohibit students from accepting positions at facilities where they are currently doing an internship or have previously done an internship. The student may request not to be placed at a specific facility. There may be a number of acceptable reasons for this request. Eastern Washington University and the parties it contracts with shall not discriminate on the basis of race, color, creed, religion, national origin, sex, sexual orientation, age, martial status, disability, or status as a disabled veteran or Vietnam era veteran. This policy applies to all EWU programs and facilities and any person or agency entering into an agreement with EWU. EWU and its contracting parties will comply with all laws, state and federal pertaining to discrimination. STUDENT PREFERENCES OF SPECIFIC SITES Students have the opportunity to share their preference for specific site assignments from a list of sites available for each clinical internship. Student input is shared in writing. The number of choices requested from the student changes dependent upon the pool of available sites for a specific internship. Students have the opportunity to meet with the DCE and/or Assistant DCE as frequently as needed during the selections process. However, it is not possible to accommodate the preferences of all students for all clinical internships. FACILITY TYPES The clinical sites available to students have been grouped into types described below. The vast majority of the facilities utilized as clinical sites will generally fit into one of these descriptions. GENERAL PRACTICE General Practice: Typically, a general practice site will be a small rural hospital with 20–30 inpatient beds. Outpatient service is usually large (may be up to 80% of the PT service); other areas may include acute care, long-term care, home care, industrial and pediatrics. Pediatric clients may be served in the clinic, in schools, in institutions or in their homes. The amount of time students spend in each setting will vary, depending on staffing and size of caseloads. ORTHOPAEDIC Orthopaedic: The orthopaedic outpatient clinic may be a free-standing clinic, 5 a clinic within a hospital, or a hospital satellite clinic (affiliated with a hospital but not located within the hospital). Caseloads will primarily be adult general orthopaedic cases. A few clinics are involved with sports medicine. At these clinics, 10-25% of the patient caseload may be classified as sports injuries and the clinic may employ athletic trainers. The percentage of sports injuries seen will fluctuate, depending on the season. The remainder of the caseload will be general orthopaedics, as described above. Note: the names of many outpatient clinics include the words “sports medicine”: This does not mean that the clinic specializes in sports medicine exclusively, nor does it mean that these clinics serve a large number of patients with sports injuries. In actuality, the caseload may indeed be general orthopaedics. From the Class of 2007: Some clinics offer specialty services, such as work hardening, hand clinic, women’s health or lymphedema treatment. In some clinics, you will work very closely with other professions – occupational therapy and speech language pathology. Strategies to prepare for an internship in this setting: Demonstrate a strong knowledge of anatomy and biomechanics. Practice your examination skills, including special tests. Practice palpation skills, especially on the spine. Research your specific internship facility – find out the number of patients per day, the most common diagnoses, and the average age of the patients. This information can be found in the Clinical Site Information Form in the clinical education file cabinets. Review the most common diagnoses, including assessment and treatment. Practice the skills needed for assessment and treatment of patients with the most common diagnoses. Recommended resource: Clinical Orthopaedic Rehabilitation, Wilk and Brotzman. Review the scan examinations taught in class. Design a form to use during examination (i.e., flow sheet) to minimize patient movements. Review joint mobilizations and capsular patterns. REHABILITATION There are three types of rehabilitation sites: the inpatient rehabilitation unit, the outpatient rehabilitation clinic and subacute/skilled nursing facility. Patients will include those with neurologic, orthopedic, cardiac and general medical diagnoses. The proportion and type of neurological diagnoses seen will vary depending on the specific facility. For example, patients with a spinal cord injury are routinely seen in only a few of the rehabilitation sites. Patients who have had strokes or hip replacement surgeries are seen more routinely. INPATIENT REHABILITATION UNITS: Inpatient rehab units are usually found only in large, metropolitan hospitals. Caseload consists of adult and/or pediatric patients who are generally seen twice a day by the PT. Patients will also be seen by the Occupational Therapist (OT), speech therapists, social worker or other rehab professionals. Working as part of this rehab team and participating in rehab “rounds” is an important aspect of this learning experience. Length of stay for patients varies, but typically may be anywhere from 1-8 weeks. Discharge is usually to home, perhaps with supportive services. From the Class of 2006: This is a setting where patients receive daily intensive therapy to prepare for discharge home or to another facility. Patients frequently come from an acute care hospital and receive 3 hours of therapy (physical therapy, occupational therapy and speech) per day in rehab. Common diagnoses include stroke, traumatic brain injury, spinal cord injury, post surgery such as total hip or total knee arthoplasty or cardiac diseases. Physical therapists provide caregiver training and do home evaluations. 