GI Physiology: Digestion and Absorption I
advertisement

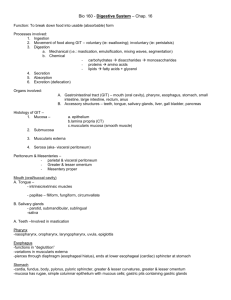
GI #41 Mon. 03/03/03 8 a.m. (Orig. Thur. 02/27/03 1 p.m.) Dr. Gwirtz Scribe: Malik Ali Page 1 of 8 This scribe has not been reviewed and probably won’t be because Dr. Gwirtz will be out of town on Wed. But I assure you I included EVERYTHING on the lecture tape. I feel I did a thorough job. If you have any questions listen to the tape. GI Physiology: Digestion and Absorption I Digestion and absorption - Objectives Describe the process of digestion and absorption of carbohydrates (in the small intestine) Describe the process of digestion and absorption of proteins Describe the process of digestion and absorption of lipids – how bile salts are involved Describe the role of bile salts in the uptake of lipid digestion products (monoacylglycerol and fatty acids) by the small intestine Describe the chylomicrons and very-low-density lipoproteins made by the small intestine List the fat- and water-soluble vitamins and describe their mechanisms of absorption by the gastrointestinal tract Describe the mechanisms of absorption of sodium, calcium, and iron by the gastrointestinal tract Describe how water is absorbed in the GI tract Describe the malabsorption syndromes of the small intestine Digestion and absorption begin as soon as you start eating a meal. For example, eating a hamburger will begin the process by digesting starches via salivary αamylase in the mouth, continues to the stomach, and mostly to the small intestine. Absorption of a number of calories, proteins, carbos, other electrolytes and water occurs. Anatomical Basis of Absorption Most occurs in small intestine. Very little occurs in stomach b/c of tight junctions among epithelial cells that inhibit absorption due to thick mucosal barrier. Some very lipid-soluble substances absorbed in stomach due to poor absorptive surface - alcohol - asprin - absorbed unionized in stomach acid; ionized in epithelial cell causes damage - some drugs, ex – digitalis If you ate a 5 Lb bag of sugar, you would absorb it! Absorptive surface in small intestine increases 600 X: 1 GI #41 Mon. 03/03/03 8 a.m. (Orig. Thur. 02/27/03 1 p.m.) Dr. Gwirtz Scribe: Malik Ali Page 2 of 8 – simple tube – folds - 3X – villi - 10 X – microvilli - 20 X arrangement of blood vessels and central lacteal – important for countercurrent exchange for nutrients in villi pinocytic vesicles unstirred layer exists among microvilli – cells are continuously secreting a watery solution to allow nutrient absorption across epithelial cells to blood capillary or lymphatic system. Absorption in small intestine CHO, fat, amino acids, electrolytes, vitamins, minerals, water Absorptive capacity much greater than needed normally - Normally absorb several hundred grams CHO, 100 g fats, 50-100 g amino acids, 50-100 g ions, 8-9 L water - Max capacity for water absorption is 20 L or more per day - Cholera toxin can cause us to lose 20-30 L/day thus overpowering our capacity to absorb fluid and we lose fluid instead General Mechanisms of Digestion & Absorption The most basic mechanism of digestion is hydrolysis whether it is a protein, CHO, or fat: R” - R’ + H2O → R”OH + R’H. Enzymes act on the R-R link. All starches, sugars converted to glucose, galactose, or fructose for absorption Proteins and amino acid peptides broken down into amino acids for absorption Lipids, cholesterol, cholesterol esters broken down to free fatty acids and glycerol to diffuse into epithelial cells and then absorbed as triglycerides and cholesterol Chemical digestion of carbohydrates (Fig 24.33a in Berne and Levy) Starches are begun to be broken down to oligosaccharides by salivary amylase in the mouth – 40% of starches digested by this enzyme until it is inactivated by acid Pancreatic -amylase continues the digestion of oligosaccharides in the small intestine – 60% of starches digested this way Lactose and Sucrose have no digestive activity in mouth or via pancreas but are digested by intestinal brush border enzymes (located on the microvilli) – lactose into galactose and glucose, maltose (a glucose polymer) into glucose, and sucrose into glucose and fructose 80% of sugar absorbed is glucose, 10% is galactose, 10% is fructose Absorption of Carbohydrates 2 GI #41 Mon. 03/03/03 8 a.m. (Orig. Thur. 02/27/03 1 p.m.) Dr. Gwirtz Scribe: Malik Ali Page 3 of 8 Sources: sucrose, lactose, starches Absorbed as a monosaccharide: glucose, galactose, fructose Glucose & galactose: via an active Na+- co-transport mechanism across epithelial cell Fructose: facilitated diffusion CHO Digestion & Absorption in the Small Intestine Glucose-1 transport mechanism – glucose and Na+ attach to a carrier molecule to bring glucose inside (Na-cotransport requires energy) Galactose via a similar mechanism w/ Na+ attached to a carrier Fructose comes in via a facilitated diffusion mechanism which requires no energy