Cardio-11-02
advertisement

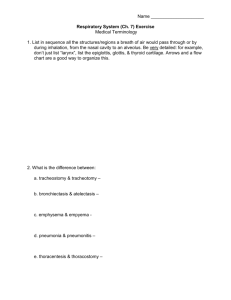
Cardio Notes: 11-02-98 Obstructive & restrictive diseases eat away at Vital Capacity. They both lead to hypoxia (decreased O2) and hypercapnea (increased CO2). RV (residual volume – always there) = 1.2 L ERV (expiratory reserve volume) = 1.1 L TV (tidal volume) = 0.5 L IRV (inspiratory reserve volume) = 3.0 L TLC (total lung capacity) = 5.5 L It is usually 5.8 L in a healthy young male. It is usually 5.0 L in a healthy young female. TIC (total inspiratory capacity) = 3.5 L TLC = TV + IRV FRC (functional residual capacity = 2.5 L FRC = ERV + RV VC (vital capacity) = 4.5 L VC = IRV +TV+ ERV VC = all of the lung tissue that you can inflate and deflate Hypoxemia – lack of O2 in the lungs. Hypercapnea – excess CO2 in the lungs. Look to V/Q if there’s a problem. For instance. If there is normal breathing but the patient is hypoxic and hypercapneic, you must decide if V or Q is the problem. In this case, since breathing is normal, it must be a perfusion (Q) problem. If there is decreased V – problem is in the lungs – pulmonary function If there is decreased Q – problem is in the blood (heart) – circulatory function When you decrease vital capacity, you decrease V. All lung problems decrease V. We want V/Q to be 1/1. In lung problems, V/Q may be ½. SMALLER V/Q. In heart problems, V/Q may be 2/1. LARGER V/Q. Obstructive disease: How does obstructive decrease V? It blocks the airways. Asthma is bronchoconstrictive. There is vagotonia in the smooth muscles causing constriction. Also, there is an increase in mucous. The problem here is in blowing the air out. There is an increase in RV (residual volume) and air is trapped in the lungs. The lungs expand in order to maintain VC (vital capacity). But the amount they are able to expand is limited by the chest size. So the person becomes barrel chested. But as the condition worsens, (patient continues to smoke, etc.) there is more obstruction so the RV keeps increasing and vital capacity begins to decrease (it cannot increase anymore. It has no place to go). FVC (forced vital capacity) = maximum in and maximum out. This is a measure of quality of air. If you are 28 years old and your FVC is 80% of what it should be, it’s time for a change! In obstructive disease, the mechanism of destruction is: Increased RV eats away all the room to breathe. It eats away at the vital capacity. So there is a decrease in VA (alveolar ventilation). In order to treat, you must decrease the obstruction as much as you can so that the patient doesn’t continue to trap air in the lungs, increasing residual volume. In a 30 year-old asthmatic who has normal vital capacity, the RV is probably growing. FEV1 = forced expiratory volume in 1 second. This should be about 80% of FVC (forced vital capacity). This may only be about 60% in a young asthmatic and wheezing may be heard as air is going in and out of the lungs. This is not good. The condition is taking it’s toll. MDs measure FEV1 and give an inhalant with a Beta II agonist (albutyrol).(epinephrine effects Beta II receptors.) Is asthma, the patient is in a hypersympathetic state. The inhaler acts to dilate smooth muscle in the lungs. Now, FEV1 becomes 75% of FVC. So this airway constriction is reversible. Asthma is reversible. A reversible airway disease is asthma. There is a problem with this: albutyrol is hard of the heart. You don’t want the patient using the inhaler more than 2 or 3 times a day. In fact, this should be used more like 2 to 3 times per week. You don’t want a patient to be using this forever. The SA node responds to Beta II drugs by increasing the heart rate. The results are arrhythmias and weakened hearts. The more a patient uses the inhaler, the more he needs it. If he uses too much, this could increase inflammation, which would increase the desire for more drugs. All pulmonary conditions decrease V. Decreased vital capacity decreases V. Increased residual volume decreases vital capacity. There is nothing to prove that a patient can decrease his residual volume after it had increased. We can work with the vital capacity. Tests for lung conditions: Spirometers: expensive and a pain to use. For example, a 50 year-old male, ex-smoker. He quit smoking in Oct, 1995. Prior to that, he had 1PPDX30 (I pack of cigarettes per day for thirty years.) Results of spirometry: VC = 87% of predicted VC. After using an inhaler, it was 90%. FEV1 = 40% of predicted FEV1. This is severe obstruction. The inhaler did not help this. Therefore, this condition is NOT REVERSIBLE for this man. He has emphysema. PEFR = flow meter. The cost is about $25.00. It shows the obstructive state of the lungs. The flow rate expected depends upon age and sex. If the expected flow rate is 516 ml/second and the patient’s is only 320 ml/second, the patient probably has an obstruction. Emphysema is a non-reversible airway disease. Quitting smoking can help the damaged lining of the airway tissues to heal and can decrease the chance of developing cancer. But the quitting smoking does not change the lung size, it cannot decrease the residual volume to it’s original size. Emphysema doesn’t usually damage the lungs irreversibly until the patient is in their 40’s. There is the appearance of a hyperinflated lung. (In asthma, there is not as much inflation of the lungs.) If the patient is not barrel chested, chances are that he doesn’t have emphysema. In bronchitis, there is inflammation of the respiratory bronchioles. In emphysema, there is inflammation of the terminal bronchioles. (Only a little further than bronchitis.) Restrictive Lung Disease: Aka “small lung disease” Problem: interstitial tissue cannot expand. If the patient cannot expand the lung tissue, all lung volumes decrease. There is no problem with the airways. ERV <1.1 L TV < 0.5 L IRV < 3.0 L Vital Capacity << 4.5 L (much less than 4.5 L) Pneumonia and Scoliosis are restrictive, they keep the interstitial tissue from expanding. Atelectasis is restrictive. It affects tissue compliance. There is a collapse of the acinus. They used to put these people on a ventilator until they realized that it destroyed more tissue than it helped. Restrictive disease decreases vital capacity. It decreases FVC. FEV1 is normal or better! FEV1/FVC is higher than predicted. Around 90%! This is because there is a decreased amount of air in the lungs and the patient is able to get rid of it easily. TLV is decreased. The category of lung disease includes: pneumonia, cancer, pulmonary fibrosis (Hamman-Rich), etc. Hamman-Rich syndrome – fatal pulmonary fibrosis, usually within 60 months. Example, a 40 year-old female who has never smoked. VC = 1.58 L Predicted VC – 3.91 L FEV1 = 1.46 L Predicted FEV1 3.24 L TLC = 1.69 L Predicted TLC 6.06 L RV = 0.11 Predicted RV = 2.0 L There are white, cloudy areas in her lung tissue that don’t expand. The fibroblasts in the interstitial tissue are going hog wild. Prednisone helps a little temporarily. Usually with restrictive diseases, the RV doesn’t change. But in Hamman-Rich syndrome and several other conditions, there is a decrease in RV. The lungs in HR Syndrome are filled with adhesions. Sarcoidosis – chronic cough and shortness of breath. Usually in young males (in their 20’s) A form of pulmonary fibrosis 80% of the cases are reversible and the fibrosis disappears leaving no permanent damage. The tissues, however, may take up to ten years to recover. Compliance – the active process of opening. Increases in obstructive diseases. The lungs are easily expanded. Decreases in restrictive diseases. Recoil – a passive process of closing. Decreases in obstructive diseases. Increases in restrictive diseases. Obstructive disease: Increased compliance Decreased recoil Restrictive disease: Decreased compliance Increased recoil