6 From the Class of 2007: Patient caseloads can vary from 100% neurological conditions (stroke, spinal cord injury, etc.) to post-operative orthopaedic rehabilitation and conditioning. Strategies to prepare for an internship in this setting: Review neuromuscular academics. Be flexible. Work on observation skills. Be creative with interventions. Practice communicating in layman’s terms. Review treatment strategies for patients with cognitive impairments. Organize your neurological assessment and be ready to perform it. OUTPATIENT REHABILITATION CLINICS: Outpatient rehab clinics are usually associated with a large hospital facility. The clinic may be in the hospital or located off-site. Caseload consists of adult and/or pediatric patients who are generally seen two to three times per week by the PT. Patients may also be seen by the occupational therapist (OT), speech therapist or other rehab professionals. From the Class of 2006: This is a setting where patients come for a multidisciplinary approach to rehab. Common diagnoses include stroke, traumatic brain injury and other neurologic diseases. Strategies to prepare for an internship in this setting: Review neurologic academics. Be flexible. Work on observation skills. Be creative with interventions. Practice communicating in layman’s terms. SUBACUTE /SKILLED NURSING FACILITY: Subacute (or transitional care) units are usually located in skilled nursing facilities (SNF). A proportion of the beds in the SNF may provide residential nursing care as well. Approximately 70-80% of the patients seen in PT will be from the subacute unit of the facility. Patients may have a variety of diagnoses, including neurologic, orthopaedic, cardiac or general medical. Multiple system medical involvement is common. Most likely, these patients will also be seen by the occupational therapists, speech therapists, social worker or other rehab professionals. Working as part of this rehab team and participating in rehab “rounds” is an important aspect of this learning experience. In subacute units, the majority of the patients return to home in 2-8 weeks; others may be transferred to a type of supported living or skilled nursing facility. Patients seen will be primarily geriatric. From the Class of 2006: Patients in a Skilled Nursing Facility are usually patients who have been discharged from a hospital but are not able to return home because they require physical therapy, occupational therapy and/or speech therapy or have continued nursing needs. Some patients will leave once they meet their rehab goals and others will remain long-term residents. Students will see a wide variety of diagnoses from all systems. There are many opportunities to observe and participate with other disciplines, including occupational therapy, speech, home health, social workers, dieticians, physicians, 7 administrators and nursing. Physical therapy includes therapeutic exercise, gait training, bed mobility, transfer training and balance training. Physical therapy is usually done five times a week or more. Physical therapists do family training, discharge planning, safety evaluations and order equipment. Strategies to prepare for an internship in this setting: Review total hip and total knee post-operative precautions. Practice transfers, gait training, bed mobility and balance training techniques. Know indications/contraindications for therapeutic exercise. Know medical precautions to exercise. Think creatively, be flexible and patient. Develop interpersonal skills to interact effectively with older patients. Review a variety of strategies to help patients accomplish functional tasks. Review orthopaedic skills – these are frequently used in this setting. Prepare to communicate frequently with occupational therapists, speech language pathologists, respiratory therapists, nurses, nurse’s aides, social workers and physicians. ACUTE CARE Acute Care-Inpatient: In a hospital, caseloads may include adult and/or pediatric patients. Patients may be seen in the intensive care unit, bedside and/or in the Physical Therapy Department of the hospital. A major component of the caseload may be patients who have just had orthopaedic surgery (joint replacement, spine surgery, fracture repair, etc). Depending on the facility, patients may be seen on a number of services at the hospital, such as general medical/surgical, oncology, neurology, cardiac or transplant. From the Class of 2006: This is a fast paced setting with exposure to many aspects of acute care, including intensive care units (ICU), cardiac care units (CCU), medical/surgical units and transitional care units. There is a wide variety of diagnoses seen. Physical therapists are frequently the first to get patients up out of bed. Discharge planning is done beginning with the first patient visit and physical therapists determine the appropriate and safe return to home or other living options. Students need strong communication skills to work with patients, families, nurses, occupational therapists, speech language pathologists, physical therapy assistants, discharge planners and physicians. From the Class of 2007: A primary responsibility for PTs in this setting is to monitor response to activity after a surgery or during recovery from illness. Therefore, knowledge of oxygen saturation, blood pressure, heart rate, respiratory rate and the changes with modification of position or activity is vital. Physical therapists also play an integral part in discharge planning to an environment that is safe and most conducive to the individual patient’s healing process. You need to be prepared for interruptions from other health care team members working with your patients. Often, you will need to be flexible as your caseload may change frequently. Strategies to prepare for an internship in this setting: Practice evaluations for an acute care setting. Review all precautions with lines and management of lines. 