Absorption of Glucose From Various Carbohydrate-Containing Foods Glucose in its pure form has a glycemic index of 100 which means it absorbs quickly Within other foods, absorption of glucose is a little less Dietary Fiber CHO not digested by human GI tract: cellulose, hemicellulose, pectins Bind water Decrease transit time (meal spends less time in GI tract) ADsorb!!! minerals: Ca, Fe, Mg, Zn ADsorb organic material: bile salts (bile pool is decreased), lipids Bacterial flora digest gas Failure to absorb osmotic diarrhea (mechanism of laxatives to increase motility) Too much fiber can be bad. If on a high fiber diet, you can end up with certain malabsorption syndromes. Also can become dehydrated. Lactase deficiency can also cause osmotic diarrhea and lots of gas. Chemical Digestion of Proteins (Fig. 24.33 – Berne and Levy) Protein digestion begins in stomach by pepsin which is activated by HCl from pepsinogen In the small intestine, trypsinogen is activated by the brush border enzyme enterokinase and then trypsin activates other proteolytic enzymes. Enterokinase must be present!!! 3 GI #41 Mon. 03/03/03 8 a.m. (Orig. Thur. 02/27/03 1 p.m.) Dr. Gwirtz Scribe: Malik Ali Page 4 of 8 Proteases and Peptidases in the Small Intestine Pancreatic proteases digest the proteins into oligopeptides which are futher broken down by the brush border enzymes (amino peptidases, carboxypeptidases, dipeptidases) into amino acids You still have some di- and tripeptides present Absorption of Proteins Meats, plants Digestion by Epithelial Peptidases Absorbed as dipeptides, tripeptides and free amino acids Active Na+-co-transport mechanism - most amino acids absorbed by this mechanism 5 different amino acid and peptide transport proteins in luminal membrane Absorption of Di- and Tripeptides Across Brush Border Even though you have di- and tripeptides entering across the brush border, you have cytoplasmic peptidases which will further break down into amino acids Only thing that enters portal circulation are amino acids which eventually enter the blood Amino Acid Transporters in Brush Border and Basolateral Membrane - charts from book, don’t memorize - several are Na+ dependent, some are Na+ independent Conversion of Inactive Pancreatic Proenzymes to Active Enzymes Proenzymes like trypsinogen are secreted by the pancreas and are converted to trypsin by enterokinase (in brush border) which then acts to activate other proteolytic enzymes Fat (Large, Lipid Droplets) Digestion / Absorption Emulsified by acid, pepsin in stomach; minimal digestion by gastric lipase Requirement for bile salts: a) Continue emulsification in small intestine using bile salts in segmentation contractions – breaking large droplets into small ones b) Digestion by pancreatic lipases c) Bile salt micelles transport fats to surface of epithelial cells. Lipid soluble side attaches to lipid droplet, and enzymes attach to soluble side of bile salt to begin digestion of lipids d) Fats diffuse into epithelial cells (bile salt stays in lumen) – digested and absorbed in small intestine 4 GI #41 Mon. 03/03/03 8 a.m. (Orig. Thur. 02/27/03 1 p.m.) Dr. Gwirtz Scribe: Malik Ali Page 5 of 8 Greasy pan being washed by a detergent – similar to bile salts on lipids Lipid Digestion Once emulsified, pancreatic lipases convert to monoglycerides and fatty acids and also to glycerol and fatty acids Cholesterol esters must be digested by cholesterol esterases for cholesterol to be absorbed Action of Pancreatic Lipases Triglyceride is hydrolyzed into 2-Monoglyceride and free fatty acids by Glycerol ester hydrolase Cholesterol ester is hydrolyzed into cholesterol and fatty acid by cholesterol ester hydrolase Lecitin is hydrolyzed into lysolecitin and fatty acid by phospholipase A2 Absorption of Fats Once lipids in epithelial cell, need to absorb into circulation via chylomicrons Formation of chylomicrons (big fat globules) - Fats recombined to form new triglycerides in endoplasmic reticulum - Aggregate into globules along with absorbed and newly formed cholesterol, phospholipids in Golgi apparatus - Coated by apoprotein Absorption of Fats Exocytosis of chylomicrons through basolateral membrane and into lymphatic capillary b/c too big to enter blood capillary - Enter blood circulation Absorption can describe the whole process getting into the blood circulation via the liver, not just to epithelial cell Small chain fats can diffuse through epithelial cell into blood (40% of dietary lipids) – don’t require bile salts Absorption of bile salts - Na-cotransport in terminal ileum Other 60% are medium/large chain and must have bile salts – chylomicrons – for excretion through lymphatics Unstirred Layer Figure diffusion of micelle with bile salts surrounding it. Micelle moves lipids through unstirred layer so that they can move through epithelial layer to be absorbed. Monoglycerides, cholesterol, and free fatty acids are moved 5 GI #41 Mon. 03/03/03 8 a.m. (Orig. Thur. 02/27/03 1 p.m.) Dr. Gwirtz Scribe: Malik Ali Page 6 of 8 Figure – Inside epith cells, ER and Golgi aid in making chylomicrons. Make trigylycerides, phospholipids, cholesterols are re-esterified Form Chylomicrons Exocytosis into lymphatics Difference between small and large chain lipid absorption – know the process Absorption of Bile Acids in Terminal Ileum Transporter binds bile acid to one site and Na+ to another Move bile acid into epith cell and into portal blood (high in bile salt conc.) Each bile salt used about 3 times in a meal Overall Fluid Balance in GI Tract Ingesting about 9 L/day total 1. Ingest 2 L/day of water 2. 