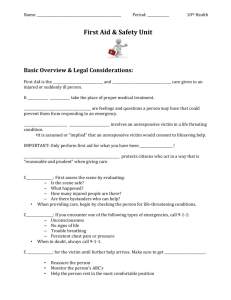
First aid: immediate care given to victim of injury or sudden illness
advertisement

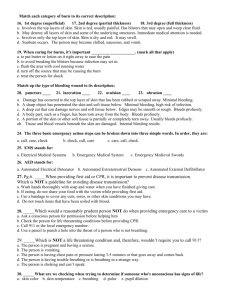
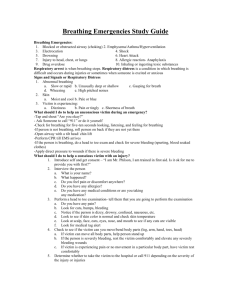
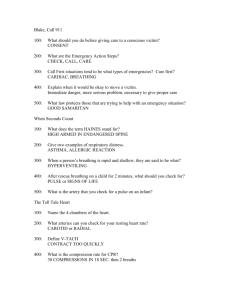
First Aid and CPR 11th grade First aid: immediate care given to victim of injury or sudden illness until more advanced care can be obtained. First responder: a person trained in emergency care that may be called on to give such care as a routine part of his job. Citizen responder: a person who recognizes the emergency and decides to act. This person may not have special or advanced medical skills or training. Injury: damage that occurs when the body is subject to an external force such as a blow, a fall, a collision, an electrical current or temperature extremes. Emergency: a situation requiring immediate action. Life-threatening emergency: an illness or injury that impairs the victim’s ability to circulate oxygenated blood to all the parts of the body. Non-life-threatening emergency: a situation that does not have an immediate impact on victim’s ability to circulate oxygenated blood, but still needs medical attention. Good Samaritan law: laws that protect people who willingly give first aid without accepting anything in return. Citizen responder’s role in emergency: Recognizing that an emergency exists Deciding to act Taking action by calling 911 or local emergency # Giving care till medical help arrives Emergency action steps: 1. Check the scene and the victim 2. Call 911 or local emergency # 3. Care for the victim Checking the scene: Is the scene safe? What happened? How many victims are there? Are bystanders available to help? 1 Checking the victim for life threatening emergencies: 1. Unconsciousness 2. No breathing or trouble breathing 3. No signs of life (pulse, breathing, coughing or movements) 4. Severe bleeding Calling 911: Who you are Where you are What the emergency is Condition of victim Care given so far If you are alone call first then care for: Unconscious adult or adolescent victim Witnessed sudden collapse of a child or infant Unconscious child or infant with risk of heart problem If you are alone care first for: Cardiac emergencies Breathing emergencies Bleeding emergencies Give 2 minutes of care then call 911 Disease transmission: passage of disease from one person to another. How bloodborne pathogens are spread; 1. A pathogen is present 2. There is enough of the pathogen present to cause disease 3. Pathogen passes through correct entry site 4. A person is susceptible to pathogen How to prevent the spread from person to person: Personal hygiene Personal protective equipment Cleaning up blood spill What to do if you are exposed: 1. Wash the exposed area quickly as possible 2. Be sure to notify the professional on site 3. Seek medical attention Obtaining consent: 1. Who you are 2. Your level of training 3. The care you would like to give 2 Do not move the victim unless there is risk of fire, gas explosion, toxic gas, risk of drowning or collapsing structure. How to move the victim: 1. Walking assist 2. Pack strap carry 3. Two-person seat carry 4. Clothes drag Checking the victim for life threatening emergencies: Unconsciousness No breathing or trouble breathing No signs of life (pulse, breathing, coughing or movements) Severe bleeding Shock: The condition in which the body fails to circulate oxygen-rich blood to all parts of the body. If left untreated, it can lead to death. Checking for consciousness: 1. Tap the shoulder and ask “are you ok?” 2. Call 911 or local emergency # Checking for pulse: 1. Adult---carotid artery 2. Child or infant---brachial artery Checking an unconscious person: 1. Check for open air way 2. Check for breathing 3. Check for signs of life 4. Check for sever bleeding If the person is unconscious do the ABC which stands for: Airway: open the airway Breathing: check for breathing Circulation: check for signs of life and bleeding Airway: head tilt/chin lift technique: move the tongue from the back of throat, allowing air to enter the lungs. Breathing: look, listen and feel for no more than 10 seconds. If no breathing: 1. Give 2 rescue breaths lasting 1 second each 2. If the air goes in (chest rises), check for signs of life 3. If no signs of life, begin CPR Circulation: Carotid artery for adults Brachial artery for children and infants 3 Checking a conscious victim: Interview the victim and bystanders Check the victim from head to toe Medical ID tags and bracelets will provide important medical information about victim. Giving care: Do not further harm Monitor breathing and consciousness Help victim rest in a comfortable position Keep the victim from getting chilled or overheated Reassure the victim Give any specific care needed Without oxygen brain cells begin to die in 4 to 6 minutes. Breathing emergencies are either respiratory distress or respiratory arrest. 