8 Practice transfers and bed mobility. Review lab values – make a “cheat sheet”. Prepare to instruct in functional activities. Be ready for discharge planning – learn about options (Skilled Nursing Facilities, rehab, home health). Practice chart reviews. Review post-surgical precautions. Read chapters in the pathology text regarding cardiopulmonary and respiratory diseases. Review medical terminology. OTHER INTERNSHIP OPPORTUNITIES Other clinical internship opportunities may include experiences in pediatrics, home care, women’s health, work hardening, wound care, industrial, administration, cardiac rehabilitation, wellness/prevention, aquatics or chronic pain. Other types of experiences are also possible. Pediatrics: At pediatric sites, neurologic diagnoses are commonly seen but orthopedic diagnoses may be seen as well. There are basically three types of options available in a pediatric experience. 1) School system. May include 3 – 12 or birth to 21. This experience will offer the unique perspective of physical therapy delivered in an educational based model rather than the medical model. It is important that students understand this distinction when requesting a school based experience. Often physical therapists provide services at more than one location so students must be willing to be flexible and mobile. Students must have their own transportation. From the Class of 2007: Physical therapy in the school system is an educational based model. Physical therapy is a support service available to the children who require extra help/interventions/adaptations to enable them to participate as much as possible in the school with their peers. Physical therapy supports the education, especially physical education that is the focus of the interventions provided. Physical therapy could include individual therapy or group based therapy (adaptive physical education). Strategies to prepare for an internship in this setting: Read about the Individuals with Disabilities Education Act (IDEA) and Individualized Education Plans (IEPs): information can be found on the web. Be ready to be creative with therapeutic play activities. Review autism, attention deficit behavior modification strategies and motivational strategies for working with children. 2) Hospital. Will most likely include outpatient as well as inpatient services. The proportion of outpatient to inpatient will vary depending on the facility. 3) Outpatient Clinic. May be based primarily in an outpatient clinic but services may also include home care, school system contracts and/or residential facility coverage. It is important that students be willing to be flexible and mobile. Students must have their own transportation. 9 From the Class of 2006: Common diagnoses include neuro/developmental delays, cerebral palsy and Down’s Syndrome. The age range could be birth to 18 or 21. Evaluations used include the Bailey, Bruininks Osteretsky Test of Motor Proficiency and the Peabody and others. From the Class of 2007: Students must be able to meet the physical requirements of working in an outpatient pediatric setting, including sitting, kneeling, lying on the floor and lifting/carrying children comfortably and safely. Strategies to prepare for an internship in this setting: Work on family education. Be prepared to deal with behavior issues throughout treatment sessions. Develop effective communication skills with children. Review assessment tools and standardized tests used in pediatric settings. Prepare to work in a collaborative model with occupational therapists and speech language pathologists. Be prepared to research new diagnoses. Know the developmental sequence (i.e., when babies roll, sit, stand, etc.). Spend some time around children who have typical development. Evaluate a child who is developing typically using a measure, such as the Peabody. Learn basic sign language (yes, no, please, thank you, etc). PROGRAM EXPECTATIONS OF THE STUDENTS The clinical education component of the Program offers the student the exciting opportunity to engage in collaborative, experiential learning in a variety of practice settings. The unique nature of clinical learning does require that the student allocate additional funds beyond college tuition and fees to cover this curricular requirement. In addition, the student and the student’s support system may need to make temporary compromises in some or all of the areas outlined below. EXPENSES FOR CLINICAL EDUCATION: In order to fulfill the clinical education component of the Program, students will be expected to allocate additional funds for parking, travel and/or relocation housing expenses. RELOCATION: Students should anticipate that clinical education will require geographic separation from their significant other, family, friends and pets. TIME OFF: The Program does not provide the student with any time off during clinical education courses. Any time missed due to illness or emergency must be reported to the DCE and/or the Assistant DCE and the clinical instructor. Time missed must be made up by the student. See the Student Handbook for additional details. 10 HOLIDAYS: Holidays, such as Veteran’s Day, Thanksgiving, Easter, Memorial Day, and others may occur during a clinical education course. The student will follow the same holiday schedule as the clinical instructor. This may mean that the student will not be able to join family and friends for the holiday. VARIABLE CLINIC HOURS: The clinical hours for some students will be approximately 8:00 am – 5:00 pm, Monday through Friday. However, other students will not have this typical schedule. The student may be scheduled for four ten-hour days, or long days on Monday, Wednesday and Friday, with shorter hours on Tuesday and Thursday. Other variable schedules are possible, including weekend hours. Start time may be earlier than 8:00 am and leaving time may be later than 5:00 pm. Students are expected to comply with the schedule assigned to them by the clinical instructor. If students have special needs that do not allow them to comply with an atypical schedule, the DCE and/or Assistant DCE must be informed of this restriction well in advance of clinical assignments. EMPLOYMENT