Chapter 16 Blood
advertisement

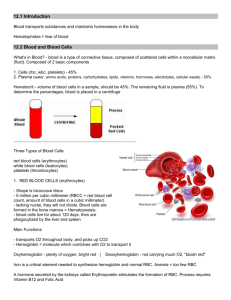
Chapter 16 Blood Objectives: 1. Describe the composition and physical characteristics of whole blood. Explain why is it classified as a connective tissue. 2. List the functions of blood. 3. Discuss the composition and functions of Plasma. 4. Describe the structural characteristics, functions, and production of erythrocytes. 5. Describe the chemical makeup of hemoglobin. 6. List the classes, structural characteristics, and functions of leukocytes. 7. Describe the structure and functions of platelets. 8. Give examples of disorders caused by abnormalities of each of the formed elements. Explain the mechanism of each disorder. 9. Describe the process of hemostasis. List the factors that limit clot formation and prevent undesirable clotting. 10. Give examples of hemostatic disorders. Indicate the cause of each condition. 11. Describe the ABO and Rh blood groups. Explain the basis of transfusion reactions. 12. Explain the importance of blood testing as a diagnostic tool. Whole blood: composed of formed elements (the cellular components) and plasma. Colored scarlet to dark red. pH of 7.35-7.45. 5-6L in males, 4-5L in females. Plasma = 55%, Buffy coat < 1%, RBC’s = 45%. Hematocrit (percentage of RBC’s) in males = 47 + 5%, females 42 + 5%. See figure 16.1 Functions of Blood: 1. Distribution: O2, nutrients, metabolic wastes, hormones 2. Regulation: body temperature, pH (w/ buffers), fluid volume 3. Protection: prevent blood loss (platelets and clotting proteins), prevent and combat infection Plasma: See Table 16.1 90% water, 100 dissolved solutes (table 16.1) such as nutrients, gases, hormones, wastes, products, ions, proteins Plasma proteins: albumin (made by the liver) is the most abundant to maintain osmotic pressure of the blood, others act as shuttles, buffers, clotting proteins, and for immunity (to name a few). Formed Elements 1. Erythrocytes: (see hematocrit). Approx 5 million/ml See figure 16.3 Red blood cells (RBC’s), biconcave discs, anucleate, flexible for travel through capillaries Huge surface area to volume ratio, suited for gas exchange a. hemoglobin: binds easily and reversibly to oxygen (4 globin and 4 heme). See figure 16.4 4 molecules of oxygen per 1 molecule of hemoglobin (Hb) b. hematopoiesis: formation of blood. Erythropoiesis: formation of RBC’s See figure 16.5 occurs in bone marrow, cells arise from pluripotent stem cells Iron (Fe), Vit B12, and Folic Acid necessary Life span 100-120 days; damaged cells (ragged cell membranes) become trapped in spleen, iron is salvaged & stored, rest of heme is degraded to bilirubin (in liver), then secreted in bile to intestines. See figure 16.7 erythropoietin from kidneys stimulates RBC’s due to hypoxia caused by See figure 16.6 i. reduced #’s of RBC’s (hemorrhage or excess RBC destruction) ii. reduced availability of O2 (high altitude or pneumonia) iii. increased tissue demands (aerobic exercise or homeostatic imbalance) c. erythrocyte disorders i. anemia: low oxygen carrying capacity hemorrhagic anemia: blood loss hemolytic anemia: RBC’s lyse (Hb abnormal, transfusion mismatch, ii. parasitic/bacterial infections) aplasic anemia: destruction or inhibition of bone marrow (toxins, drugs, ionizing radiation) decreased hemoglobin content iron deficiency anemia pernicious anemia: lack of Vit B12 abnormal hemoglobin: sickle cell anemia See figure 16.8 iii. polycythemia: too many RBC’s makes blood viscous, sludgy (blood doping) 2. Leukocytes:4000-11,000/ml. See figure 16.9 and Table 16.2 Defense against disease Characteristics include margination (sticking to capillary walls), diapedesis (movement through capillary walls), and chemotaxis (movement toward a chemical). Move by ameboid motion >11,000 WBC’s indicates leukocytosis and a normal homeostatic response to invasion A. granulocytes: contain