1. Respiratory distress can be caused by: 2. Partially obstructed airway 3. Illness 4. Emphysema or asthma 5. Electrocution 6. Heart attack 7. Head, chest, lung or abdomen injury 8. Allergic reaction 9. Drugs 10. Poisoning 11. Emotional distress Anaphylactic shock: is a severe allergic reaction which causes difficulty breathing. Symptoms of anaphylactic shock are tightness in chest and throat and swelling of face and neck. The person in shock should be immediately injected with EpiPen. Airway obstruction: 1. Anatomical---airway is blocked by the tongue or swollen issue of mouth and throat. 2. Mechanical---airway is blocked by food or toy or vomit or blood. Care for airway obstruction in conscious victims: 1. Encourage the victim to cough forcefully to dislodge the objects 2. Provide five back blows 3. Provide five abdominal thrusts 4. For infants and pregnant women provide five chest thrusts 4 If respiratory arrest occurs and victim stops breathing, do the following: Lay the victim on his back Head tilt/chin lift Look for object in the mouth and dislodge it Give the rescue breaths every 3 seconds for about 2 minutes If the breaths don’t go in, begin CPR Cardiac emergencies and unconscious choking: Heart attack: a condition in which blood flow to some part of the heart muscle is compromised and the heart begins to die. If enough of heart muscle dies, the heart can not circulate blood effectively. Cardiac arrest: a condition in which the heart stops beating. Cardiopulmonary Resuscitation (CPR): a combination of chest compression and rescue breathing. (Cardio=heart, pulmonary=lungs) Cardiac chain of survival: 1. Early recognition and early access 2. Early CPR 3. Early defibrillation 4. Early advanced medical care Check for heart attack: Check-Call-Care CPR: is not effective if the victim is on soft surface like a sofa or mattress. You should place your body sideways to the victim Place the heel of one hand on the victim’s sternum (breast bone) at the center of his chest. Place other hand directly on top of the first hand. Use the heel of your hand to apply pressure on the sternum. Try to keep your fingers off the chest by interlacing them together and upward. Compressions should be a rate of 100 per minute. Count 1 and 2 and 3.....up to 30 in 18 seconds. Do 30 compressions and 2 breaths (1 breath every 5 second for adult and every 3 second for child). Open airways after 30 compressions, then give 2 breaths. Do 5 cycles (about 2 minutes) then check for signs of life. When to stop CPR: The scene becomes unsafe The victim shows signs of life An AED becomes available and is ready to use Another trained rescuer arrives and takes over You are too exhausted to continue 5 AED (automated external defibrillator): gives an electric shock or defibrillation to the victim of cardiac arrest. For each minute that defibrillation is delayed the chance of survival is reduced by 10%. 1. Turn on the AED 2. Wipe off the victim’s chest dry. Apply pads on chest. 3. Let AED analyze the heart rhythm and say a) stand clear b) deliver shock 4. Push the button and wait for instructions Caution: Do not use AED around water. Remove wet close. Remove victim from the puddle Do not place AED on implantable devices. Remove nitroglycerine patch on victim’s chest before AED use. Bleeding: large amount of bleeding in short amount of time is called hemorrhage. Bleeding could be internal or external and both could life threatening. External bleeding is visible and comes from the wound. Internal bleeding is inside the body and difficult to recognize. Care for external bleeding: Check, Call, Care Cover with sterile dressing Apply direct pressure until bleeding stops Cover dressing with bandage Call 911 Monitor victim Care for internal bleeding: Do not further harm Monitor breathing and consciousness Help the victim rest in a comfortable position Keep the victim from getting chilled or overheated Give specific cares needed Shock: is a progressive condition in which the circulatory system fails to circulate oxygen-rich blood to parts of the body. When vital organs such as brain, heart, and lungs do not receive oxygen-rich blood, they function properly. 3 conditions needed to maintain adequate blood flow: 1. The heart must be working well 2. An adequate amount of oxygen-rich blood must be circulating in the body 3. The blood vessels must be intact and able to adjust blood flow Types of shock: 1. Anaphylactic (affecting breathing) 2. Cardiogenic (occurs with heart attack) 3. Hypovolemic (severe bleeding or loss of plasma) 4. Neurogenic (emotional shock or fainting) 5. Septic (caused by severe infection, bursting appendix). 