DURING CLINICAL EDUCATION COURSES: The student may not be able to maintain part-time employment during clinical education courses depending on location of placement assignment and hours for the clinical experiences. The student will be expected to comply with the working hours of the assigned facility. If employment hours conflict with facility hours, the student will be expected to change or forfeit employment hours. HEALTH INSURANCE: Students are required to carry health insurance. The health insurance required by EWU may be adequate for Spokane area internships only: refer to EWU health insurance information provided by campus. ASSIGNMENT CANCELLATION: An internship site will not be canceled or changed once it is scheduled unless there are extenuating circumstances, such as a student illness or injury preventing the ability to complete internship requirements, family issues or a problem with the internship site as determined by the Clinical Coordinator of Clinical Education (CCCE) or the DCE and/or Assistant DCE. If the student is required to cancel or change the internship due to the reasons stated, the student will inform the DCE and/or Assistant DCE as soon as possible. It is not acceptable for any student to directly contact a clinical internship site to negotiate or cancel planned clinical internships. CPR REQUIREMENTS The Program requires all students to have completed the Health Care Providers Cardiopulmonary Resuscitation (CPR) certification course. The course will be scheduled during the academic year. Proof of course completion will be provided to the DCE and/or Assistant DCE prior to clinical internships. If recertification is necessary, it is the responsibility of the student to obtain the recertification and provide proof to the DCE and/or Assistant DCE. Students will not be able to continue in a clinical internship if CPR certification lapses. CLINICAL SCHEDULE All students are expected to attend and complete the clinical internships according to the Department schedule that is predetermined by the University academic calendar. The list of internship dates will be given to students during Clinical Education Seminar I in the first quarter of the Program. 11 RELOCATION DURING CLINICAL EDUCATION All students are expected to go out of the Spokane area for a minimum of one internship. During clinical experiences that require relocation, students are responsible for securing their own housing. Students are expected to demonstrate flexibility in being willing to relocate to areas where they may not have friends and/or family. The student is expected to have budgeted funds for relocation expenses. This may mean that a student will need to be paying rent at two locations during the period of the clinical course, in addition to forfeiting income from part-time jobs, if so employed. Students have successfully utilized a variety of ways to secure relocation housing. The following suggestions may be helpful: Consult the Clinical Site Information Form that is filled out by the CCCE and kept on file. On this form, CCCEs can indicate whether they have housing lists available for students or whether they assist the student in securing housing. Many are very willing to help the student find housing. Consult with the DCE and/or Assistant DCE. Sometimes they may know of housing options or can provide the student with suggestions on when and how to contact the CCCE regarding housing, if appropriate. Consult with classmates and friends who may have friends or family in the area. Contact churches and/or the Chamber of Commerce in the area. Contact the student housing office of schools/colleges in the area. Craig’s List. MODELS OF CLINICAL EDUCATION The typical model for PT clinical education is assigning one student to one (or two) clinical instructor/s, and the majority of students have been assigned to clinical experiences of this type. During the past several years, the Program has started utilizing collaborative models of clinical education in which more than one student is assigned to one (or two) clinical instructor/s. Whenever used, these models have provided students with sound learning experiences. The Program will continue to expand its utilization of collaborative models. Some internships are scheduled back-to-back in the same facility. These are large facilities where the student can do two different settings within the system: acute care and outpatient, acute care and rehab, etc. Students scheduled for a back-to-back stay in the same city for two ten week internships. This model was developed to reduce students’ financial burden and increase learning opportunities. From the Class of 2007 on back-to-back internships: (3 of 3 students responding to the questionnaire stated that they would recommend this schedule to future students). Pros o Learning one system vs. two increases the rate of immersion into therapy activities in the 2nd internship at the facility. o You really get to know the people you work with, especially management. 12 o You are able to take on a long but productive project over two internships. o I found this set-up beneficial. The outpatient facility was a satellite clinic so I was not in the same facility for both internships. The only common denominators were the same director of rehabilitation and staff meetings were combined with inpatient and outpatient therapists. The benefits of this set-up were familiarity with staff and system with the second internship. This allows for a shorter adjustment period and increased confidence. o I was able to follow patients from subacute to outpatient. I spent a significant amount of time with three patients in particular and learned a lot from being able to see their progress over a 5 – 6 month period. o This was easier on my family. Cons o If you do not like the facility (management, company), you have to be there longer. o If you did not like the first internship, you would still be there for the second. CLINICAL