membrane bound cytoplasmic granules, lobed nuclei, and are primarily phagocytic i. neutrophils: most numerous WBC (Never let monkeys eat bananas), granules contain perioxidases and hydrolytic enzymes attracted to sites of inflammation phagocytic and partial to bacteria ii. eosinophils: attack parasitic worms, lessen severity of alleries iii. basophils contain histamine B. agranulocytes: no granules i. lymphocytes: 2nd most numerous, T and B cells ii. monocytes: largest cells, become macrophages C. leukopoiesis: WBC production from bone marrow See figure 16.11 D. leukocyte disorders i. leukopenia: abnormally low WBC count (drugs and anticancer therapies) ii. leukemia: cancerous condition involving WBC’s; from a single clone iii. infectious mononucleosis: caused by Epstein-Barr virus, excess agranulocytes result Platelets: fragments of megakaryocytes, called thrombocytes, regulated by thrombopoietin See figure 16.12 Hemostasis See figure 16.13 1. Vascular spasm: constriction of damaged blood vessels to reduce blood flow due to direct injury to smooth muscle, chemicals released from endothelial cells and reflexes from pain receptors. 2. Platelet plug formation: when endothelium is damaged, platelets swell and become spiky, get sticky, and attach to collagen. 3. Coagulation: the ultimate reactions are: a. Phase I: prothrombin activator (PA) is formed b. Phase II: PA converts prothrombin to thrombin c. Phase III: Thrombin catalyzes the joining of fibrinogen molecules to a fibrin mesh which traps blood cells and seals holes. Phase I: Intrinsic Pathway Extrinsic Pathway ----- -- “short cut” since tissue factor (TF) is released by damaged cells -- calcium is required -- cascade leads to production of prothrombin activator blood remains in BV collagen exposed platelets cling and release PF 3 cascade of activated clotting factors causes production of prothrombin activator Phase II: PA catalyzes transformation of prothrombin to thrombin Phase III: Thrombin catalyzes fibrinogen to fibrin. Fibrin glues platelets together and makes a web that forms a clot. Plasma becomes gel-like and traps formed elements. Thrombin and calcium activate factor XIII that binds fibrin tightly together. See figure 16.14 Clotting Factors: enhance clot formation. Vitamin K is necessary for synthesis of other clotting factors. Clot Retraction and Repair: platelets pull the clot together (w/ actin and myosin), squeezing out serum. Platelet derived growth factor stimulates rebuilding. Fibrinolysis: the breakdown of the clot that begins within 2 days of clotting. Removes unneeded clots when healing occurs. Factors limiting clot growth or formation swift removal of clotting factors inhibition of activated clotting factors by antithrombin III, protein C and heparin Factors preventing undesirable clotting smooth endothelium antithrombic substances Vitamin E quinine (vit E + oxygen is a potent anticoagulant) Thromboembolytic conditions Thrombus: a clot that develops and persists in an unbroken blood vessel Embolus: a thrombus that breaks away Arterio/Atherosclerosis, severe burns, inflammation Slowflowing blood (bed ridden, long rides) Prevention through aspirin, dicumerol, warfarin (Coumadin) Bleeding disorders Thrombocytopenia: lack of platelets, spontaneous bleeding can occur Impaired liver function: procoagulants not made, lack of Vitamin K can cause Inherited genetic disorders of clotting: hemophiliac Blood Types See figure 16.15 and table 16.4 Due to presence or absence of antigens or agglutinogens, either type A or type B Possible blood types include: Type A, Type B, Type AB, Type O Blood Type Antigen Antibodies A A B B B A AB A,B NONE O NONE A,B Rh factor: an additional antigen found on cells. Rh + : antigen present; Rh - : antigen absent. Hemolytic disease of the newborn can result if an Rh – mother has an Rh + baby, RhoGAM is given to prevent.