1.5 L/day of saliva 3. 2 L/day of gastric secretions 4. .5 L/day of bile 5. 1.5 L/day of pancreatic juices 6. 1.5 L/day of intestinal secretions Small intestine absorbs 8.5 L/day Colon absorbs 400 mL/day 100 mL/day water excreted Where is most of the water absorbed in the GI tract? – the small intestine!!! – absorbs 8-10 L/day; Large intestine – approx. 1 L/day Water Absorption in the Small Intestine Diffusion, mainly through pores between the epithelial cells - 85-95% absorbed in upper small intestine (duodenum and jujenum) Follows osmotic gradient created by absorption of nutrients and electrolytes Exception: entry of hyperosmotic chyme from stomach into duodenum results in osmosis of water (secretion) into the intestinal lumen to make iso-osmotic soln. relative to plasma. But that water is actually absorbed, it doesn’t just sit there 1-3 liters ingested, 7-10 liters secreted by gut, but only 150-200 ml excreted in feces! 6 GI #41 Mon. 03/03/03 8 a.m. (Orig. Thur. 02/27/03 1 p.m.) Dr. Gwirtz Scribe: Malik Ali Page 7 of 8 Table 34.1 – Transport of Na+, K+, Cl-, and HCO3- in the large and small intestines Na+ is absorbed in all regions of the gut – jujenum, ileum, colon. Active transport is a co-transporter which requires Na+ along with other nutrients – glucose, galactose, bile salt co-transport in ileum – in order to be absorbed. Co-transporters require energy in active transporter mechanisms Cl- is normally absorbed in small intestine following electro-chemical absorption gradient by Na+, HCO3- usually follows as well Na+ is passively absorbed in the small intestine following water through the pores In the ileum and colon, Cl- is absorbed in exchange for the bicarb ion secretion The bicarb is secreted because it is needed in the colon to neutralize the acid secreted by the bacteria there Major Ion Transport in Jejunum Most nutrients absorbed here Na+ co-transport with different sugars and amino acids (active transport) Cl- follows Na+ Na+/H+ exchange for absorption of Na+ K+ is passively absorbed between the cells Active Na+/K+ exchange in order to keep Na+ low in the cell Major Ion Transport in Ileum Na+ co-transport with sugars, amino acids, and particularly bile salts Cl- follows by the electrical-chemical gradient Na+/H+ exchange and also Na+ pump at basolateral membrane Active Cl- absorption in exchange for HCO3- secretion (neutralizes acid by bacteria) Major Ion Transport in Colon Na+/H+ exchange Only electrolytes, water, and things like vitamin K that are made by bacteria No absorption of CHO, amino acids, or lipids Absorption of Sodium Ions 25-35 g daily ingested Mechanisms at luminal membrane 1. diffusion through Na+ channel 2. coupled Na+- Cl– co-transport 3. Na+-H+ co-transport 7 GI #41 Mon. 03/03/03 8 a.m. (Orig. Thur. 02/27/03 1 p.m.) Dr. Gwirtz Scribe: Malik Ali Page 8 of 8 Na+-solute co-transport (glucose, galactose, amino acids, bile salts) Active transport through basolateral membrane into intercellular spaces to blood circulation 4. Absorption of Chloride Ions Follows electrochemical gradient created by absorption of Na+ Active absorption in distal ileum and large intestine in exchange for HCO3- ions (for buffering acidic products formed by bacteria) Absorption of Bicarbonate Absorbed in jejunum with Na+ Active secretion in distal ileum and large intestine in exchange for Cl(wrong in ppts) ions (for buffering acidic products formed by bacteria) Absorption of Ions Potassium - passive, through tight junctions and lateral spaces Calcium - active - absorbed relative to body’s need via parathyroid hormone and vitamin D Iron - active - absorbed relative to body’s need Calcium and Iron absorbed according to body’s needs Absorption of Ca++ Ca++ binding protein inside cell Amount of Ca++ conc. inside cell dependent upon vit D converting 25-hydroxycholcalciferol in the liver to Ca++ binding protein synthesis If you need more Ca++ in cell, you will make more Ca++ binding protein to bring in more Ca++ If you don’t need Ca++, the Ca++ stays in the cell and when cell is sloughed off it is excreted Effects of Vitamin D3 on Ca++ Absorption With Vit D, you make more binding protein and absorb lots of Ca++ in duodenum Without Vit D (control), you absorb some Ca++ but to a lesser extent 8