EDUCATION CLASSES Clinical education classes are held throughout the academic portion of the curriculum to share information about the clinical internships, discuss clinical education topics and concerns and assist the student in the procedures of internship site selection. Included in these classes are clinical education terminology, polices and procedures of clinical education, a review of the Student Handbook, expectations of students during internships, problem solving strategies, discussion and student input regarding learning styles, discussion of the generic abilities, teaching the use of the Clinical Performance Instrument that is used for evaluation during the clinical internships and discussions of ethics, patient confidentiality and professionalism. SELECTIONS PROCEDURES Students are asked to submit a written narrative of their general goals and a description of their learning style. This information is reviewed by the DCE and Assistant DCE and kept in the student’s clinical education file. Students are encouraged to make an appointment with the DCE and/or Assistant DCE to discuss their input information, ask questions about the selections process or share any extenuating circumstances. Site selection for the 5-week internship and the three 10 week internships are completed during clinical education classes. The DCE and Assistant DCE compile information on the sites available for each internship based upon responses to a letter that is sent out to the CCCE of each appropriate facility and 13 share this information with the students. Students will have adequate time to review the sites using the information in the files. Students will then provide input on their specific choices on a form provided. Site selections for the 5-week internship are done during the first fall quarter. Site selections for the first 10-week internship are done during the first spring quarter. Site selection for the second and third 10 week internships are done during the second spring quarter. TYPICAL QUESTIONS ASKED ABOUT THE CLINICAL SELECTIONS PROCESS If I have had lots of experience in a specific practice area as an aide, do I have to have experience in that area during my clinical education sequence? Yes. If you have had extensive work/volunteer experience in any practice area prior to PT school, this is not the same kind of experience that you will have during clinical education in those areas. The task and clinical decision making processes that you will be developing and utilizing as a student physical therapist are quite different from those you utilized as an aide. How can I find out about the clinical sites utilized by the Program? There is a file cabinet available to students containing information about the majority of the clinical sites. There is a copy of the Program’s Clinical Site List with names and addresses of all the sites currently contracted on top of the file cabinet. In addition, there is a map atlas in the file cabinet. Included in these files may be photographs of the site or information that the CCCE has provided. The Clinical Site Information Form that is filled out by the CCCE and placed in these files will give students extensive information about the types of patients seen, the size of the staff, variety of learning experiences available at the site, etc. PT students who have had experiences at that site will have filled out an evaluation form describing their experience at that site and this form is included in these files. The student’s evaluation of the clinical instructor is not included in these files, since that information is confidential. You can also talk with other PT students about their experiences at various clinical sites. Finally, you can talk with the DCE and/or Assistant DCE about specific sites. Viewing the facility’s web site may provide you with additional useful information. Can I contact the clinical site directly with questions regarding the site? No. You should not contact the clinical site directly. Once assigned to a site, you will be able to contact the CCCE with questions. Can I arrange my own clinical education site? No. Students may not solicit new clinical sites on their own behalf or on behalf of the Program. If you know of clinical sites that might be good sites for the Program to investigate, give that information to the DCE or Assistant DCE for consideration. Can I call sites that the Program is currently contracted with to arrange a clinical slot or to inquire about potential clinical slots for myself or other students? No. Under no conditions would this be appropriate. The DCE or Assistant DCE contacts clinical sites about potential clinical slots for students. 14 If I don’t do a specific type of clinical experience, will I ever be able to practice in that specialty? Yes. All graduates will have the ability to practice in a variety of settings. I don’t know what area I would like to practice in after I graduate; is that a problem? No. All clinical internships provide an educational experience that will serve you well, regardless of the practice setting you choose for your first, second, or THIRD jobs! The clinical education program is set up in such a way that you will be competent as a general practitioner upon graduation. You can successfully pursue any practice area once you graduate. In fact, often students take a first job in an area that they could not have imagined themselves in as a first or second year PT student. Take advantage of the variety of clinical sites available. Will I know who my clinical instructor will be once I know which facility I have been assigned to? Generally not. The CCCE will assign the clinical instructor. You will be calling the CCCE at your clinical site about four weeks before each clinical starts. At that time, the CCCE will tell you who your clinical instructor will be. What if I am confused or have questions about the clinical placement process? Talk with the DCE or Assistant DCE as soon as possible. 15