6 Signs of shock: Restlessness or irritability Altered consciousness Pale or ashen, bluish, cool or moist skin Rapid breathing Rapid and weak pulse Excessive thirst Nausea or vomiting Care for shock: Check, Call, Care Help the victim lie down on his back Elevate legs about 12 inches to help the blood circulate to vital organs Do not elevate legs the victim is nauseated or having trouble breathing Do not elevate legs if you suspect head, neck or back injury Do not elevate legs if there are broken legs or hips Do not give victim anything to eat or drink (he may need surgery) Injuries to soft tissues: Wound: is any physical injury involving a break in layers of skin (epidermis=outer layer, dermis=deeper layer and hypodermis=last layer). Closed wound: the outer layer of the skin is intact and the damage lies below the surface which may cause internal bleeding. Open wound: the outer layer of skin is broken and there is external bleeding. Types of open wound are: Abrasions: the most common type of open wound. It is characterized by the skin being rubbed or scraped away. It is always painful because it exposes the nerve endings. Lacerations: it is a cut commonly caused by a sharp object such as knife. It is not painful because nerve endings are damaged and can’t send signal to the brain. Avulsions: an injury in which a portion of skin or soft tissue is partially or completely torn away. Bleeding is significant in avulsions. If the body part is severed, it is called amputation. Punctures: it is the result of skin being pierced with a pointed object such as nail, piece of glass or a knife. Burns: 1. Superficial (first degree): involve only the top layers of skin, take 5-6 days to heal without scarring. Sunburn is an example of 1st degree burn. 2. Partial thickness (second degree): involve deeper layers of skin, are red and cause blisters filled with water, are painful, take 3-4 weeks to heal, scarring may occur. 7 3. Full thickness (third degree): destroys all the layers of skin, affects underlying tissue, it is life threatening, results in scarring, takes long to heal. Care for burns: Check the scene for safety Stop the burning by removing the victim from the source of the burn Check for the life-threatening conditions Cool the burn with large amount of cold running water Cover the burn with loose sterile dressing Prevent infection Keep the victim from getting chilled or overheated Do not put ointment, butter, oil or other commercial or home remedies on blisters or deep burns because they seal the heat in and they have to be removed when personnel arrive. Specific types of burn: chemical, electrical, radiation Musculoskeletal injuries: Joint: a structure where to bones are joined Tendon: a cordlike, fibrous band that attaches muscle to bone Ligament: a fibrous band that attaches bone to bone Muscle: a soft tissue that creates movement Fracture: a break or disruption in bone tissue Dislocation: the displacement of a bone from its normal position at a joint Sprain: the stretching and tearing of ligaments and other soft tissue at the joint Strain: the stretching and tearing of muscle and tendon Care for musculoskeletal injuries: Call 911 if: The injury involves the head, neck or back The injury impairs walking or breathing You see or suspect a fracture or dislocation You suspect multiple injuries Otherwise do the “RICE” Rest: place the victim in a comfortable position Immobilization: avoid moving the injured body part Cold: helps reduce swelling and eases pain Elevation: helps with the blood flow and reducing the swelling Splint: a device used to immobilize body parts. Types of splint are: Soft splint (towel, blanket), rigid splint (board, metal strip, magazine), anatomical splint 8 Injuries to the extremities: arm, forearm, clavicle, shoulder, elbow, wrist, finger, knee, ankle, foot. Injuries to the head neck and back: brain, face, neck, spine, nose, eye, ear, mouth, jaw. Care: Minimize head, neck and back movement Check for life threatening conditions. Make sure to maintain an open airway. Monitor consciousness and breathing Control external bleeding Maintain normal body temperature Manual stabilization: placing the hands on both sides of the victims head. Concussion: a temporary impairment of brain function due to a head injury. Amnesia: loss of memory. Different from concussion Do not attempt to align the head and neck in case of neck and spinal injuries. Injuries to the chest, abdomen and pelvis: Care for rib fractures: Have the victim rest in a position that will make him breath easier Do not move the victim if you suspect head, neck or back injury Call 911 Use a rolled blanket or pillow to support and immobilize the area Bind the victims arm to the chest on the injured side Monitor breathing to minimize shock Care for puncture wounds (gun shot): Cover the wound with a large dressing that does not allow air to pass through Tape the dressing in place Call 911 Take steps to minimize shock Care for injuries to abdomen (internal organs protruding): Call 911 Put on disposable glove Carefully position the victim on the back Do not apply pressure Do not push any protruding organs back in Remove clothing from around the wound Cover dressings loosely with plastic wrap Cover dressings with a light towel to maintain warmth 9 Care for pelvis injuries: Do not move the victim unless necessary Try to keep the victim flat Control the external bleeding Call 911 take steps to minimize shock Sudden illness: fainting, diabetic emergency, seizure, stroke, poisoning, heart attack and shock. Fainting signals: sweating, vomiting, distortion or dimming vision, head or abdominal pain Care for fainting: Position the victim on the back Elevate the legs about 12 inches for blood circulation Loosen clothing Check for life-threatening conditions Do not give victims anything to drink or eat Do not slap the victim or splash water on their face If the victim does not recover, call 911 Diabetic emergency: diabetic person’s pancreas gland does not produce insulin and the patient has to take insulin injections to regulate the blood sugar. Too little or too much insulin will cause a drop in blood sugar. Care for diabetic emergency: give victim something sweat such as candy, fruit juice or dissolve table sugar in some water and give it to victim. If the situation is serious call 911 Seizure: when the electrical activity of brain becomes irregular, the body loses control of movement. This control loss is known as seizure. Head injury, disease, fever, poisoning or infection can initiate seizure. Before seizure, victim experiences an aura such as hallucination, a strange sound or smell. Care for seizure: Do not try to stop the seizure Do not hold or restrain the person (it may cause injury) Do not try to place anything in person’s mouth or between teeth After seizure is over let the person rest for a while If the victim does not recover, call 911 Stroke: disruption of blood flow to a part of brain causing permanent damage to brain tissue. Also called “cerebrovascular” accident or “brain attack” Fast recognition of stroke: Face-Arm-Speech-Time (911) Control of stroke: control blood pressure, no smoking, healthy eating, exercise 10 Signs of poisoning: nausea, vomiting, diarrhea, trouble breathing, sweating, seizure, headache, dizziness, weakness, etc. 4 ways of poisoning: Inhalation, ingestion, absorption and injection Inhalation: breathing toxic fumes such as gases and chlorine or fumes from the household products such as glue and paints or from drugs such as crack cocaine. Care: make oxygen available if possible, call 911 Ingestion: swallowing poisonous food such as certain mushrooms and shellfish or drugs and alcohol or household cleaning products. Care: encourage them to vomit Absorption: when the poison comes to contact with skin and gets absorbed such as poisonous plants, poison ivy, and poison oak. Care: rinse the affected area, use medicated lotion Injection: the poison enters the body through bites or stings of insects, spiders, ticks, marine life, animals and snakes. Care for insect bites: remove the stinger from the skin by scraping it with nail or a credit card. Do not use tweezers because the venom sac may rupture in the skin, wash site with soap and water, apply ice to reduce swelling Care for ticks bite: ticks can carry Lyme disease. Pull the tick out of skin by tweezers. Use antibiotic prescribed by physician. Care for spider and scorpion bites: call 911, wash the wound, and apply ice. Care for snake bite: call 911, wash the wound, keep injured area lower than the heart, do not apply ice, do not cut the wound, do not apply suction, do not apply tourniquet, and do not use electrical shock such as from the car battery. Care for jelly fish sting: rub alcohol or baking soda, do not use meat tenderizer. Heat and cold related emergencies: people at increased risk are: Those who work or exercise strenuously in a warm or cold weather Elderly people Young children Those with predisposing health problems such as diabetes and heart disease Those who take diuretic medication Types of heat related emergency: Heat cramp: to care for heat cramps have the victim rest comfortably in a cool place, lightly stretch the muscle then grasp and squeeze it, provide cool water or sports drinks, if the victim does not recover give salt water. Heat exhaustion: it occurs after long periods of exercise in hot and humid environment or with certain jobs such construction or fire fighting. To care for heat exhaustion, provide rest, fluid, and prevent from shock. Heat stroke: is the most severe form of heat related emergency and it often happens when people ignore signals of heat exhaustion and needs the same care as heat exhaustion 11 Types of cold related emergency: Frostbites: it is freezing of body tissues. The signs are: Lack of feeling in affected area Skin that appears waxy Skin that is cold to touch Skin that is discolored (flushed, white, yellow or blue) Care: Get the person out of cold Do not try to rewarm the frostbitten are Rub the affected area gently Soak the affected area in warm water Loosely bandage the area Avoid breaking a blister Call 911 Hypothermia: it is the general cooling of the entire body as the body temperature falls bellow 95 degrees (normal 98). It may cause abnormal heart rhythm and death. Signs are: Shivering Numbness Glassy stare Decreased consciousness Weakness Impaired judgment Care: Gently move person to a warm place Remove wet clothing and wrap with blanket Use hot water bottles or packs wrapped in towel Do not warm the person rapidly. It may affect the heart rhythm 12